Tonsillectomy
Information for patients from the Ear Nose and Throat (ENT) Department
You have been referred to the hospital for a tonsillectomy. This leaflet explains the following:
What the tonsils are
What the alternatives to surgery are
What happens before, during and after surgery
What the risks are to having surgery.
If you have any questions after reading this leaflet, please speak to your doctor.
What are tonsils?
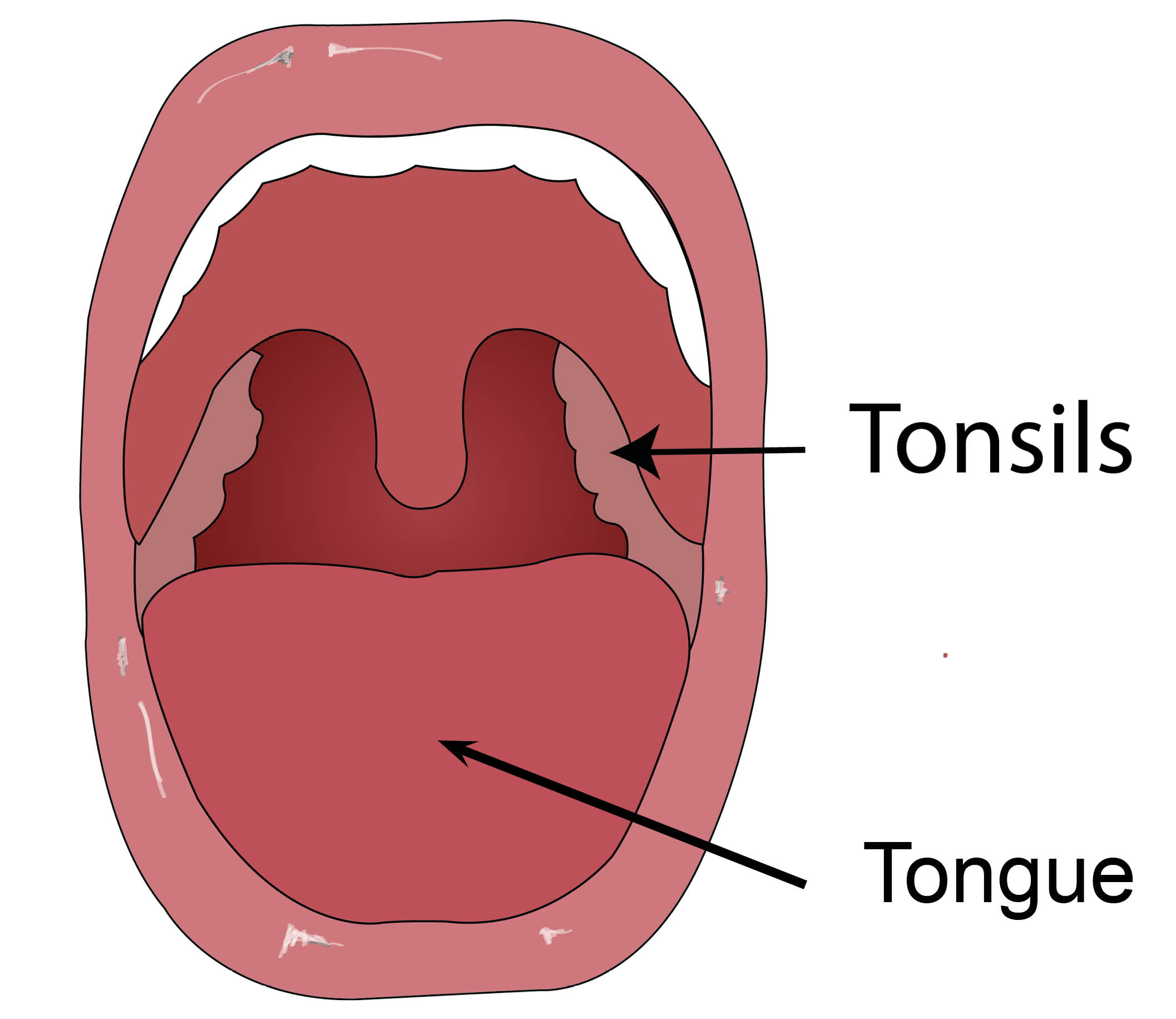
Tonsils are often thought to be the tissue at the back of your throat, however you also have tonsils at the back of your nose (the adenoids) and your tongue. They are all part of the body’s immune system, helping to fight infection.
