The Rhesus factor and anti-D
Information for women, birthing people, and their families
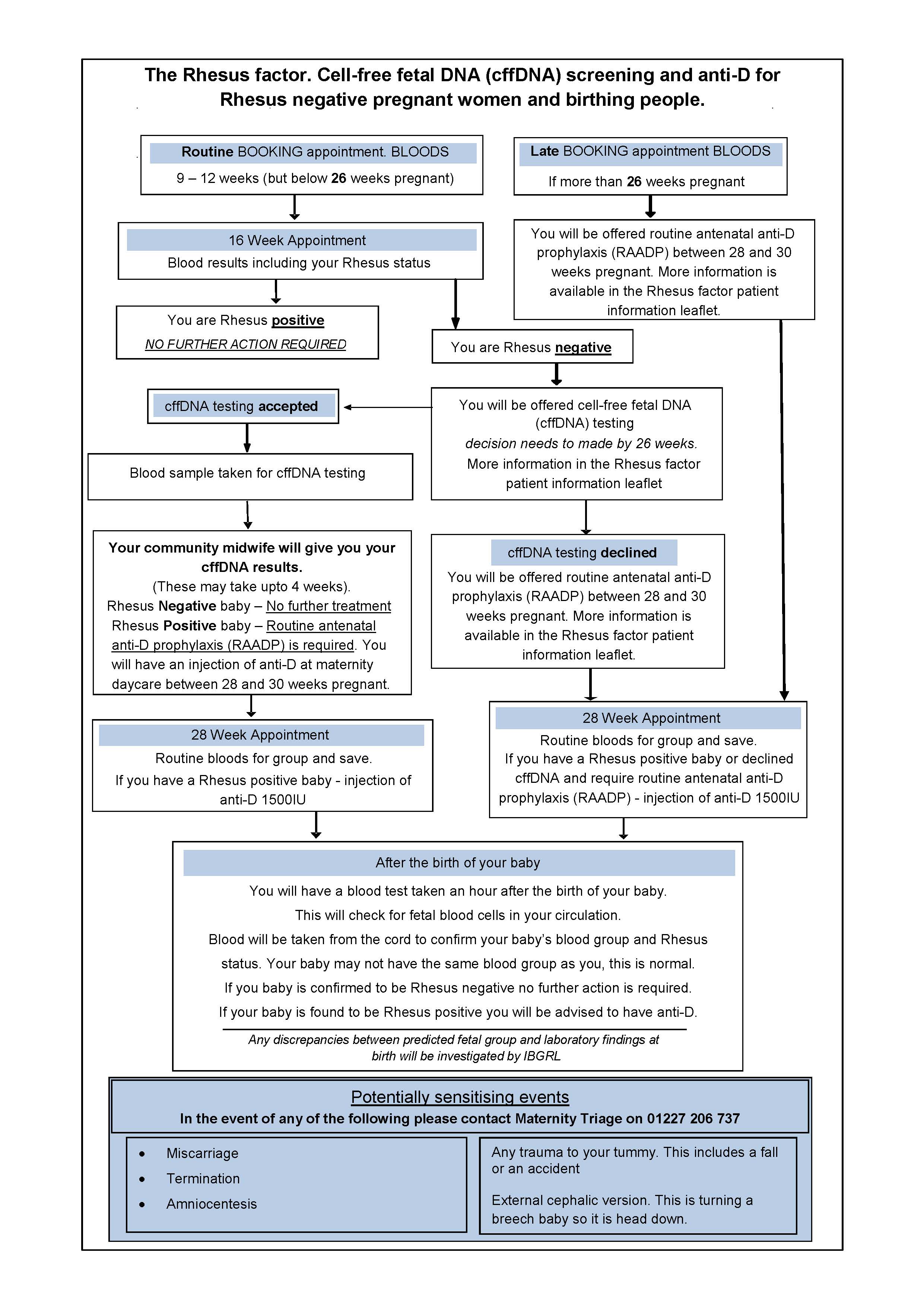
We have given you this leaflet as you are pregnant and your blood group is Rhesus negative. It explains why you may need to have anti-D injections during your pregnancy and after your baby’s birth.
