You and your oesophageal stent
Information for patients from the Trust's Endoscopy Units
You have been referred for a stent placement. You will have already discussed the reasons for this with your consultant or specialist nurse. This leaflet will help remind you of the information they have given you, including:
explaining what an oesophageal stent is
what happens during and after your procedure, and
what to do if you have any concerns.
If you have any questions or are feeling anxious, please speak to any of the Endoscopy Unit staff.
What is an oesophageal stent?
An oesophageal stent is a flexible, metal tube, knitted from a special type of metal thread.
How is the procedure carried out?
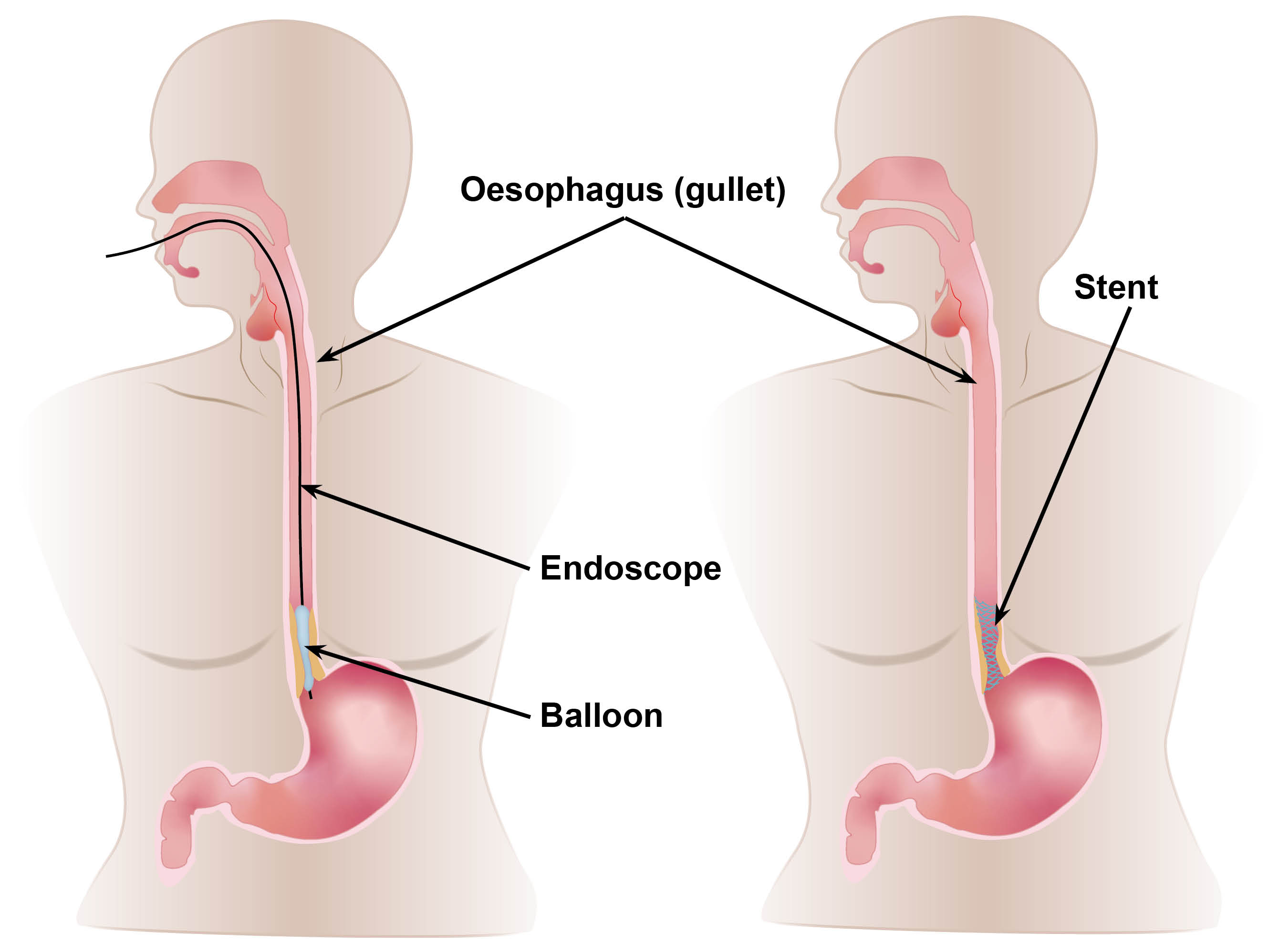
The stent is placed in the narrowed area of your oesophagus (gullet), to help with your swallowing difficulties. This procedure is called an endoscopy.
