Treatment for bladder tumours (transurethral resection of bladder tumours (TURBT))
Information for patients from the Urology Department
You have had an examination that has shown that you have an abnormal area (tumour or cancer) in your bladder. Your consultant has recommended that you have a transurethral resection of these bladder tumour(s). This treatment will allow your consultant to investigate the type of tumour(s) you have and how to treat them.
This leaflet explains the benefits, risks, and alternatives to the procedure. It also outlines what you can expect when you come into hospital. If you have any questions, please speak to your nurse, who will be happy to help you.
How does the bladder work?
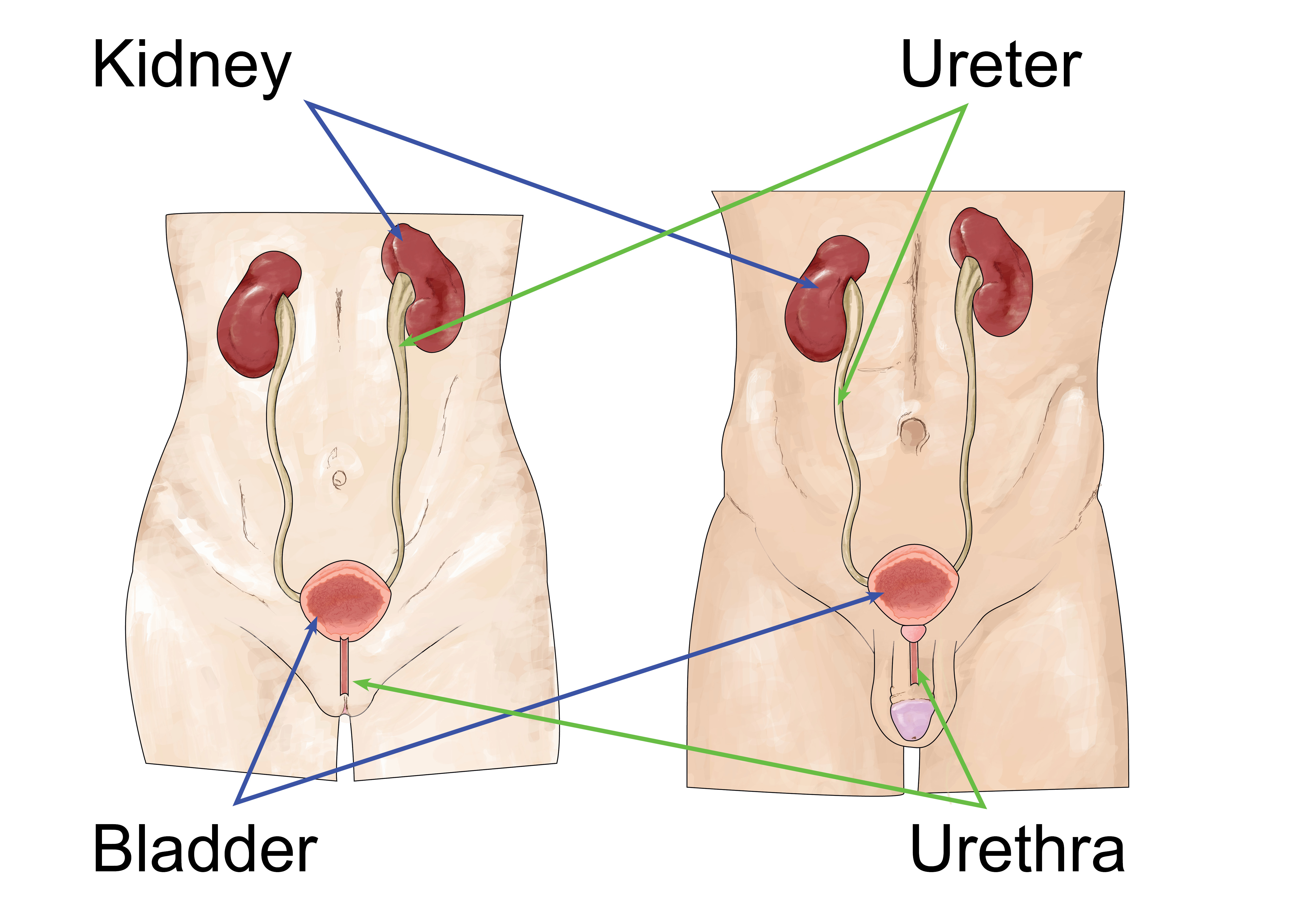
Your bladder is located in the lower part of your abdomen. It has two main functions, the storage and emptying of urine.