Tonsils usually grow during childhood. They shrink in adulthood, as they become less important in fighting infections. Your body can still fight infections if the tonsils in your throat are removed.
What is tonsillitis?
Tonsillitis is an infection of the tonsils, caused by a virus or bacteria. It can affect anyone. Symptoms include:
sore throat
fever
bad breath
painful swallowing; and
swollen neck glands.
Your tonsils will look red and swollen, and you may be able to see white spots on their surface. These symptoms usually last for 3 to 4 days, but can carry on for up to 2 weeks.
Treatment is usually painkillers and rest. Severe cases of bacterial infection may need antibiotics.
What is a tonsillectomy?
A tonsillectomy is surgery to remove the tonsils at the back of the throat.
When will I need to have a tonsillectomy?
Tonsil removal is often done to stop you repeatedly getting tonsillitis. If tonsillitis keeps recurring it can cause absences from school or work.
In young children, doctors may recommend removing the tonsils if the child has:
a history of febrile seizures from tonsillitis; or
breathing problems at night due to enlarged tonsils.
Though rare, tonsillar tissue may grow back. This could need more surgery, if it causes repeated infections.
What is a tonsillotomy?
Your doctor may suggest you have a coblation tonsillotomy. This is a surgical technique that may cause less pain and bleeding than a traditional tonsillectomy.
During this procedure, we melt down the tonsils until little or no visible tissue remains. Doctors may offer this treatment to young children, to reduce the risks of having an operation.
Is surgery the only option?
The alternative to surgery is to manage your symptoms by treating tonsillitis with painkillers and antibiotics. Track your progress over time, and see if this helps and you have less episodes of tonsillitis.
To help reduce infections:
Eat a balanced diet and exercise.
Do not smoke or expose children to passive smoking.
Brush your teeth and gargle with salt water to keep your mouth clean.
What are the risks to having surgery?
The main risks of the procedure are as follows.
Pain. Your throat will feel very sore for up to 2 weeks following surgery; pain will peak around day 4 to 5. For more information on controlling your pain, see What pain relief should I take after my tonsillectomy? below.
Bleeding can occur any time from the day of your tonsillectomy to 2 weeks after. If you spit out any bright or dark red blood or clots, please go to your nearest Emergency Department. Even a small amount could cause a larger bleed. Most bleeds stop with observation and antibiotics. Severe cases may need surgery or a blood transfusion. Please speak to your surgeon if you cannot have a blood transfusion.
Infection. A fever is common in the first 24 to 48 hours after your operation. However, if it does not settle, it could be a sign of infection and you may need antibiotics. Please see your GP or go to your nearest Emergency Department if you have any concerns.
Damage to teeth, lips, and gums. The instrument used to keep your mouth open during surgery rests on your teeth. Rarely, this can damage your teeth, lips, and gums. Please tell your surgeon if you have any loose teeth.
Complications of a general anaesthetic. Your anaesthetist will explain the risks of a general anaesthetic on the day of your operation. More information on anaesthesia is available in the You and your anaesthetic leaflet.
What will my throat look like after my operation?
