Third- and fourth-degree perineal tear during childbirth
Information for women, birthing people and their families
You have had a third- or fourth-degree perineal tear during childbirth. This is also known as an obstetric anal sphincter injury (OASI). This leaflet will explain:
what this type of injury is
how to care for your injury
why it is important to make sure your bowel and bladder are working well
why and how to do pelvic floor exercises; and
what follow-up appointments you will have in the next 12 weeks.
If you have any questions after reading this leaflet, or you need further support, please speak to your midwife.
What is an obstetric anal sphincter injury (OASI)?
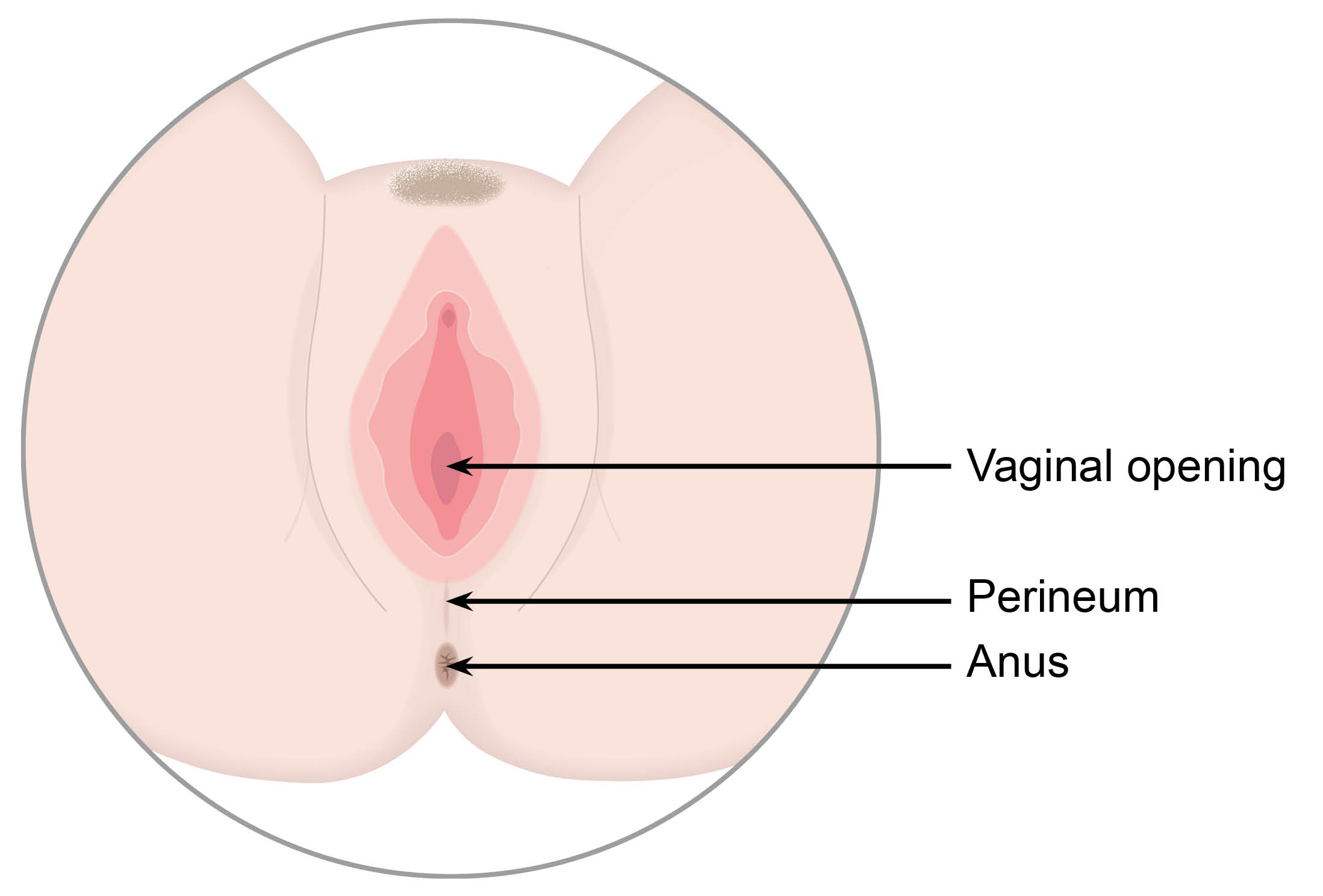
An obstetric anal sphincter injury (OASI) is also known as a third- or fourth-degree tear. This type of tear can extend down from the vaginal wall, and backwards through the perineum, to the muscle that controls your back passage (anal sphincter). Your perineum is the area between your vaginal opening and your anus.
