Scaphoid fracture
Information for patients from the Orthopaedic Hand Service
You have a scaphoid fracture. This leaflet will explain:
what a scaphoid fracture is
the causes and symptoms
what your treatment options are, and
how to manage and treat your symptoms.
If you have any questions after reading this leaflet, please speak to your therapist.
What is a scaphoid fracture?
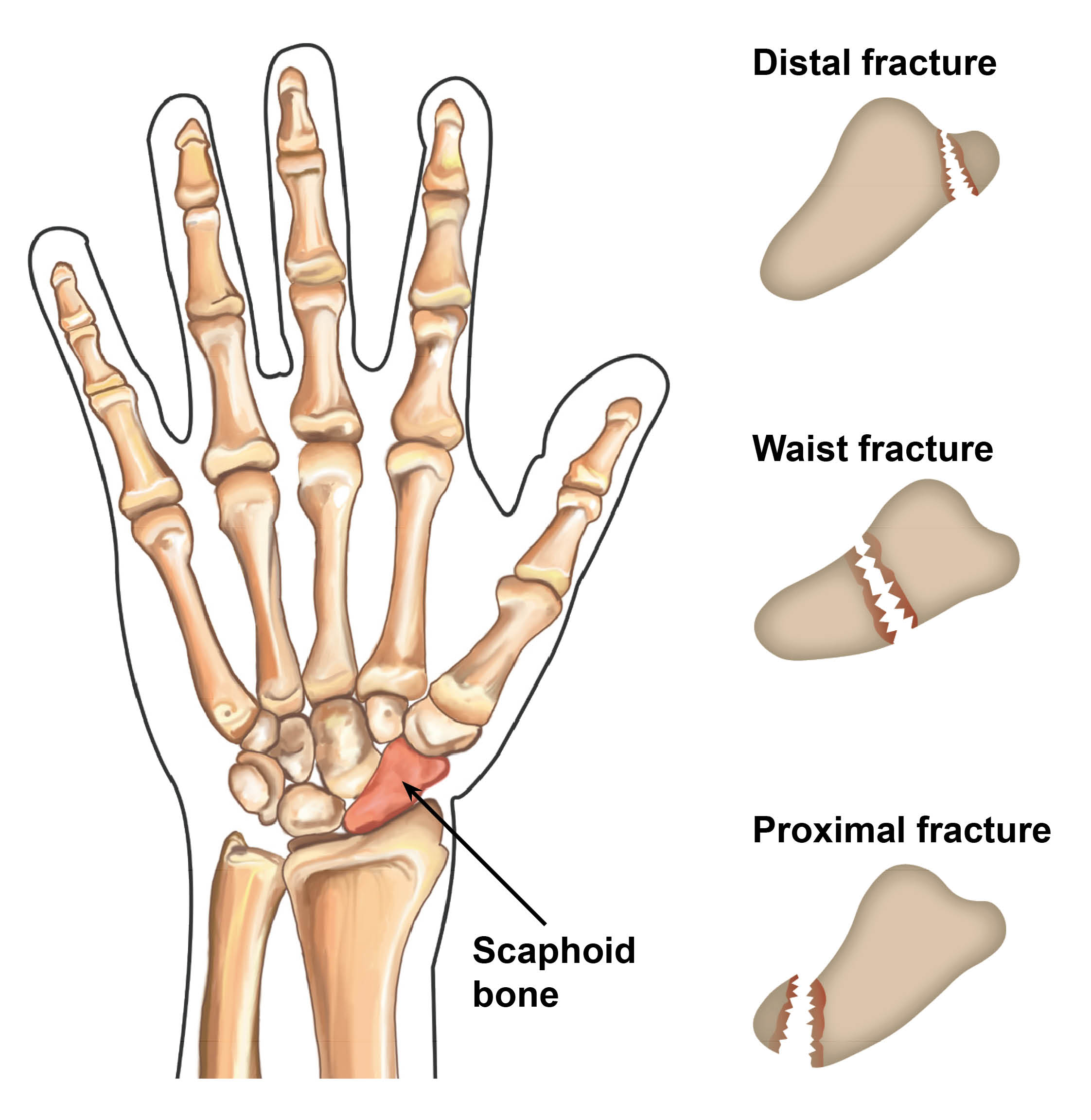
The scaphoid is one of eight small bones (called the carpal bones) of the wrist. It is found at the base of the hand, on the same side as the thumb. A scaphoid fracture is a break in this bone. A break is the same as a fracture.
What causes a scaphoid fracture?
Scaphoid fractures are usually caused by an unexpected force through the wrist and hand. This might be through contact with the ground, such as a fall onto an outstretched hand.
What are the signs and symptoms?
Pain or tenderness at the base of the thumb can be a sign of a scaphoid fracture. However, this can also occur with a wrist sprain or bone bruising. It can be difficult to see some scaphoid fractures on x-rays within the first week. It may be necessary to have further x-rays taken 10 to 14 days later. Sometimes you may also need an MRI scan.