The endoscope is a long narrow camera, which an endoscopist will pass through your mouth down into your oesophagus. With the help of x-rays the endoscopist will have a clear view of the narrowed area.
To start with, it may be necessary to dilate or stretch the narrowing with a special balloon. The stent is then placed into the narrowed area. Here it will gradually expand and hold itself in place.
How will the stent help me?
When in position, the stent will gently expand to hold the narrowed area open. This will make it easier for food to pass down when you eat.
What happens when I arrive at hospital?
Please report to the Endoscopy Unit reception desk. One of the nurses will collect you and take you to an admission area to prepare you for your procedure.
Will the procedure hurt?
Before your procedure, you will be given sedation and a pain relief injection through a cannula in your hand or arm. This will make you relaxed and drowsy. A nurse will be with you the whole time.
How long will I have to stay in hospital?
You will be in hospital for at least one to two days. During this time, staff will make sure:
any pain from the procedure is controlled
follow-up tests are arranged, and
you know how to look after your stent.
What happens after my procedure?
On the day of your procedure
After your procedure you can rest, as you will feel sleepy. A nurse will check your pulse and blood pressure regularly.
You may feel some pain and discomfort in your chest. If necessary, your nurse will give you injections for the pain and keep you comfortable.
You may have an intravenous (IV) drip to give you fluid.
You may have a chest x-ray to check the position of the stent.
You will not have any food, but your endoscopist may allow you to sip water later in the day.
Day 2
You may be ready to have a very soft diet today, if you are managing to drink fluids. This may include soup, yoghurt, ice cream, runny custard, or jelly.
Day 3
You may be ready for a soft diet. This may include scrambled eggs, steamed fish, omelette, mashed potatoes, mashed bananas, and custard. If you are managing to swallow, you may progress to more solid food. This may include sandwiches with no crusts, soft vegetables, pasta, and rice pudding.
Are there any risks to having this procedure?
Your doctor will explain the risks before your procedure. These may include:
bleeding
perforation of the oesophagus
misplacement of the stent, or
failure to place the stent.
You can discuss these risks with your doctor or nurse before they ask you to sign a consent form.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
Will I need a follow-up appointment?
Your nurse will discuss your follow-up care with you before you leave hospital. You will already have met the upper gastro-intestinal cancer nurse specialist. You will also meet a dietician. Your care will continue under the consultant who arranged your stent placement.
Will I need to change my eating habits?
Your stent will allow food to pass into your stomach through the narrowed gullet, but this may not be as wide as a healthy gullet. You may have to look at changing your eating habits.
Sit upright when you eat.
Never rush your food, take your time.
Always chew your food well. Wear your dentures if you have them. You will have to avoid some foods which can be difficult to chew into small pieces. This includes chunky meat such as steak, tough or stringy vegetables, and soft cheese. These foods have a higher risk of blocking your stent.
Do not swallow chunks of food, they may get stuck and block your stent.
Drink plenty of water with your food. Always have a fizzy drink after each meal; this will help keep your stent clean and prevent blockages.
Try not to eat before going to bed. Prop yourself up in bed with two or three pillows.
Remember that food cannot only pass into your stomach now, it can also come back up into your oesophagus. Stomach acid can also come up and cause heartburn. If this is troublesome, your endoscopist can prescribe medication to help.
What if my stent becomes blocked?
Should your stent become blocked and you have difficulty swallowing, do not panic. Get up and walk around. Try sipping a fizzy drink, this may help dislodge small blockages.
Contact your nearest Emergency Department immediately, if:
the problem does not resolve
you cannot keep fluids down, or
you are regurgitating your food or vomiting.
Contact details
Please phone the Endoscopy Unit. The units are open Monday to Sunday 8am to 6pm.
Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783058Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234370William Harvey Hospital, Ashford
Telephone: 01233 616274
If you have any questions between 6pm and 8am Monday to Sunday, contact the Emergency Department (ED).
ED, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 235030ED, William Harvey Hospital, Ashford
Telephone: 01233 616207
Our units are regularly inspected and audited. Please ask if you want any information about our performance standards. You can also visit the Care Opinion web site.