Urine is the waste fluid produced by your kidneys when they clean your blood. The urine then travels down the ureters from your kidneys and into your bladder. As your bladder fills with urine, the detrusor muscle allows it to expand, like a balloon.
When your bladder is full, you get the urge to pass urine (urinate). The urine then leaves your bladder and travels through your urethra. The urethra is the tube that carries urine to the outside of your body.
Men have a prostate gland that sits at the base of their bladder.
What is a transurethral resection of a bladder tumour (TURBT)?
A tumour is an abnormal growth. It can be benign (not cancer) or malignant (cancer). A TURBT is a treatment for bladder tumours.
During a TURBT, the tumour(s) is cut away from the bladder wall, removed and then sent for examination. From this, your consultant will be able to find out whether the tumour cells are cancerous. If they are, the examination will show what grade and stage the cancer has reached. Using this information, your consultant can then decide what treatment you may need.
Why do I need this procedure?
A TURBT is the standard treatment for bladder tumours.
Benign bladder tumours usually grow very slowly. However, if they are not treated, they could become very large. This can cause problems, as they take up too much space in your bladder or begin to press on other organs in your body.
Malignant tumours continue to grow unless they are removed. They can invade surrounding tissue and spread to other areas of your body. This can cause further problems.
What are the symptoms of bladder cancer?
Bladder cancer occurs most commonly in people aged between 50 and 70 years old. In the UK, it is the fourth most common cancer in men and eighth most common cancer in women.
The most common symptom of bladder cancer is blood in your urine (haematuria).
You may also have symptoms similar to having a urine infection. For example you may have pain when you pass urine, and the urge to pass urine more often than usual.
What causes bladder cancer?
The exact causes of bladder cancer are not known. However, you are more likely to develop bladder cancer if you:
Smoke. Chemicals in tobacco enter the bloodstream and are then filtered out by the kidneys. It is thought that these can cause damage to the bladder lining, which can lead to bladder cancer.
Have a history of bladder cancer in your family.
Have worked in the dye, chemical, or print industry. Certain chemicals used in these industries have been banned, as they are now known to cause cancer.
Have repeated bladder infections, for example cystitis.
Have had bladder cancer before.
Have developed a bladder infection called schistosomiasis. This is caused by a parasite found in certain tropical countries.
What are the alternatives to TURBT?
If possible, bladder tumours will always be removed by surgery. If there is a recurrence of a malignant tumour, we may offer chemotherapy or immunotherapy as a treatment. But a TURBT is the first treatment offered for all bladder tumours.
What are the risks?
Although serious complications are rare, every surgery has risks. The risks of having a TURBT include the following.
Blood in your urine; this is common, and most people experience this.
A mild burning sensation when passing urine. This can last for a few days, but it is not uncommon for it to last several weeks. You should drink plenty of water to keep hydrated and flush your system, at least two litres per day.
Infection can happen occasionally. Please see your GP if you think you may have a urine infection.
Perforation of your bladder is very rare. If this happens you will need a temporary urinary catheter or open surgical repair.
Difficulty in passing urine straight after your operation, once the catheter is removed. If this happens you may need to have a catheter re-inserted and go home with this for a period of time.