How common are third- and fourth-degree tears?
Most women or birthing people will have a tear of some kind during birth. These tears are usually minor, and some do not even need stitches.
Third- and fourth-degree tears occur in about 3 out of 100 vaginal births.
It is more common with a first-time vaginal birth, occurring in 6 in 100 women or birthing people. This is compared with 2 in 100 women or birthing people who have already had a vaginal birth.
What type of tear do I have?
Many women or birthing people experience tears during childbirth. Tears can occur as the baby stretches the vagina and perineum during birth. The following are the types of tears that can occur.
.jpg)
Perineal tear
Small, skin-deep tears are known as first-degree tears and usually heal on their own. Tears that are deeper and affect the muscle of the perineum are known as second-degree tears. These commonly need stitches. More information on first- and second-degree tears is available in our Perineal Tear Advice Sheet.
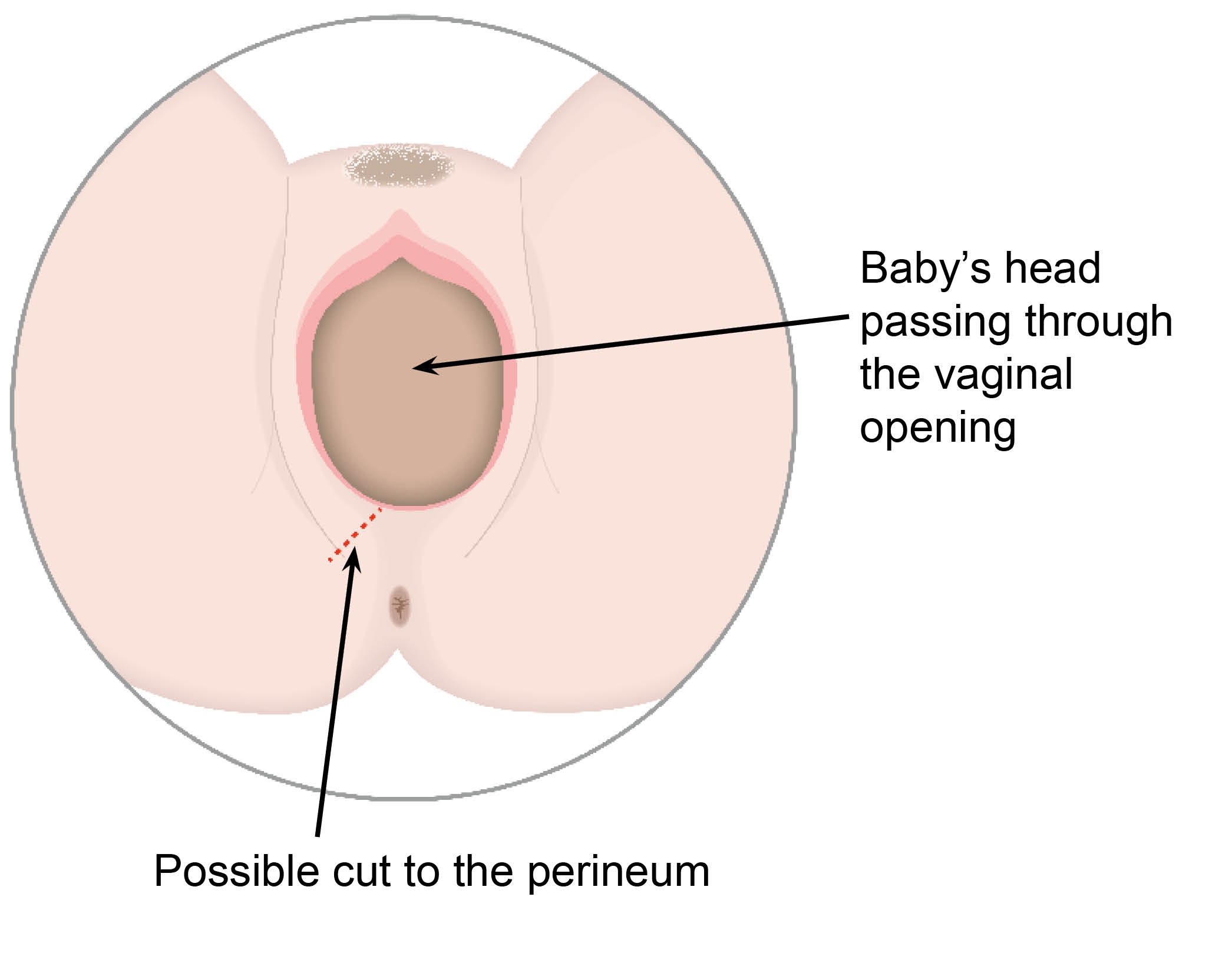
Episiotomy
An episiotomy is a cut made by a midwife or doctor in the area between the vagina and anus (perineum). An episiotomy makes the opening of the vagina a bit wider, allowing the baby to come through it more easily. This may be done if:
your baby needs to be born more quickly
to make more space for your baby to be born; or
if there is a risk of a tear to your anus.