Anti-D will protect you from making antibodies against your baby’s blood in the future. This has been common practice in the UK for more than 20 years. Your current pregnancy will not be affected by these antibodies. This will only affect your future pregnancies.
What is Rhesus negative blood?
There are several different types of human blood, known as blood groups.
Group A
Group O
Group B
Group AB
Each of these blood groups can either be RhD positive or negative.
Your baby may not have the same blood group as you. This is normal. Being RhD positive or RhD negative is determined by the presence of the rhesus D (RhD) antigen. This is a molecule found on the surface of red blood cells.
People who have the RhD antigen are RhD positive, and those without it are RhD negative. In the UK, around 85 of every 100 members of the population (85%) are RhD positive.
How can the Rhesus factor affect my pregnancy?
Sometimes in pregnancy, a small amount of blood can cross from the baby to the woman or pregnant person. This is called a Feto-Maternal Haemorrhage (FMH). It generally happens just before birth and is quite normal. It occurs in nearly 75 of every 100 pregnancies.
It can also happen after a sensitising event. Sensitising events include:
a miscarriage
an amniocentesis (needle test in your tummy for Down’s syndrome), or
trauma to your tummy.
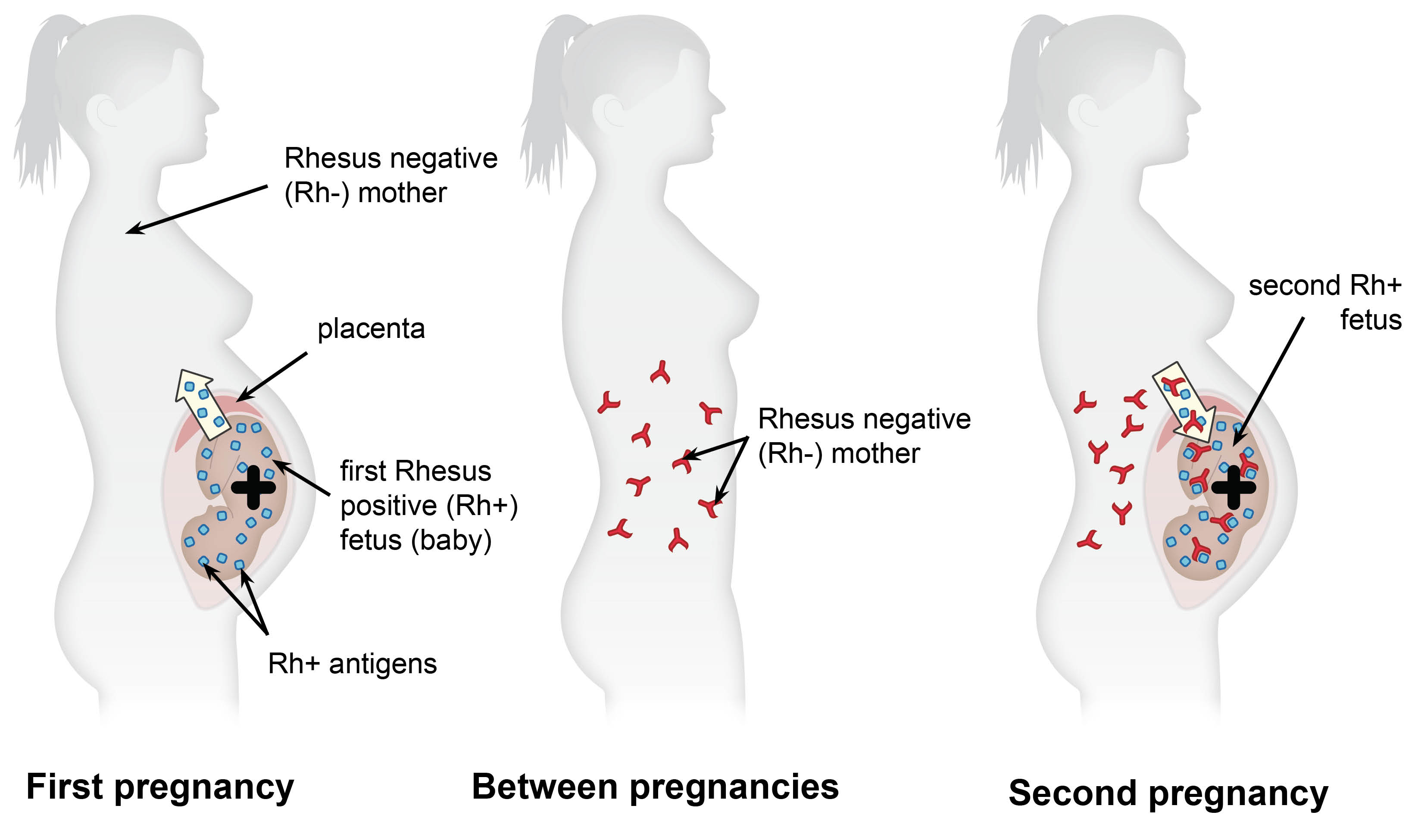
Any blood from a Rhesus positive baby in the bloodstream of a Rhesus negative woman or pregnant person can be seen as ‘foreign’. The maternal immune system may then make antibodies against this ‘foreign’ blood.
In the future your immune system will remember how to make these antibodies. This helps your body to make them more quickly and in greater numbers, if needed.
This only becomes a problem during your next pregnancy. If your baby is again Rhesus positive, and there is another transfer of blood across the placenta. Your immune system uses its “memory” to make the same antibodies as before. These antibodies can then cross the placenta to your baby. They can start to attack your baby’s blood within your baby’s circulation before their birth. This is called Rhesus disease.
Babies who have this problem have Haemolytic Disease of the Newborn, or HDN for short.
HDN can be very mild and only found using a blood test. However, it can be serious and cause your baby to be:
jaundiced
disabled
stillborn, or
to die after birth, as a result of anaemia.
