Stable fractures (breaks) of the spine
Information for patients from the Radiology Department
This leaflet has been given to you as your x-ray shows that you have a fracture (break) to one or more of the bones in your spine (vertebrae). The fracture is known as a compression fracture. This leaflet will help you manage your fracture and give you advice on managing your pain.
What is a compression fracture?
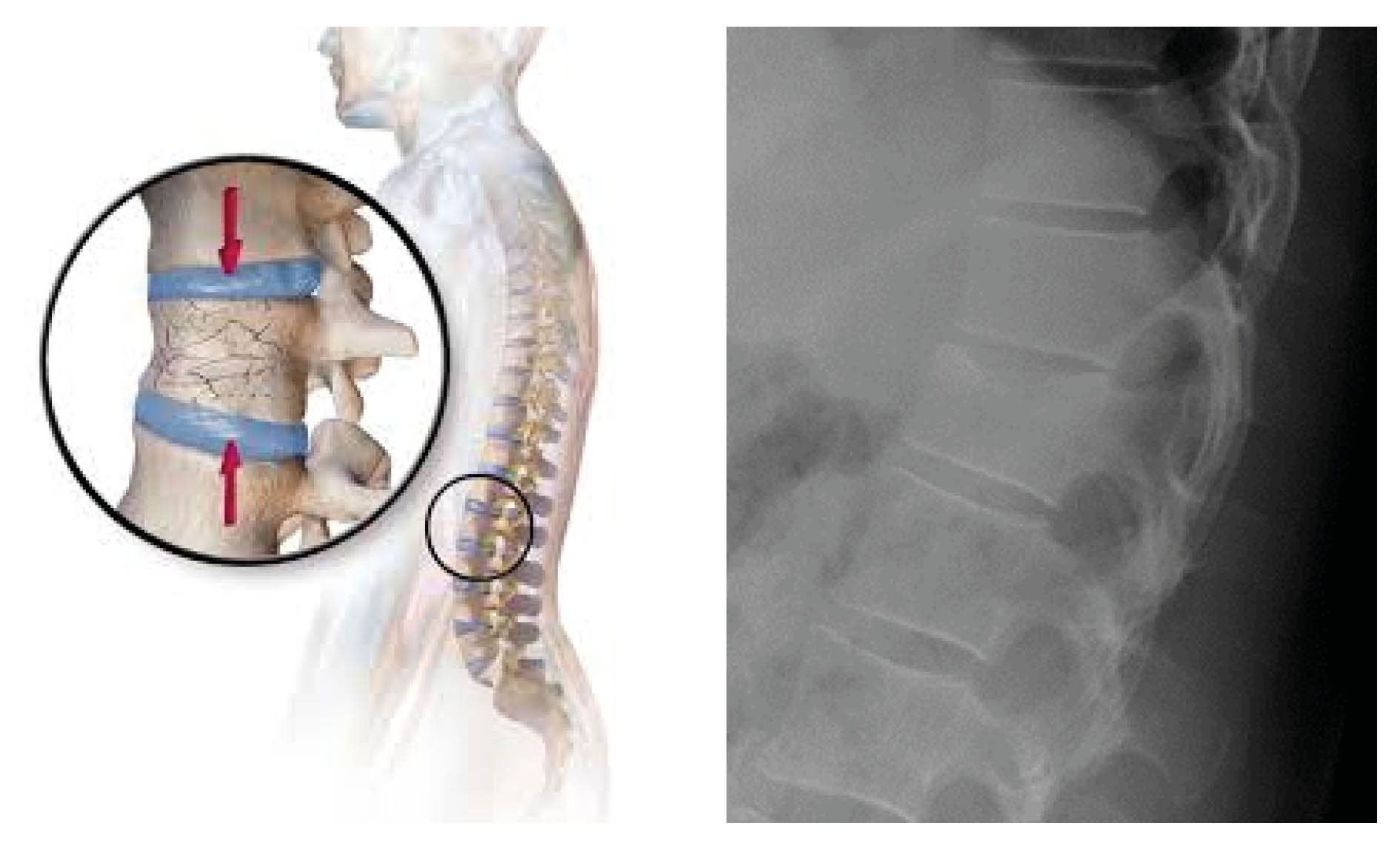
This is a type of fracture where the vertebrae (building blocks of the spine) caves in on itself due to compression or pressure on the bone.