It is possible for an episiotomy to extend and become a deeper tear. If your doctor or midwife feels you need an episiotomy when you are in labour, they will discuss this with you.
.jpg)
Third- and fourth- degree tears
A third-degree tear is a tear that extends into the muscle that controls the anus (the anal sphincter). If the tear extends further into the lining of the anus or rectum it is a fourth-degree tear.
Rectal buttonhole
This is a rare injury. It occurs when the anal sphincter (or muscle) is not torn, but there is a hole between the back passage and the vagina. This means that wind and faeces (poo) may be passed through the vagina instead of through the anus. This is not normal. If you have this you should see your healthcare professional urgently.
If you have had a tear during the birth of your baby, your midwife or doctor will explain which of the above applies to you. If you have any questions, please speak to them.
What happens if I have a third- or fourth-degree tear?
This type of tear will need to be repaired in theatre, as soon as possible after your baby is born.
If your midwife or doctor suspects that you have a rectal buttonhole, this will also need to be repaired in theatre.
These tears will not heal well without being repaired in theatre.
What happens before surgery?
Your doctor will discuss the procedure with you, and ask for your consent. They will answer any questions you may have.
You will have an epidural or a spinal anaesthetic before your operation. This will mean that the area is numb, and you will be awake during the operation. An anaesthetist will discuss this with you before your operation. Please ask them any questions you may have.
A general anaesthetic may be needed (this is where you are asleep for the procedure), but this is rare. You will have a canula (small plastic tube) placed into a vein in your arm before the procedure begins.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
What happens after surgery?
You may need IV (intravenous) fluids. If you are given these, the anaesthetist will explain why. These will be given through a drip into the canula in your arm.
An epidural or spinal anaesthetic means you will need a catheter (a soft tube) in your bladder. This will be inserted after the spinal anaesthetic or at the end of surgery. It will drain your urine, as you will not be able to feel when you need to wee. The catheter is usually kept in for 12 hours to fully allow feeling to return to your bladder. It will be removed by a midwife or maternity care assistant.
Your urine will be measured when you go to the toilet, to make sure your bladder is fully working. Two measurements of 200mls or more of urine tells us your bladder is working well.
It is unlikely you will go home with the catheter. However, you may need to go home with a catheter and return after 7 days to have it removed if you are unable to:
pass urine, or
empty all the urine from your bladder (urinary retention).
After your operation you will be given pain relief, such as paracetamol and ibuprofen. Please ask for stronger pain relief if you need it.
You will be given a course of antibiotics, to help reduce your risk of infection. For them to work, you must take the full course of antibiotics.
You will be given laxatives. These will make it easier and more comfortable to open your bowels (have a poo), and reduce any straining whilst sitting on the toilet.
How long will I stay in hospital after my operation?
You will need to keep the catheter in for at least 12 hours. After this we need to make sure you are able to wee without issues. Once you have passed over 200mls of urine twice, you may be able to go home.
You may also need to have a blood test and wait for your results.
You should not have to stay in hospital for an extended time unless there are any other complications, or you do not feel ready to leave. Rarely, another operation may be needed to repair your tear.
If you have questions on how your tear is healing, please speak to the OASI lead midwife, your midwife, or your doctor. The contact details for the OASI lead midwife are at the end of this leaflet.
Will anyone check my stitches when I go home?
Your community midwife will check your perineum and stitches when they see you after your discharge from hospital. They will make sure you are healing well before you are discharged from Maternity's care. If you have any concerns or questions about your stitches or healing, please talk to your community midwife.
How do I care for my wound and stitches?
You will have stitches between your vagina and your anus, and also beneath your skin. With time they will all dissolve (soften and fall out). You may notice small threads on your sanitary pad or in the bath.
You may be able to feel some of the stitches, especially those around the anus muscle, for up to three months. This is normal. Sometimes these stitches are visible (on the outside of your skin). Other times they may be internal and may not be noticeable.
You are likely to feel pain or soreness for four to six weeks after giving birth. It may be more uncomfortable particularly when walking or sitting. The stitches can irritate, or feel tight as healing takes place. This is normal. To help with any discomfort, you can take:
paracetamol (maximum 4 doses in 24 hours); and
ibuprofen (maximum 3 doses in 24 hours).
Passing urine can sometimes sting. Pouring water over the area when urinating (weeing) can help.