Deep vein thrombosis (DVT) is a blood clot, usually in the large leg veins. You will be given anti-embolism stockings before your surgery, and you should start moving around as soon as possible after surgery.
Urine incontinence (the unintentional passing of urine) following surgery. This can be urgency incontinence, when urine leaks as you feel a sudden, intense urge to pee. Or frequency incontinence, when you are unable to fully empty your bladder, which causes frequent leaking.
Latex allergy, as some catheters are made from latex.
Will I have an anaesthetic?
Yes. You will have this operation under either:
a general anaesthetic (you are asleep for the procedure), or
a spinal anaesthetic (you will be awake but numb from the waist down).
This will be discussed with you before your surgery.
How long will I be in hospital?
How long your operation takes will depend on the size of your tumour.
You will usually be able to go home about one to two days after surgery. This will depend on how difficult your resection was.
What happens before my operation?
You will come to hospital for a pre-anaesthetic check before your surgery (preassessment). At this appointment a nurse will check your blood pressure, weight, and medications. They will also take blood and urine samples, and carry out heart tracing and x-rays, if necessary.
Please remember to bring a list of all your medication to this appointment. Bring this list when you come into hospital for your surgery as well.
If you are taking any blood-thinning medication (for example aspirin, warfarin, or clopidogrel), you may need to stop taking these before your surgery. Staff will discuss this with you at your preassessment appointment.