There are several types of compression fractures. You will have either a crush, biconcave, or wedge fracture. These fractures are usually stable and do not cause any short or long-term paralysis.
What are the most common symptoms of a stable compression fracture?
You may have different levels of pain from your vertebral fracture, however not everyone feels pain.
You may also feel that your back is stiffer and notice that you have less movement and find it harder to stand up from a chair; this is likely to improve as your fracture heals.
Vertebral fractures can also cause small changes in your normal posture and loss of height.
What causes spinal compression?
The most common causes of a spinal compression fracture are osteoporosis and trauma. In patients with osteoporosis, a slight increase in stress on the back can cause vertebral bodies to fracture or collapse.
It is possible for other conditions or events to cause a vertebral compression fracture. Osteoporosis in the spine is by far the most common cause, especially in women over the age of 50.
What treatment is available?
The most common type of treatment for these types of injury is known as conservative management and will be led by your own GP. This means that that there is no invasive surgery or repair undertaken. The main aim of conservative management is pain control and returning you to your normal activities.
If your fracture is painful you will probably need to take painkillers. Please ask your GP or pharmacist for advice.
Other treatments include prevention of further fractures and progressive deformity. We would usually suggest reducing but not avoiding normal daily activities that cause you pain. Avoiding activity completely can weaken your bone further and in some cases result in muscle weakness and joint stiffness.
Some sports may need to be avoided until your fracture has healed and your pain has settled. You can continue with activities such as gentle swimming and walking if you are able to. It is useful to pace activity such as housework, so that your pain does not increase too much; pacing is taking a break before you need it.
Your GP may prescribe you painkillers and advise you regarding your mobility and activities. Other treatments and investigations may include:
physiotherapy
falls prevention
osteoporosis assessment and treatment (if needed); and
investigation of other possible causes for bone weakness.
You can discuss with your GP whether these treatments are appropriate for you.
Is surgery an option?
Sometimes it is considered necessary to have surgery. But surgery is only usually needed if pain does not improve, worsens, or new neurological symptoms arise (see the list of neurological symptoms below). If these symptoms happen you should go to your nearest Emergency Department immediately by ambulance. Do not try to drive yourself.
You should try to move as little as possible until you have been checked by an Emergency Department doctor.
Important neurological symptoms to be aware of
Reduced leg strength (paresis) or complete weakness (paralysis).
Loss of sensation in your legs or buttock area.
Urinary retention (unable to pass urine) and urinary and faecal incontinence (unable to control bowel and bladder function).
Significant increase in level of pain.
If you have any of these symptoms then you should go to your nearest Emergency Department for further assessment. For symptoms one to three you must call an ambulance (999) immediately and limit all movement.
My level of pain keeps changing, is this normal?
Sudden increases in pain are common. If these occur, please limit your movement and take regular painkillers. If the symptoms do not quieten down then you must follow the same instructions as above.
It is very important that you are aware of any changes to your symptoms. It is common to have slight changes in your level of pain.
When and how will I receive my results?
Your full x-ray report (results) will be sent to the clinician who referred you. A copy will be made available to your GP on the day of your x-ray (when they are ready depends on the opening hours of your GP surgery).
A copy of your results will also be available to our Fracture Liaison Service. This team deals with osteoporosis and falls prevention. Please discuss a referral to them with your GP, who can arrange the referral.
How long will it take for my fracture to heal?
Your fracture usually takes about six weeks to heal. Over this time pain will improve in most cases.
Will I need a follow-up appointment?
In most cases any follow-up appointments will be with your GP. Please contact your own GP for
advice on this.
Further information
What if I have any questions or concerns?
Please contact your GP if you have any further questions about your condition.