In England and Wales, about 500 babies develop HDN each year. In 2022 there were 605,479 births in England and Wales. These babies must be closely monitored after their birth. Each year about 25 to 30 babies die from HDN, and a further 30 will have minor developmental problems.
What protection is available?
Doctors and midwives are very aware of this problem and can stop it from happening. They do this by giving an injection of anti-D immunoglobulin (anti-D for short). This stops your body producing antibodies against Rhesus positive blood cells. This will then stop HDN developing in future pregnancies. This is known as anti-D prophylaxis. Prophylaxis is a treatment used to prevent something from happening.
An injection called anti-D is recommended to all women and pregnant people who are Rhesus negative. This is called routine antenatal Anti-D prophylaxis, known as RAADP. This has been recommended by the National Institute for Health and Clinical Excellence (NICE) since 2002. It is not suitable for women and pregnant people who have been ‘sensitised’. If you are already ‘sensitised’ this means that you already have antibodies to anti-D in your blood. A blood test at the beginning of your pregnancy will find out if this is the case for you.
We offer screening to all Rhesus negative women or pregnant people. This blood test predicts the Rhesus type of your unborn baby’s blood. This is called free baby’s DNA (ffDNA) testing. It involves you having a blood test at 16 weeks (you can have this test up to 26 weeks). This will give us time to arrange an anti-D injection at 28 weeks should you need it.
You can also have this screening if you have a multiple pregnancy (twins or more). It is your choice whether to take these tests or not. If you are unsure about what to do, please speak to your midwife or obstetrician.
Anti-D is not needed if your unborn baby is Rhesus negative. We can reduce the amount of unnecessary anti-D that we give with this screening.
What are the benefits of fetal RhD (Rhesus) screening?
If the screening predicts that your baby is Rhesus negative, you will not need to have any further tests. This means you avoid having unnecessary anti-D injections.
What are the risks of fetal RhD (Rhesus) screening?
There is a very small chance that the screening predicts the wrong blood type for your baby. Therefore, after your baby’s birth we will double-check your baby’s blood type. We do this by taking a sample of blood from their umbilical cord. This will confirm that your baby is Rhesus negative. This result is usually available in about two hours, so it should not delay you going home.