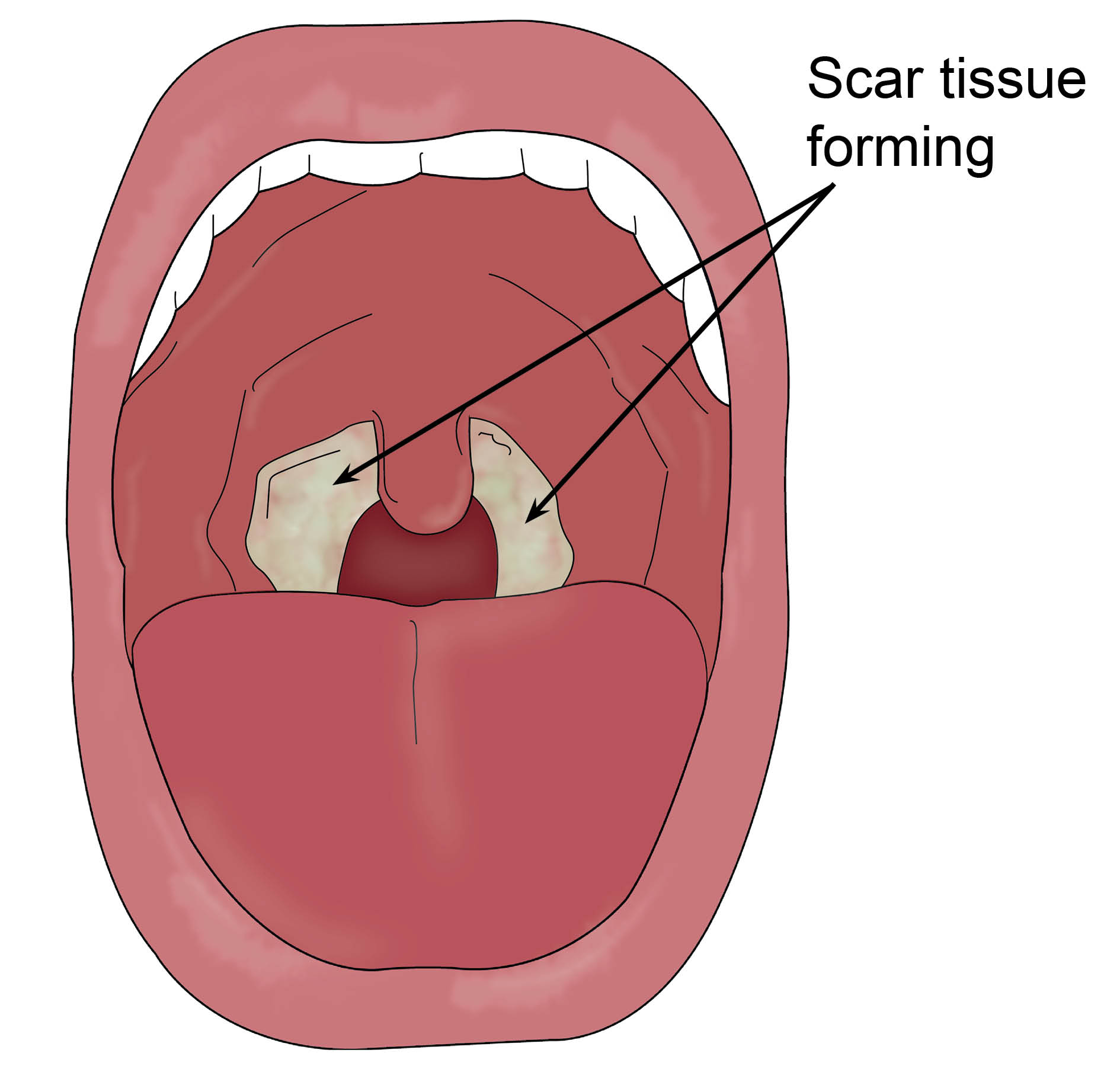
You will notice a whitish-yellow coating at the back of your throat after your operation. This is completely normal, and is scar tissue forming. It is not a sign of an infection, and you do not need antibiotics. This may cause you to have bad breath.
You may also see some black stitches at the back of your throat. These will come away on their own within 14 days; swallowing them is harmless.
What should I do before I arrive at the hospital?
If you smoke, you should quit. Smokers are more likely to have complications after their operation. If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
Take 2 weeks off work or school. Do not plan anything important for 2 weeks after your surgery.
Make sure you have plenty of paracetamol and ibuprofen at home. Take these every day for at least 7 days after your operation.
Bring into hospital any other medication you are taking. These will be locked in a cupboard by your bed, and used as needed. Please remember to take these home when you leave.
If you have tonsillitis, a cold, or flu in the 2 weeks before your surgery, please telephone the Preadmission Nursing Team for advice. Your operation may need to be postponed due to the higher risk of bleeding.
