Surgery for testicular cancer
Information for patients from Urology
This information leaflet is for men who have been diagnosed with a possible testicular cancer, and will need an orchidectomy. The aim of this leaflet is to answer questions about your diagnosis and surgery.
What is testicular cancer?
Testicular cancer is a malignant tumour that invades healthy tissue but may spread to other body organs.
Testicular cancer is uncommon compared to other cancers, such as breast or lung cancer. Although uncommon, testicular cancer is the most common solid tumour in men aged 15 to 35.
What causes testicular cancer?
The cause of testicular cancer is unclear. However several factors have been noted in relation to the disease. For example, undescended testes (testes which have not dropped into the scrotum) that are not corrected in early childhood have been linked with an increased development of testicular cancer or any disorders of testicular development.
After treatment we recommend that you examine your testis every month.
What are the signs and symptoms of testicular cancer?
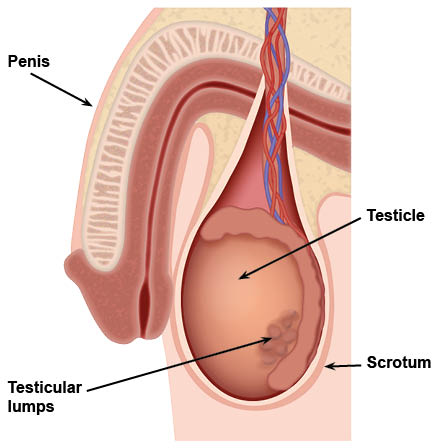
Most often testicular cancer begins with a hard painless lump. You may also have a dull ache, heaviness, or pain in your scrotum. Sometimes your scrotum is swollen and you cannot feel the normal testicle inside it.
The lump or swelling can be there for quite a while, or it can appear almost overnight and be very painful. Very rarely, your whole scrotum (left and right sides) is swollen.
How is testicular cancer diagnosed?
Different problems can produce different symptoms and different findings on examination. The most important things are your history (record of past events) and the physical examination of your scrotum. However sometimes it is impossible to determine what is inside the scrotum just by performing a physical examination.
Other tests may include the following.
Ultrasound is where harmless sound-waves are aimed at the area of your scrotum. The sound-waves bouncing back (the echo’s) from this area are seen as a picture on a screen. This is a painless, convenient, and highly accurate way to examine organs and tissues inside your scrotum.
Tumour markers are blood tests that if raised, signal certain types of testicular cancer. Not all testicular cancers will cause raised tumour markers, so having normal levels does not rule out the diagnosis.
In all patients diagnosed with testicular cancer we like to perform a CT scan of their chest, abdomen, and pelvis. This is to make sure the disease has not spread to other areas, particularly the abdominal lymph nodes. Your doctor will explain this in more detail.
What procedure am I having?
The procedure is called an orchidectomy (an operation to remove your testicle). It is carried out through an incision (cut) in your groin and not through your scrotum.
Your surgeon will also give you the option of inserting a testicular prosthesis, if it is something you wish to have. Your surgeon will discuss the benefits and risks of this with you before your procedure.
Are there alternatives to surgery?
You will discuss your treatment options with your surgeon before anything is planned. However surgery is the definitive treatment.
What will happen before my operation?
You will need a surgical assessment appointment before your surgery (pre-surgical assessment). This will include a blood test and maybe an ECG (which records the rhythm of your heart).
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
What happens when I arrive at hospital for my orchidectomy?
You will be admitted to either Kent Ward or Day Surgery at Kent and Canterbury Hospital.
Admission details, including the date and time of your operation and instructions on when you can eat and drink before surgery, are listed in your appointment letter. If you have any questions, please contact Kent Ward before the day of your surgery.
Will I have an anaesthetic?
Your operation is carried out under a general anaesthetic (you will be asleep for the procedure). A local anaesthetic is also placed in your wound, so it should be numb when you wake up after surgery.
How long will I be in hospital?
The procedure takes approximately half an hour. You are usually in hospital as a day case (you can return home on the day of your operation), but you may be advised by your surgeon to stay in hospital overnight.
Will I have stitches?
Yes, but they are dissolvable and should dissolve within two to three weeks. They are usually placed under your skin so you cannot see them.
How will I feel after my operation?
You may feel some discomfort after your surgery and will be given painkillers to take home.
Are there any risks to having the operation?
Possible complications are:
infection
bruising
bleeding into the scrotum (scrotal haematoma)
seroma or fluid collection within the scrotum
pain
swelling of the wound
numbness of the skin below the incision, which may be permanent; and
less than one in every 100 patients may need to return to theatre for bleeding complications.
These symptoms should not last long but if they continue or you have any concerns, please contact either your GP or your cancer nurse specialist (CNS).
What should I do when I return home?
For the first week after your operation:
You may walk about and climb stairs but do not overdo things.
Be sensible and take regular breaks during the day; this will help to reduce any swelling of your scrotum and make you feel more comfortable.
Do not lift heavy items; ask someone to do it for you.
Wear jockey type shorts rather than boxer shorts.
When can I drive again?
Do not drive for one to two weeks after your operation, or until you feel comfortable. Before driving again you must be pain free and able to perform an emergency stop without discomfort.
When can I return to work?
Depending on the type of work you do, you should be able to return to work two weeks after your operation. If your work is physically strenuous then you may need longer to recover. Please discuss this with your doctor.
Will I need a follow-up appointment?
Yes. An outpatient appointment will be arranged and sent to you for three to four weeks after your operation.
An automatic appointment will be made with an oncologist at Maidstone, who reviews all testicular cancer patients in the region. This is to discuss the need for second line treatments such as chemotherapy. The need for this depends on the pathology result of your testicle, your CT scan, and your tumour markers. Not all patients need chemotherapy, many just have surveillance.
What if I feel unwell at home?
If you feel unwell or have concerns about your wound, please go to the Urgent Treatment Centre at Kent and Canterbury Hospital.
Further information
If you have any further questions or concerns, please contact Kent Ward on 01227 783102, or the urology / oncology clinical nurse specialists via the Cancer Careline on 01227 868666.
Alternatively further information is available from the British Association of Urological Surgeons (BAUS) web site.