If it comes back showing that your baby is Rhesus positive, we will discuss what this means with you. We will recommend that you have a blood test to check if a feto-maternal haemorrhage (FMH) has occurred. We will also offer you an anti-D injection within 72 hours of the birth.
When is anti-D given?
We may give you anti-D in three situations.
Antenatal anti-D prophylaxis (AADP)
For a potentially sensitising event. Your baby’s blood cells can enter your circulation during a sensitising event. You may receive an injection of anti-D if you are Rhesus negative after such an event. These include:
o a miscarriage
o a termination
o an amniocentesis
o vaginal bleeding
o a fall or accident, which could cause an injury to your tummy, or
o an external cephalic version (turning a breech baby so they are head down).
Even if you wish to have Rhesus screening, you may have already had a potentially sensitising event before you get the results of your baby’s blood type. If so it is very important that you contact the Early Pregnancy Assessment Unit or Maternity Triage. You do not need to do so if you have already been told that your baby is predicted to be Rhesus negative.
Early Pregnancy Assessment Unit. If you have any potentially sensitising event before your dating scan. Contact details are at the end of this leaflet.
Maternity Triage. If you have any potentially sensitising event during your pregnancy. Contact details are on your lilac notes and at the bottom of this leaflet.
Routine antenatal anti-D prophylaxis (RAADP)
We will offer you RAADP when you are 28 weeks pregnant:
o if your baby’s blood type is predicted to be Rhesus positive
o if you decline fetal Rhesus screening, or
o if you have an inconclusive result.
This is a single injection of anti-D. It is given into the muscle of your upper arm. You must have this injection between 28 and 30 weeks of pregnancy. This is because the risk of sensitisation is highest in your third trimester. You must still come to your appointment for routine anti-D prophylaxis at 28 to 30 weeks. This is still needed even if you had anti-D earlier in your pregnancy.
Postnatal anti-D prophylaxis (PADP)
After the birth, a blood sample will be taken from your umbilical cord to test your baby’s blood group. You will need another injection of anti-D if your baby is Rhesus positive. This will remove any of your baby’s Rhesus positive red cells from your blood.
The dose of anti-D given may vary. It will be determined by the amount of the feto-maternal haemorrhage (FMH). This generally happens just before birth and it is quite normal. You should still be offered PADP even if you have already had other tests, AADP or RAADP.
What are the risks of having anti-D?
Anti-D immunoglobulin is made from a part of the blood called plasma. It is collected from screened blood donations from the USA. The production of anti-D is strictly controlled. This is to reduce the chance of a known virus being passed from the donor, to the anti-D and then to the recipient. The risk of this happening is very rare.
Anti-D can cause an allergic reaction, but this is rare.
If you have a bleeding disorder, we may give you anti-D intravenously (through a small tube in your vein).
I did not have free baby's DND (ffDND) testing, or I have already been told that my baby is predicted to be Rhesus positive. Do I still need to have anti-D injections?
No, the choice is yours. The aim of the anti-D injection is to reduce the risk of your future children developing HDN. In some cases, anti-D may not be necessary, including if:
you have chosen to be sterilised after the birth of your baby, or
you are certain that you will not have another baby.
What if I have any further queries or concerns?
Your midwife or doctor will be happy to tell you more about the Rhesus factor and what it means to you. If you have any questions, or if you have any doubts about the anti-D injection, do not be afraid to ask.
Contact our Maternity telephone triage service on 01227 206737 for help and advice.
Early Pregnancy Assessment Units
Birchington Ward, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234469Women’s Health Suite, William Harvey Hospital, Ashford
Telephone: 01233 633331 extension: 723-8268
Further information
References

NICE. High-throughput non-invasive prenatal testing for fetal RHD genotype. Diagnostics guidance (DG25). Published: 9th November 2016.
Qureshi H, Massey E, Kirwan D, et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. First published 21 January 2014.
NICE. Routine antenatal anti-D prophylaxis for women who are rhesus D negative. Technology appraisal guidance TA156. Published: 27th August 2008.