Preadmission Nursing Team, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783114Preadmission Nursing Team, Queen Elizabeth the Queen Mother (QEM) Hospital, Margate
Telephone: 01843 234458Preadmission Nursing Team, William Harvey Hospital, Ashford
Telephone: 01233 616743
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
What happens when I arrive at hospital?
Your appointment letter will tell you where you need to report to when you arrive at hospital.
A member of the nursing team will greet you and guide you to your bed area or cubicle. They will help you with the paperwork and discuss your hospital care. The nurse will ask you questions about your general health. Your surgeon and anaesthetist will ask similar questions.
The nurse will record your blood pressure, temperature, and pulse, and prepare you for surgery.
Before surgery, your doctor may prescribe a tablet or injection to help you relax.
Your surgeon will explain your operation again and ask you to sign a consent form.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
Will I have an anaesthetic?
Yes. You will have a general anaesthetic, so you will be asleep during surgery. You will see an anaesthetic doctor before your surgery. They will explain the anaesthesia and outline the risks. Please use this time to ask any questions.
What happens during my operation?
When you are fully anaesthetised, the anaesthetic team will take you into the operating theatre.
Your anaesthetist will choose a way of making sure that oxygen and gases can move in and out of your lungs easily. Usually this means a tube is placed in your airway. There are different types of tube for different circumstances. Your anaesthetist will talk you through this all. For more information, please read the Royal College of Anaesthetists You and your anaesthetic leaflet.
A special instrument holds your mouth open while you are asleep. Surgeons remove your tonsils through your mouth, without making an external cut.
Any excessive bleeding is controlled by a combination of:
pressure swabs
diathermy (electric cautery)
stitches; or
radiofrequency electrical current (coblation).
How long will I have to stay in hospital?
You will usually go home on the same day as your surgery or the day after. You will need to stay in hospital for 3 to 6 hours after your surgery.
If you are discharged home on the day of your operation, please make sure that you arrange for a responsible adult to stay with you for the first 24 hours.
What pain relief should I take after my tonsillectomy?
Not controlling your pain increases your risk of serious complications, including infections and bleeding.
Even if you feel a small amount of pain in the first few days after your operation, take regular paracetamol and ibuprofen. This will help keep your pain under control.
Pain will get worse around day 4 or 5. If pain is not controlled at this point, you may find it hard to swallow your medicine. This pain usually goes away within 10 days.
Eating and drinking as normally as possible reduces your chance of infection and bleeding.
Pain relief and children. How much paracetamol and ibuprofen you give your child should be based on their weight, not their age. Your child's discharge letter will tell you what dose to give them. Please give this amount to your child, even if it differs from the dosage on the medication bottle (which is based on your child’s age).
The doctor may also send you home with a throat spray and a small dose of morphine. Use these medicines if you need more pain relief on top of your regular paracetamol and ibuprofen. Adults will be given a laxative to prevent constipation from the morphine.
Please discard any unused medication at the end of 2 weeks.
Can I eat and drink when I return home?
You will start eating and drinking as soon as you are awake after your surgery.
It is very important to eat and drink regularly. Stick to a normal diet, including rough, chewy foods such as crisps and toast. This will help you heal and reduce your risk of bleeding and infection.
To help you eat and drink, take your painkillers and throat spray 30 minutes before meals.
Avoid hot drinks on the day of your surgery.
What should I do if I have any concerns or questions?
If you have any queries or concerns, please contact Rotary Outpatients or Day Surgery on the numbers below, or phone your GP.
Canterbury Day Surgery Centre, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783114 (7am to 8pm)Day Surgery, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234499 (Monday to Friday 7am to 9pm)
Telephone: 07887 651162 (Monday to Friday 9pm to 7am) (Bank Holidays and weekends, 24 hours a day)Channel Day Surgery, William Harvey Hospital, Ashford
Telephone: 01233 616263 (24 hours a day, 7 days a week)Rotary Ear Nose and Throat (ENT) Outpatients, William Harvey Hospital, Ashford
Telephone: 01233 616261 (Monday to Friday 9am to 5pm, Saturday and Sunday 9am to 3pm)
Further information
[Websites last accessed 21 January 2026]
References
[Websites last accessed 21 January 2026]
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email