Using ice packs on your perineum can also help. The cold will help reduce pain and swelling. Wrap the ice in a tea towel first. Never apply ice or ice packs directly to your skin as they can damage your skin.
See your midwife, GP, or healthcare professional if you have any worries. These could include:
the way your wound is healing
you noticing bleeding from the tear; or
you have increased pain or smell.
Preventing infection
Following these instructions will help reduce your chances of developing an infection around your wound and stitches.
Wash your hands with soap and warm water before and after going to the toilet. This will help to avoid introducing any bacteria to your wound and stitches.
Change your sanitary pads at least every 4 hours, every time you go to the toilet, or sooner if needed. Do not use tampons while you are healing, as they can cause an infection.
Keep your perineum clean. Wash your perineum daily using water only. Using soap or shower gel, may irritate your wound.
What are the signs of infection?
Signs of infection might include the following.
Red, swollen skin around your stitches.
Discharge or pus from your wound.
Increase in pain or tenderness around your wound.
A smell that is not normal for you.
Fever (high temperature / feeling hot).
Chills and sweats.
If you have any of the above, please see a midwife or a doctor.
You can call Maternity Triage up to 42 days after the birth of your baby. They are open 24 hours a day 7 days a week, and their number is at the bottom of this leaflet. After 42 days, please see your GP or call 111 if out-of-hours.
You may need antibiotics to help it heal. If you have already been given antibiotics, you may need to have your medication reviewed.
What do I need to know about my bowels?
It can be common to feel anxious about opening your bowels following a third- or fourth-degree tear. You can go home before you need to have your bowels open.
In the first few days after your repair, control of your bowels may not be as good as it was before you had your baby.
You may notice that you have difficulty controlling your bowels at first.
You may also have some issues controlling wind (flatus).
If this happens to you, do not worry and speak to your midwife or GP. These symptoms should settle when the swelling has gone, and the muscles in your back passage start to work properly again. This may happen after two or three weeks.
What will happen when I go to the toilet?
Opening your bowels (pooing) should not affect your stitches.
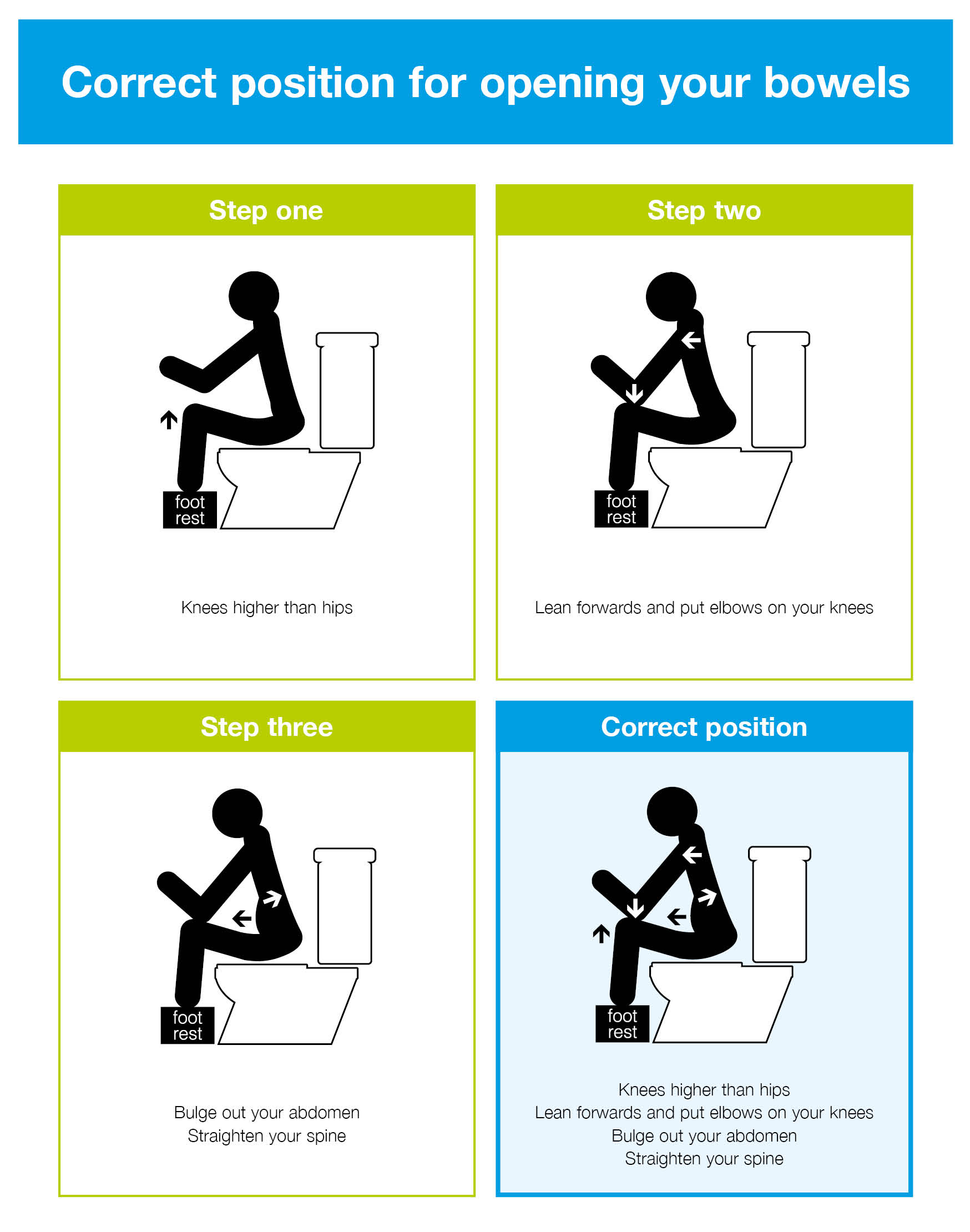
When opening your bowels, the best position to sit in is with your feet on a stool to raise your knees above your hips. This helps straighten out your bowels.