If the doctor or nurse who sees you first is unsure, they may start treatment for a scaphoid fracture ‘just in case’ and refer you on to the Fracture Clinic. It is important that you attend any clinic or radiology (x-ray or scan) appointments.
How is a scaphoid fracture diagnosed?
Your doctor, nurse, or therapist will carry out a physical examination of your wrist to identify any symptoms. If needed, you will be followed up with further x-rays to show up this bone more clearly.
If a scaphoid fracture is still suspected but not shown on an x-ray, often you are seen again after a couple of weeks for repeat x-rays or referred for further scans.
What are my treatment options?
Many scaphoid fractures are successfully treated by immobilising the wrist (stop it moving). You will be in a plaster cast for six weeks, but your treating clinician will discuss this with you as sometimes the length of time changes. It is important during this time that you do not use your hand or move your wrist without the cast or brace in place.
Fractures which occur at the end of the scaphoid (see diagram above) may need to be immobilised for longer. Occasionally an operation is needed, due to a poor blood supply to this area of the bone.
Regardless of the treatment, it is very important for you to move your fingers and if you are able to make a full fist within one to two weeks of your injury. The exercises to help you do this are listed below.
After removal of your cast or after your operation you may be referred to the Hand Therapy Team. It is important that you start gentle movement early and that you try to use your hand for light activities. The aim of treatment is to restore normal movement to your wrist and hand as soon as possible.
What is the usual outcome after a scaphoid fracture?
Most scaphoid fractures heal without problems. It may take several months for any swelling to go down and to feel like you have full strength and flexibility in your wrist and hand. Gripping, full weight-bearing, and repetitive work can be uncomfortable for up to a year after your injury.
Is there anything I can do to help myself?
There are a couple of things you can do to help with your recovery.
Simple painkillers and anti-inflammatory medication (such as paracetamol or ibuprofen) can help manage pain and swelling. Please speak to your local pharmacist if you are unsure which medications you can safely use.
Try to keep your hand and wrist elevated (raised) above the level of your heart for the first one to two weeks. This will help with the swelling in your wrist. However, you should avoid wearing a sling as this can cause discomfort in your shoulder and neck.
Try to move your fingers. Open and close your hand in a fist as much as you can. This will help with tissue healing and prevent your fingers from becoming stiff.
Try to use your hand as normally as possible within the brace or splint. However, you should avoid any heavy lifting, pulling, or pushing for the first six to eight weeks after your injury.
Make sure you move all the other joints of your hand and arm as normally as possible to avoid any stiffness.
If you are wearing a cast, keep it dry. You can shower or bath, however you need to use a shower sleeve to stop your cast becoming wet. Please ask a member of staff for more information on where to buy shower sleeves from.
By stopping smoking you can greatly reduce your risk of your fracture not healing. Compared to non-smokers, smokers are more likely to have complications in tissue healing and infections after injuries or surgery. For free friendly support and medication to help you stop smoking, contact One You Kent on telephone 0300 123 1220 or via email.
What exercises should I do?
Do not start the following exercises until you have spoken to your treating clinician. They will guide you as to how long you should continue them for.
These exercises are appropriate if you are being treated conservatively or via surgical fixation.
To avoid stiffness and to help with your return of movement, perform these exercises five to 10 times, five times each day.
It is normal for these exercises to feel uncomfortable when your fingers are stiff.
Always complete them gently and slowly.
Hold each position at the end of each range for five seconds.
Always start and finish with your fingers as straight as possible.
-
-1717749787.jpg) 1. Touch the back of your head with your injured arm.
1. Touch the back of your head with your injured arm. -
-1717749795.jpg) 2. Lift your arm straight up above your head, towards the ceiling.
2. Lift your arm straight up above your head, towards the ceiling. -
-1717749809.jpg) 3. Bend and straighten your elbow, aiming to completely straighten it in front of you.
3. Bend and straighten your elbow, aiming to completely straighten it in front of you. -
-1717749815.jpg) 4. Bend your arm, and try to touch your fingertips to your shoulder.