You will not be able to eat or drink before your surgery. Staff will give you instructions about this at your preassessment appointment.
Your consultant or registrar will see you before your operation. They will discuss your surgery, and ask for your written consent to continue. Please ask any questions that you may still have. We want to involve you in decisions about your care and treatment.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
What happens during TURBT surgery?
This operation is performed through a special telescope (a cystoscope / resectoscope). This telescope is passed up into your urethra (water pipe).
-
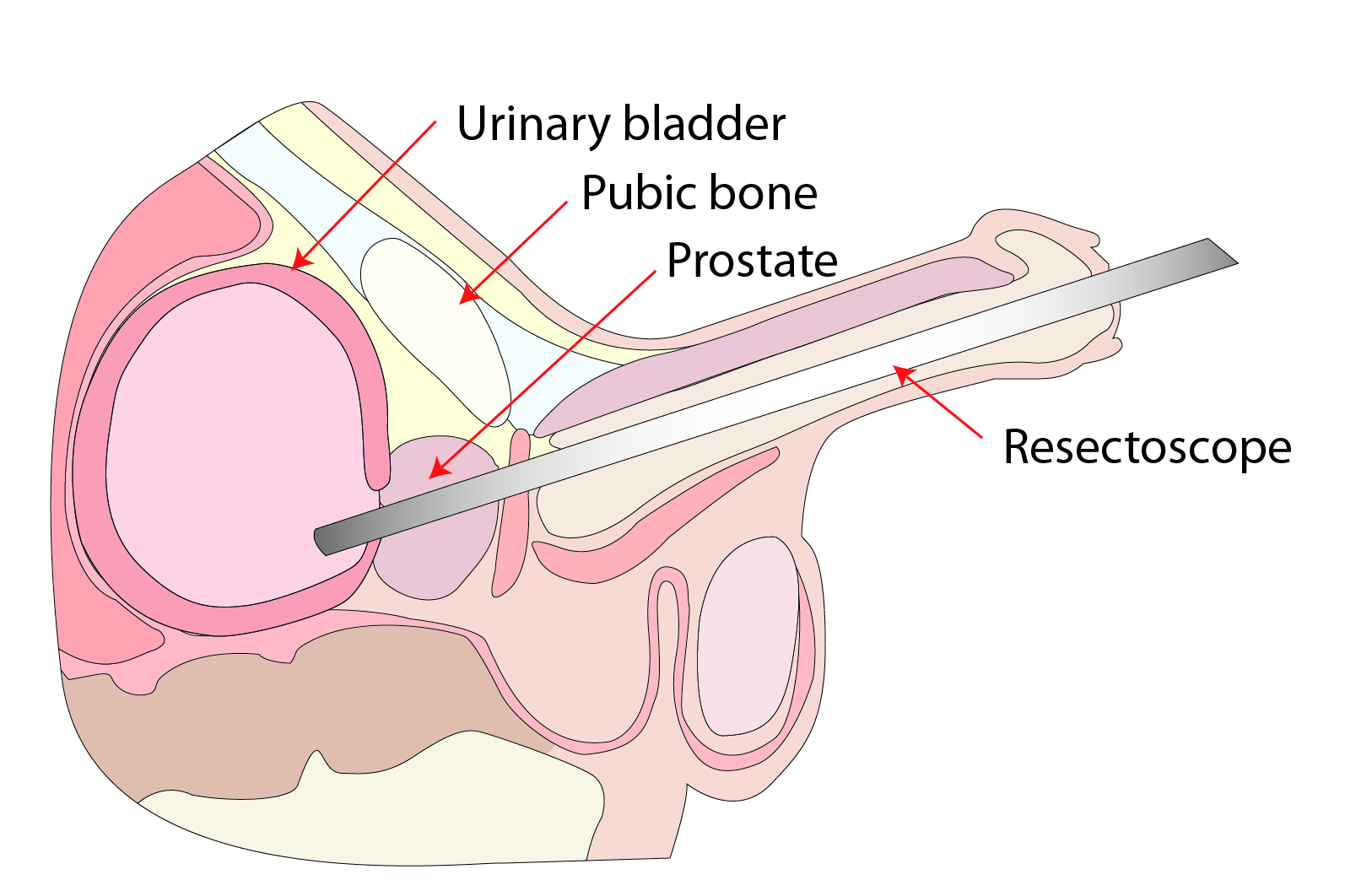 Resectoscope being passed up into the male urethra
Resectoscope being passed up into the male urethra -
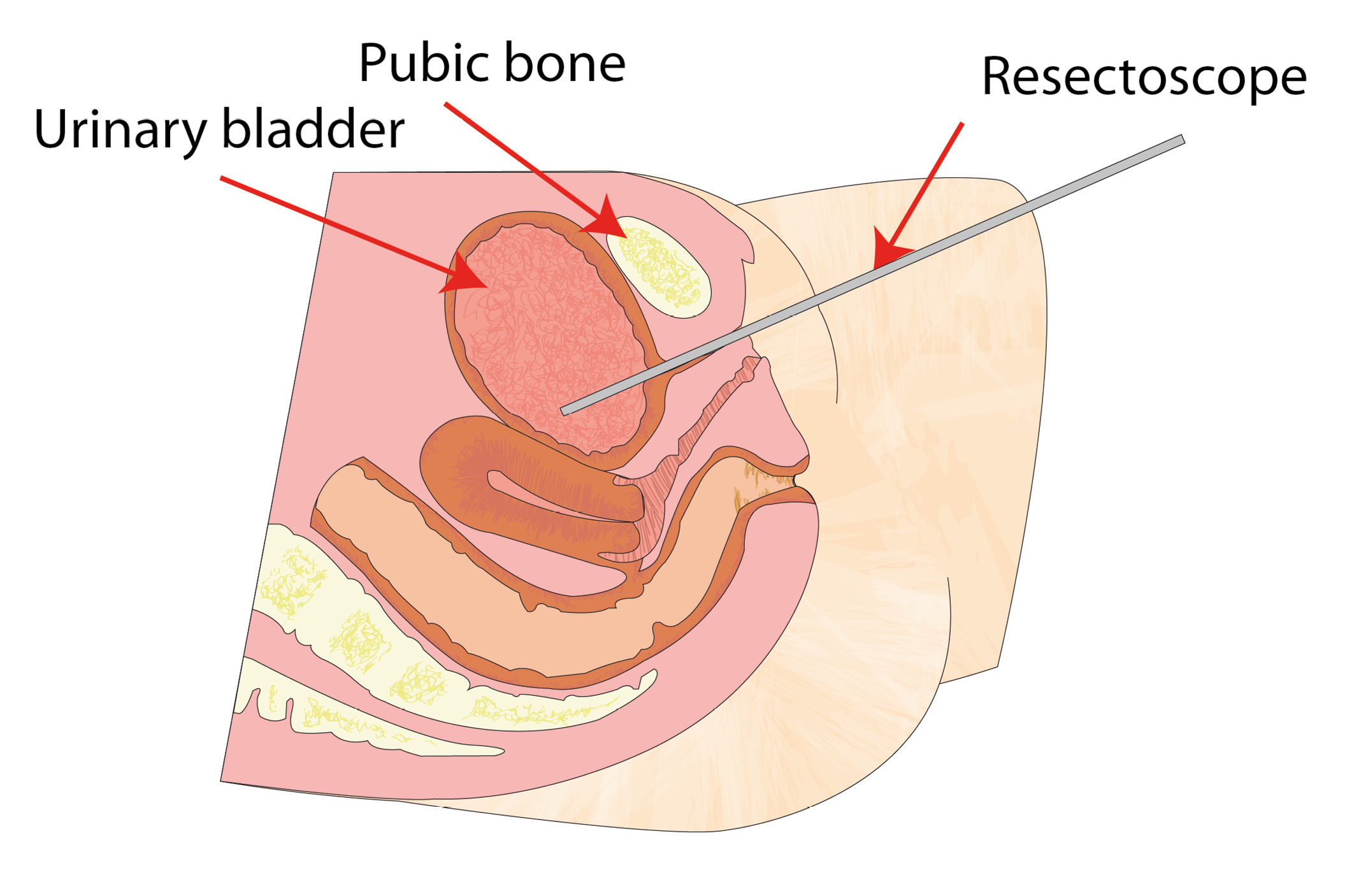 Resectoscope being passed up into the female urethra
Resectoscope being passed up into the female urethra
No incision (cut) is made on the outside of your body.
With an electrical cutting device, the cystoscope will shave down and remove the tumour or growth in your bladder.
Once the cystoscope has been removed, a tube called a catheter is passed up into your bladder. This will allow urine to be drained. Sterile irrigation fluid is often used to make sure that the catheter does not block and urine can drain out. This fluid is given through a channel on the urinary catheter. The catheter remains in place until your urine is clear, usually overnight.
You may be given a chemotherapy bladder instillation following surgery called Mitomycin. This will treat any stray cells that may still be in your bladder following surgery.
Why do I need a catheter?
A catheter will be inserted during your surgery. It is usually left in place after surgery to help to drain your bladder, as there will be some bleeding following surgery. your urine will be discoloured and bloodstained. The bleeding usually settles down in two to three days. Although you can expect to see some blood in your urine for several weeks.
The catheter may also by-pass. This means that blood or urine passes around the outside of the catheter. This is due to bladder irritation, which then leads to involuntary bladder contractions. This can also happen if you strain when you open your bowels.
You can use soap and water to clean the area and the end of the catheter.
Note: it is sometimes necessary to go home with a urinary catheter for a few days or weeks. This is to allow your bladder to heal, or if you are unable to pass urine after the catheter is removed following surgery. If this happens to you, a member of staff will show you how to care for your catheter before you leave the hospital. You will also be given a date to return to the hospital to have it removed.
Will the procedure hurt?
The operation is not normally painful. You may have some discomfort afterwards, especially from the catheter. This is known as bladder-spasm and is due to the muscle continuing to contract on occasions. Simple painkillers, such as paracetamol, should help with this.
Can I eat and drink as normal after surgery?