Try to relax and rest your elbows on your knees.
Bulge out your tummy by taking big abdominal breaths. Doing this will help you to pass poo without straining.
Take your time and do not rush.
How can I prevent constipation?
It is important to eat well and drink plenty of water to help avoid constipation. Being constipated may lead to straining on the toilet, which can damage your wound / stitches.
Drink at least two litres of water every day. If you are breastfeeding, you should drink to satisfy your own level of thirst.
Avoid alcohol, as this can dehydrate you.
It is important to eat a healthy balanced diet. For example, fruit, vegetables, cereals and wholemeal bread. Increasing fibre in your diet can help you to avoid constipation.
The doctor will prescribe you laxatives to take home. Laxatives will help soften your stools to avoid any constipation and straining on the toilet. They are safe to take while breastfeeding.
Will I be able to breastfeed?
Yes. None of the treatments offered will prevent you from breastfeeding.
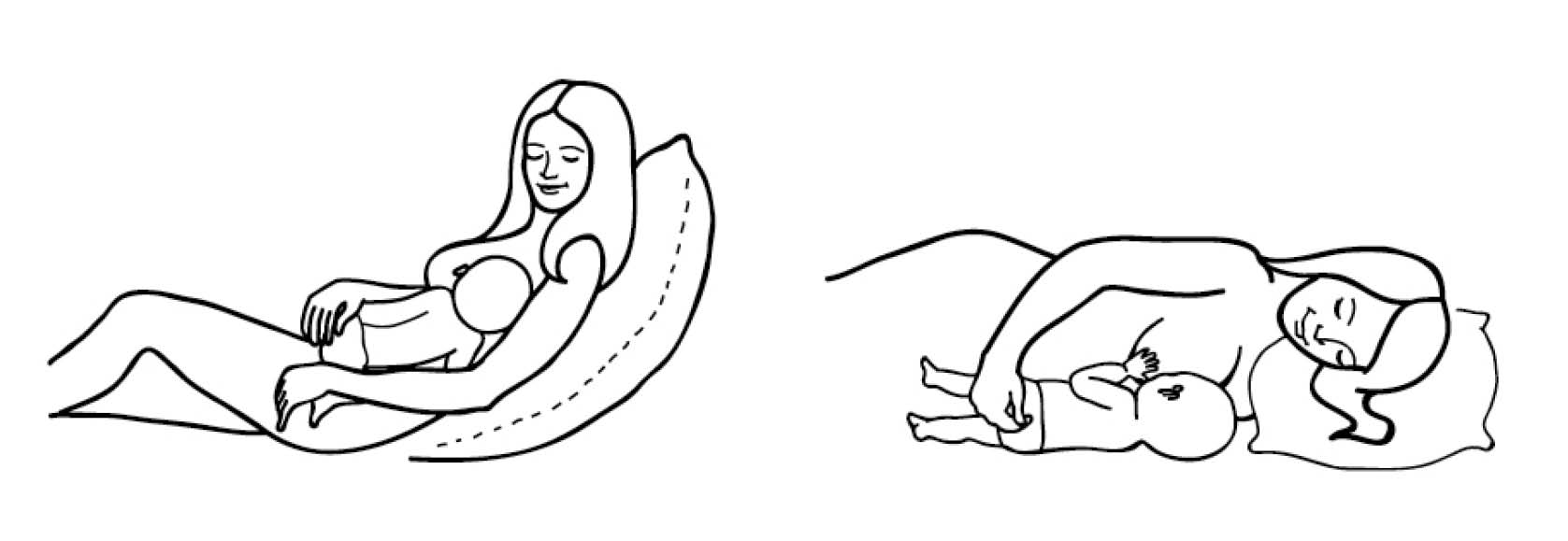
You may find it difficult to sit down for long periods of time. Breastfeeding in positions other than sitting may be helpful, such as laying on your side.
