Trigger finger or thumb
Information for patients from the Hand Therapy Service
This leaflet provides general information about trigger finger or thumb, including:
what a trigger finger or thumb is
what the causes and symptoms are
the treatment options available; and
what happens before and after surgery.
It is not a substitute for your doctor’s advice. We hope it will help to answer some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
What is trigger finger or thumb?
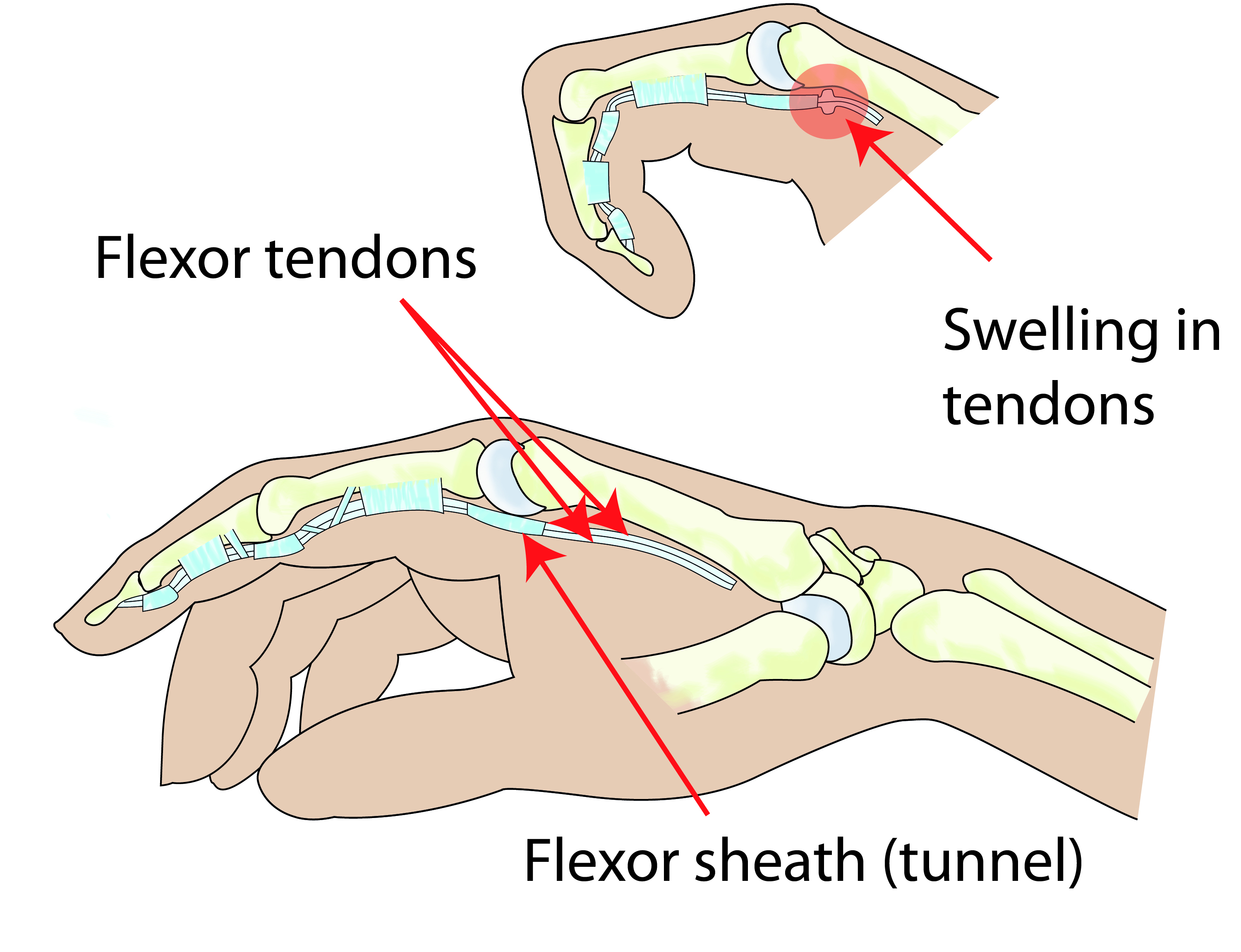
Trigger finger or thumb is the term used to describe the ‘catching’ of a finger or thumb as you bend and straighten it. This is not a serious problem, although it can cause pain in the base of your affected finger or thumb. For most people it is an irritation that interferes with how their hand normally works.