Despite the frequent and urgent need to pass urine following surgery, you should increase the amount you drink in the first few weeks. Drinking less does not always stop the sensation or need to pass urine, and can often make this worse. We recommend you drink around two litres of fluid every day.
Eat as normal, including all food groups. We recommend avoiding drinks and fluids that may irritate your bladder. These include caffeine, carbonated (fizzy) drinks, alcohol, and spicy foods.
Please avoid constipation. Increase the amount of fibre in your diet or take a mild laxative if you feel this is needed.
I’m bleeding after my surgery, is this normal?
It is not uncommon to have blood in your urine for a few days after your surgery.
Often 10 to 14 days after the operation secondary bleeding can start. This is normal, and can be due to healing and is when areas of the bladder wall shed from the operation site. You will be able to see this when you pass urine. Usually the discharge is a dark brown colour. Increasing the amount of fluid you drink will help flush this through.
If the bleeding is very heavy, persistent, contains fresh blood, or it becomes difficult to pass urine, please contact the ward or the specialist nursing team.
What should I do if I develop an infection?
Some patients do develop a urine infection after surgery. Symptoms include an increase in the burning sensation, bleeding, or increased frequency of passing urine. If you have any of these symptoms, please ask your GP for advice.
When can I go back to my normal activities?
Speak to your doctor about how much time you will need off work after your operation. This will depend on how you recover and the type of work that you do. Usually you will need to take about two weeks off. However, if your job involves lifting or heavy work, you may need to take three to four weeks off work.
We suggest that you start gentle exercises straight away. Although we advise you not to do anything too energetic, such as playing contact sports, for around a month.
Do not carry or lift heavy items for at least two weeks. Heavy lifting would include moving or lifting lawnmowers or heavy bags of shopping.
Although you cannot see your scar, you need time for things to heal internally. By four weeks you should have returned to your normal activities, unless advised otherwise.
When can I drive again?
Do not drive for at least one week after your surgery, or until you feel comfortable. Please check with your insurance company before driving again.
When can I have sex again?
You can have sex when you feel able, but it may be wise to avoid it for around two weeks.
What if I have problems at home?
Some people have a mild burning sensation when passing urine. They also feel the need to pass urine more often and more urgently after their surgery. This is due to irritation to the nerves and the bladder-lining. This usually settles after a few days. However in some cases this can last for several weeks, and patients can sometimes see blood when they pass urine.
If during the first two weeks after surgery you have any of the following , you should contact the ward, your specialist nurse, or your GP.
Develop a temperature (over 38°C), have pain, and persistent burning when you pass urine.
Do not pass urine for a period of time, leading to pain and discomfort. This may mean you are retaining urine.
Pass large clots of blood.
Have continued bleeding.
When will I receive my results? Will I have a follow-up appointment?
Your results should be available 2 to 4 weeks after your operation.
At your follow-up appointment, your doctor will review your results with you and discuss your future care. Please make sure you know the time and date of this appointment before you leave hospital.
The results from your TURBT will determine your future care.
If you had bladder cancer and your tumour was removed, you will need to have regular cystoscopies to check the cancer has not returned. To start with these will be every three months, but this will become less often if your bladder remains cancer free.
If you need further treatment, due to the type of cancer found, your consultant will discuss this with you at your follow-up clinic appointment.
What if I have any questions or concerns?
If you have any questions about your condition or treatment, or concerns when you return home, please call one of the following.
Clarke Ward, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783103Bladder Cancer Specialist Nurse
Provides support and advice regarding your diagnosis and ongoing treatment.
Telephone: 01227 868666
Further information
Macmillan Cancer Support provides information and support to anyone affected by cancer.
Telephone: 0808 808 0000Cancer Research UK provides information on all types of cancer and treatment options, as well as a book list for further information.
Telephone: 0808 800 4040Action Bladder Cancer UK provides information and support to anyone affected by bladder cancer.
Fight Bladder Cancer
Telephone: 01844 351621