If you feel that you need more support, talk to your midwife. They will show you comfortable positions for you and your baby.
How can I improve my bladder and bowel control?
After giving birth, it is important to strengthen the muscles around your vagina and anus. This will help these muscles to heal, which will help you to control your bladder and bowel. This is even more important if you have damage to your perineum from a third- of fourth-degree tear.
To help strengthen these muscles you must do pelvic floor exercises as soon as you can after birth.
What are pelvic floor muscles?
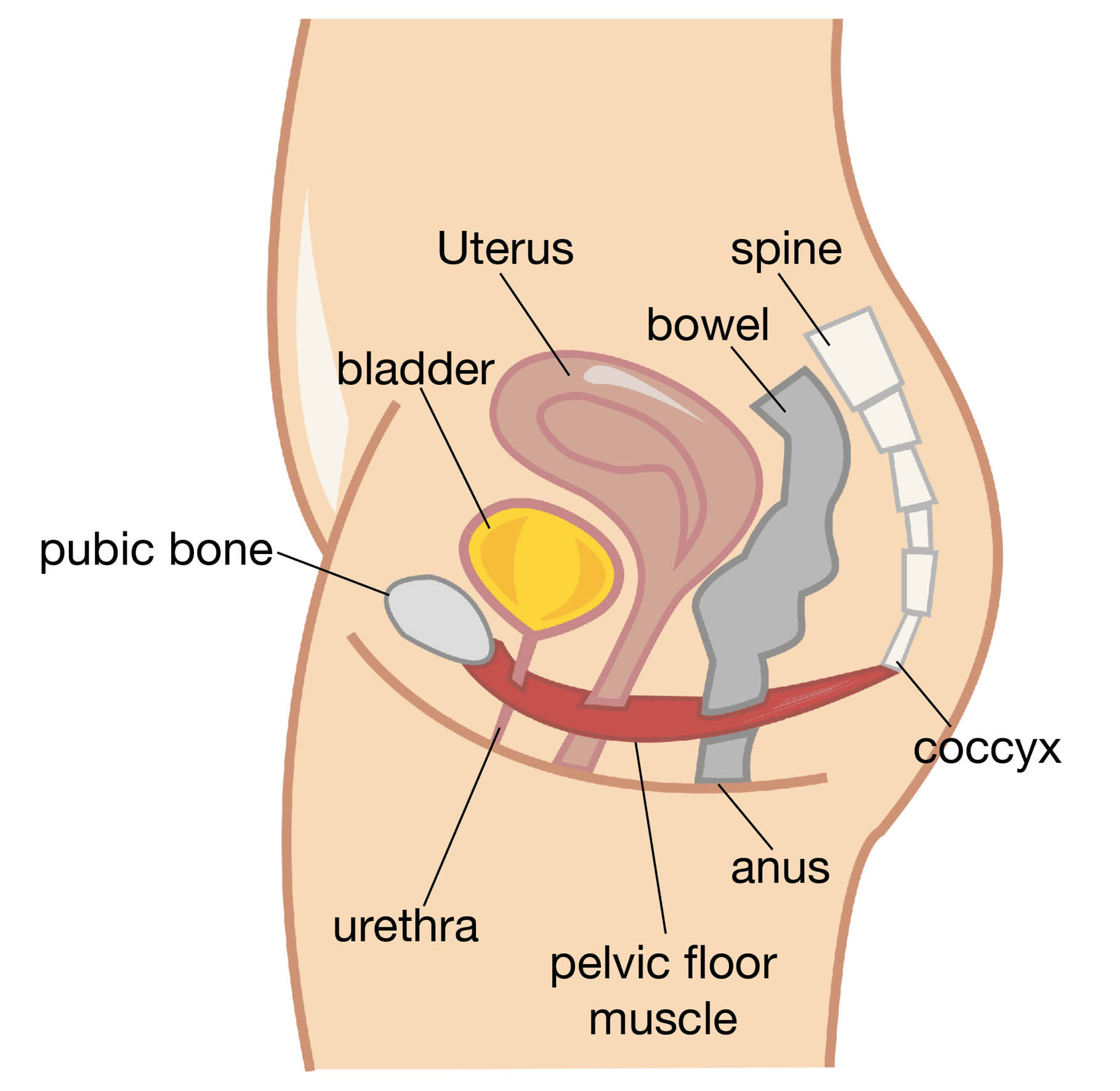
Pelvic floor muscles help to prevent the involuntary leakage of urine. They contract (squeeze) when you cough, sneeze or strain, stopping urine from leaking out.