What causes trigger finger or thumb?
We do not know why trigger fingers occur, but it is caused by a thickening around the tendon which bends your finger or thumb. It can develop in any of your fingers, but is more common in your thumb, middle, or ring finger.
It can develop in both men and women at any age, from babies to the elderly. Some conditions, such as diabetes and rheumatoid arthritis, can increase your risk or make the problem worse.
How is the condition diagnosed?
Trigger finger / thumb is usually diagnosed by a doctor or hand therapist. They will look at and feel your hand and painful tendons, looking for clinical indicators such as locking or clicking within your joints.
What are the symptoms?
It may feel like your finger or thumb is clicking or it may catch and stay bent.
Sometimes the only way to straighten your finger is by straightening it with your other hand.
Sometimes it can be sore or painful when direct pressure is placed over the thickening in the palm of your hand.
Do I need treatment for my condition?
If you have mild symptoms, these may clear up on their own, and no treatment is needed. However, treatment can be offered for three reasons.
You are having major problems getting your hand to work properly because of the locking.
Your finger has become stuck and no longer moves at all.
Your finger is very painful.
What are the treatment options available?
If the above points describe your symptoms, there are various types of treatment available to you.
Rest. Avoid activities where you have to use your hand to grip all the time or repeatedly.
Gently massage the base of your sore finger for 5 to 10 minutes. You could also try and help it by rubbing an ice cube over the sore area, to help with the swelling.
Over-the-counter anti-inflammatory tablets or gel. When buying these, please tell your pharmacist about any other drugs you are using. Ask whether these might be affected by the anti-inflammatory tablets or gel.
If your finger is worse overnight or in the morning, the hospital may give you a night splint. This splint will help keep your finger straight and prevent it from locking. Sometimes it helps to have a daytime splint to stop the finger / thumb from locking while you carry out your daily activities.
Exercises
Complete the following exercises every 2 hours, while you are awake.
Repeat each exercise slowly, 5 to 10 times.
Try to avoid locking your thumb or finger as much as possible. This helps to reduce any further thickening around your tendon.
-
.jpg) 1.Gently hook your fingers at the tips, then make a fist.
1.Gently hook your fingers at the tips, then make a fist. -
.jpg) 2.Bend the bottom finger joints as you keep your fingertips straight, then make a fist.
2.Bend the bottom finger joints as you keep your fingertips straight, then make a fist.
Seven out of every 10 patients can be successfully treated with a steroid injection in their finger or palm. For most adults this is recommended as the first line of treatment.
The risk of having an injection is small. Very rarely it can cause some thinning or colour change in the skin at the site of the injection. Your symptoms may improve within a few days of an injection, but may take several weeks. A second injection sometimes helps.
After the above options have been tried, surgery may be needed if the ‘catching’ and pain continue.
What happens before my operation?
You will be asked to attend a pre-assessment clinic.
At this clinic appointment, a nurse will discuss the operation with you.
You may have some tests (such as a blood test).
You will be asked some routine questions about your general health.
Please bring your medicines with you to this appointment; the nurse will need to know their names and the strengths. This includes non-prescription medicines, such as herbal / complimentary medicines.
Please speak to your nurse if you have any questions or concerns regarding your operation.
Depending on the anaesthetic you have, you may need to stop eating and drinking before your surgery. If this is relevant to you, you will be told at your pre-assessment clinic appointment.
Compared to non-smokers, smokers are more likely to have complications in tissue healing and infections after injuries or surgery. If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
What will the surgery involve?
The surgery is usually completed as a day case, so you will be able to go home on the day of your surgery. Local anaesthetic is usually used, so you will be awake for the procedure but the area is numbed.
Before your operation your arm will be painted with a coloured antiseptic to clean your arm and minimise the risk of infection. A band, like a blood pressure cuff, will be placed around your upper arm and inflated to reduce bleeding during surgery; this makes the procedure easier and safer. The band can be a bit uncomfortable.