They help to support the organs in your abdomen, especially when you are standing.
They help to protect your pelvic organs from external damage.
They help to hold your pelvic organs, like the bladder, in the correct position.
They help in the control of passing of urine, gas, and bowel motions.
They play a role in sexual function during intercourse.
Your pelvic floor muscles need to be fit and toned, just like any other muscle in your body. This allows them to work well.
Your pelvic floor muscles will not be very strong straight after giving birth. It is important to strengthen these muscles as soon as possible.
More information is available in the Pelvic health and wellbeing during pregnancy and after birth leaflet and in the short video produced by NHS Highland.
How can I exercise my pelvic floor muscles?
It is important to learn to do these exercises in the right way. Remember to check from time to time that you are still doing them correctly.
A continence referral to the Kent Community Health team will be made before you go home. You can start your pelvic floor exercises when you feel ready. The team's physiotherapist will contact you by letter, asking you to arrange a physiotherapist appointment. They will make sure you are doing your pelvic floor exercises correctly. They may use diagrams, drawings, and models at your appointment.
Sit comfortably with your feet and knees wide apart. If you prefer, you can lie down flat (supine position) with your legs slightly apart. Remember to keep breathing throughout. Keep your stomach, leg and buttock muscles relaxed.
Breathe in and let your tummy relax and rise.
Imagine that you are trying to stop yourself from passing gas from the bowel. At the same time also trying to stop the flow of urine from the bladder. You should feel a lifting and tightening around your vagina and anus.
Looking at your muscles can be a way of checking they are working correctly. Lie propped on the bed; place a small mirror between your legs with your knees bent and apart. As you pull up the pelvic floor you should see your anus and entrance to the vagina lifting and drawing in.
Note: If you notice the entrance to your vagina widening, you are pushing down and not pulling up. This is the opposite to tightening the pelvic floor muscle. If you leak urine or pass gas when doing the exercises, it is also likely you are pushing down and not pulling up.
How often should I do these exercises?
First decide on your ‘starting block’. Tighten your pelvic floor muscles as much as you can. Do this without using your buttocks or thigh muscles as described above. Hold tight for as many seconds as you can (up to 10 seconds at the most).
How long can you hold this contraction? _____ seconds (for example 2 seconds).
Release the contraction, and rest for at least the same time of the contraction. Repeat the ‘tighten, hold and release’ as many times as you can (no more than 8 to 12 times).
How many times can you repeat the contraction? _____times (for example 4 times).
This is your ‘starting block.’ Repeat your starting block 4 to 6 times during the day.
With this muscle training, your pelvic floor will get stronger. Your starting block will then change, for example hold for 4 seconds, and repeat 6 times. This now becomes your new starting block.
This program builds up the endurance of your pelvic floor muscles. In other words, the muscles will be able to work harder for longer.
Now perform the pelvic floor exercise but squeeze quickly and then let go. Rest 1 to 2 seconds before the next one. These are called quick contractions. They will help your muscles react quickly when you laugh, cough, exercise, or lift.
How many contractions should I do?
Aim to do 8 to 12 contractions, 3 times a day for at least 6 months. That is the easy bit; the most difficult part of the program is remembering to do the exercises. Here are some tips to help remind you.
Wear your watch on the wrong wrist.
Put stickers in places that will catch your eye. For example, your bathroom mirror, telephone, fridge, kettle, or steering wheel.
Exercise when feeding your baby.
Use reminders or alarms on your phone.
Download the squeezy app to set an exercise program. This will remind you to exercise.
How quickly will I see results?
It may take up to 6 months to see an improvement in your bladder control. Do not give up.
What if the exercises do not help me?
When you start these exercises, you may have very little feeling in your pelvic floor. This should improve the more you do your exercises.
However, if there is little or no improvement in your pelvic floor, you may need to see a physiotherapist. Particularly if you continue to have problems controlling your bowel and / or bladder. A referral to the Physiotherapy team will be made for you before your discharge from hospital. The team will contact you around 6 to 8 weeks later. They will teach you how to squeeze and strengthen your anal sphincter muscles. This will help to reduce any incontinence.
Useful links
Pelvic Floor Video (NHS Highland)
What is anal incontinence?
Anal incontinence is when you have problems controlling your bowels. Symptoms can include the following.
Sudden, uncontrollable urges to open your bowels (poo).
Not being able to control passing wind.
You may also soil yourself or leak faeces (poo).
Most third- or fourth-degree tears heal completely. Some women or birthing people may experience the symptoms listed above. It is important to talk about any concerns you have.
If you experience anal incontinence you will be referred to a specialist team. Treatment may include physiotherapy or surgery. If you have any of the symptoms listed above, talk to your GP or healthcare professional, or contact the OASI lead midwife.
What should I expect when getting back to my normal daily activities?
All patients recover differently. What you view as normal daily activities will also differ from person to person.
If you have had a third- or fourth-degree tear, you should avoid strenuous activity or heavy lifting for 4 to 6 weeks. After this time, you can gradually increase your general activity.
If you have pain that is not improving call Maternity Triage. Their number is at the end of this leaflet.
Looking after a newborn baby and recovering from an operation for a perineal tear can be hard. Support from family and friends can really help you while your body adjusts and gets better. If symptoms continue after 6 months, see your GP or healthcare professional.
Having complications when giving birth can be very distressing and disturbing. For some there is a risk of post-traumatic stress disorder (PTSD). Following a perineal tear, please contact your GP or health professional if you:
develop anxiety
have a low mood; or
feel that you need extra support.
When can I have sex?
The thought of having sex again after giving birth can be worrying. Particularly if you have had a third- or fourth-degree tear.
Once your stitches have healed and bleeding has stopped, you can have sex again. It is important only to do so when it feels right for you and your partner.
It is important that you choose and use a suitable contraceptive. You can get pregnant very soon after giving birth, even before you have a period. You can discuss your contraception options with your GP or healthcare professional.
Perineal massage may help you feel more comfortable before you have sex again. You can do this on your own, or with your partner. It is not something everyone is comfortable with, you should not do it if you feel uncomfortable.
You may notice your vagina feels drier than usual, this is not uncommon if you are breastfeeding. A water-soluble lubricant may help. You can buy these at your local supermarket or pharmacy.
If you have experienced perineal trauma, it may be several months before you feel ready to have sex again. Sex may feel different at first, and you may feel some discomfort. Any discomfort should not persist as time goes on. You and your partner may be anxious and talking about these feelings may help. It is important that you both feel ready and relaxed. If you have continued pain or discomfort, please speak with your GP or healthcare professional.
Will I have a follow-up appointment?
The OASI lead midwife will contact you around 4 weeks after you have had your baby. They will check that your wound is healing, and address any issues or concerns you may have. Please make sure your contact details are up-to-date before you are discharged from hospital. You will also have the chance to discuss the birth and any concerns that you may have.
A physiotherapist referral to Kent Community Health team will be made following your birth. You will be contacted around 6 to 8 weeks after your discharge to arrange an appointment with them. They will support you with your pelvic floor exercises and give support, if needed.
A uro-gynae specialist nurse will contact you around 12 weeks following birth. The nurse may ask some of the following questions.
Are you having any problems controlling your bladder or bowel?
Do you feel any perineal pain?
Are you having any problems with sex, such as not fully able to enjoy intercourse? Do not worry if you have not had sex yet. You can contact the specialist nurse if you have any concerns when the time is right for you and your partner.
Do you have any other concerns?
If you are worried or concerned about your health at any time, please see your GP or a healthcare professional.
What about my future birth plans?
If you have recovered well and do not have any symptoms, you may wish to consider a vaginal birth with your next pregnancy. If you continue to experience symptoms from your third- or fourth-degree tear, you may prefer to consider a planned caesarean birth. You can discuss your options with your midwife.
It is not possible to say if you will have another third- or fourth-degree tear in future vaginal births. The Royal College of Obstetricians Gynaecologists (RCOG) suggest if you had a third- or fourth-degree tear in your first birth, 7 to 10 women or birthing people in every 100 may have a similar tear in their next vaginal birth.
Risk factors for having a repeat third- or fourth-degree tear include:
having a forceps birth
your baby being born heavier than 4kg (kilograms)
being of Asian ethnicity.
You will be able to discuss your options for future births at your follow-up appointment. You can also discuss this early in your next pregnancy. Your midwife or obstetrician will discuss your individual experience with you. They will discuss birth options, and listen to your preferences. You can then make the decision that is right for you.
What if I have any questions or concerns about my tear?
If you have general questions concerning your third- or fourth-degree perineal tear, please contact the OASI Lead Midwife.
If you have urgent worries or concerns about your tear, please call Maternity Triage on 01227 206737.
Further information and support
References
East Kent Hospitals University NHS Foundation Trust. Perineal Trauma (including prevention, recognition, repair and post-operative care) Guideline. May 2023.
Royal College of Obstetricians and Gynaecologists (RCOG). Your pelvic floor.