Surgery for your trigger thumb / finger aims to remove the fibrous tissue, which is stopping your hand from working properly. To do this, your surgeon creates a small incision (cut) in your hand and releases your trigger finger by removing the fibrous tissue.
What happens after my operation?
After your operation you will spend a short time in the recovery area of the operating theatre, before you are taken back to the ward. Your arm will be elevated (raised) either using a sling or a pillow.
How will I feel after my surgery?
You may feel some discomfort in your arm following your surgery. You will be given painkillers before your leave hospital to help with any pain.
If your pain continues, contact your GP to discuss what pain medication to take while you recover from surgery.
What are the risks and possible complications from surgery?
Complications do happen, but with this surgery they are usually mild.
Delayed wound healing or infection. A small number of patients will develop an infection and may need antibiotics or a washout procedure. This occurs in one to two in every 100 cases, and is more common in patients with diabetes.
Common signs of infection are:
yellowish discharge from your wound
very high levels of pain
increased swelling and redness around the site of your surgery (more than expected); and
a bad smell coming from your hand.
If you have a combination of these symptoms, go to your GP and have your wound checked.
Surgery does not work or the condition comes back. This is rare but can happen in a small number of patients.
Your scar may be tender for a number of months. If it does not improve with time and regular scar massage, a course of therapy may help. One in every 1000 people are sensitive to hand surgery, leading to long-term scar tenderness.
Stiffness may develop, particularly in your fingers. This is usually short-term and only occasionally needs hand therapy. It is important that this is dealt with quite quickly though (within three months), to avoid permanent stiffness.
Nerve damage can happen during your surgery. This may result in either a painful spot in your scar (neuroma) or some numbness around your scar.
Complex Regional Pain Syndrome (CRPS) is a rare but serious complication. The happens when the nerves in your hand “over-react”, causing swelling, pain, discolouration, and stiffness and normally needs therapy to try to settle this. More information is available in the Complex Regional Pain Syndrome (CRPS) leaflet.
Please remember that most patients have an uncomplicated routine operation with very satisfactory recovery and outcome.
How do I look after my hand following surgery?
You need to look after your hand following surgery to help it to heal properly.
To start with, this involves making your hand comfortable and keeping it elevated (raised). Keep your hand elevated as much as possible, to reduce the swelling. Use your arm gently within the limits of your bandage, avoiding pressure over the site of your surgery.
Your wound can take 10 to 14 days to heal. During this time you can use your hand, but only to do light activities, such as holding a phone, using a knife or fork, and writing. Moving your fingers will help with your recovery.
The anaesthetic can stay in your system for up to 72 hours. Do not be alarmed if your hand is numb during this time. Contact your surgeon if this does not stop after 72 hours. The contact details for your surgeon’s secretary should be on your appointment letter.
You will have a bandage on your hand following surgery. You can remove this after 72 hours, which will leave a small sticky dressing beneath. Please do not get this bandage or plaster wet until it is all removed.
You will have dissolvable stitches or ones which will need to be removed between 10 to 14 days after surgery, either by your GP or consultant. This will be explained to you before you leave hospital.
Will I need a follow-up appointment?
You may not need a follow-up appointment. If your consultant would like you to see you again, they will organise this for you.
Hand therapy after surgery is not usually necessary.
What size scar will I have and how many stitches will I have?
The length of your scar will depend on the number of fingers affected by your condition. The number of stitches also varies, but we aim to make the scar as small as possible.
How soon after surgery can I drive?
Do not drive home following your surgery. If possible arrange for someone to collect you.
You can start driving as soon as you feel confident enough to control your car safely, including completing an emergency stop. This is usually 1 to 2 weeks after your surgery.
When can I return to work?
This varies, depending on what job you do. Please discuss this with you GP or consultant.
If you are in a supervisory or managerial role, that does not need the full use of your hand, you could return to work within a few days of surgery. Other light manual jobs may need two to three weeks off work. Heavy manual jobs may need you to be off work for a few weeks longer.
What if I have any questions or concerns?
If you have any questions or concerns regarding your treatment, please call the Hand Therapy Service on 01227 783065.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email