4. Bend your arm, and try to touch your fingertips to your shoulder.
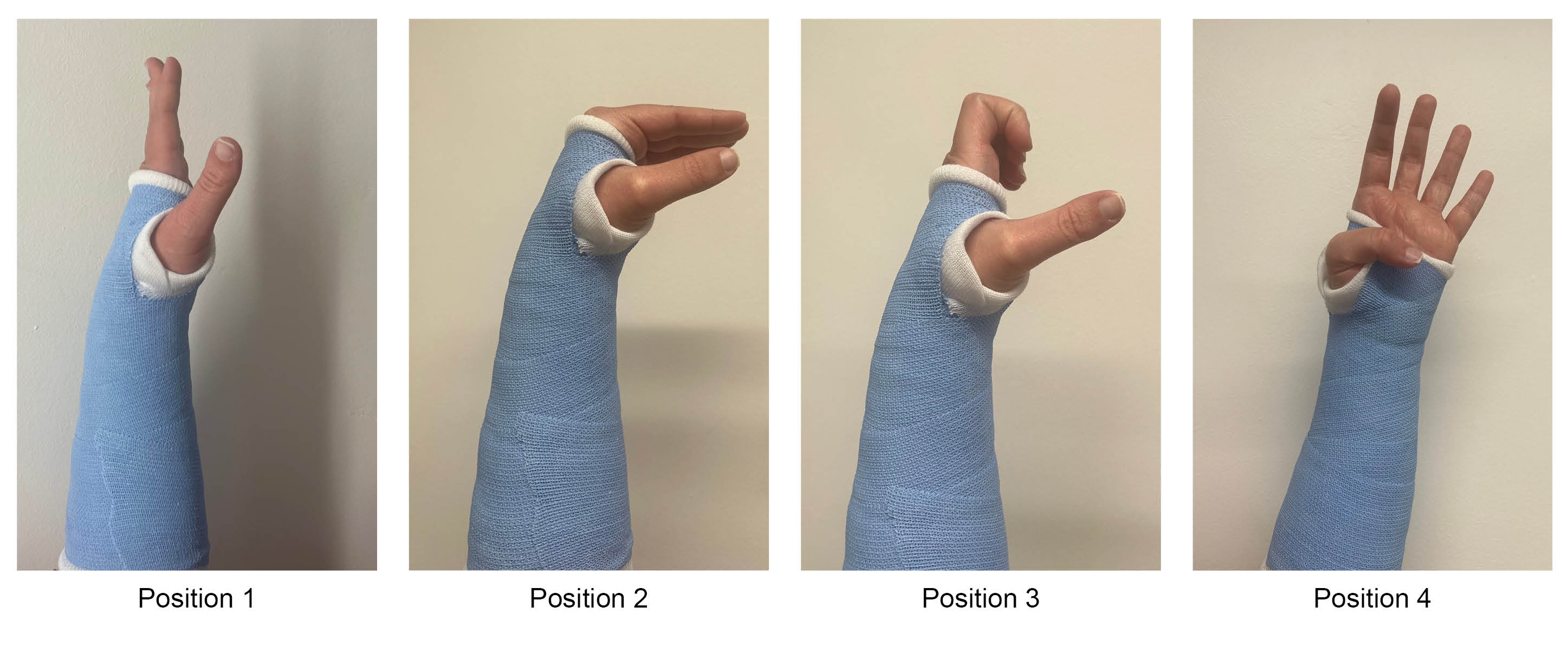

To start with you may find it difficult to complete these exercises due to pain and swelling, but aim to get as close to these positions as you can.
If your cast gets in the way or it feels too tight, please contact the Fracture Clinic for advice.
What happens if surgery is needed?
If you need surgery, you will discuss this with your treating clinician. They will explain your options fully. Please use this time to ask them any questions.
Before the day of your operation, you will be contacted by the Preassessment Clinic. At this appointment a nurse will discuss your operation with you.
They will ask you some questions about your general health. It would be helpful to take your usual medicines with you. The nurse will need to know their names and their strengths. This includes non-prescription medicines such as herbal / complementary medicines.
If you need to stop eating or drinking before your surgery, this will be explained to you at this appointment.
You may need to have some routine tests before your operation, such as a blood test.
Please feel free to ask questions and raise any concerns you may have about your operation. You will then be asked to sign a consent form.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
What are the risks with surgery?
Serious complications are uncommon. But a small number of patients can experience complications, some of which resolve with time. These include the following:
Delayed wound healing or infection. A small number of patients will develop an infection and may need antibiotics. Very rarely they may need a further small operation to clean out their wound, called a washout procedure. This is more common in patients with diabetes.
Your scar may be tender for several months. If it does not resolve with time, regular scar massage may help.
In a small number of patients non-union of your fracture can still occur, even after surgery. This happens to five in every 100 patients, where surgery is completed within four weeks of their injury. Non-union is where the fractured bone fails to heal and mend, even over a long period of time.
Nerve damage can occur during your surgery. This may result in either a painful spot in your scar (called a neuroma), or some numbness around the scar or into your thumb. This often settles within a couple of months.
Complex Regional Pain Syndrome (CRPS). This is a very rare condition but can cause severe pain, swelling, and stiffness in the hand. It can take several months to improve or may even continue. CRPS can often start gradually and may not be noticeable for four to six weeks. If you have ongoing persistent pain and swelling throughout your whole hand after this period of time, please contact the consultant you were under for the surgery for a review, or visit your GP.
Please remember that most patients have an uncomplicated routine operation and are happy with their recovery and outcomes. If you have any questions or concerns about the risks / complications listed above, please speak to your consultant or therapist before your surgery.
How long will I be in hospital?
The operation is carried out as a day case, so you will go home on the same day as your operation. Plan to be in the hospital for up to six hours.
How will I feel after my operation?
You may be in a little discomfort after your surgery, this is normal. However, it is not common to be in large amounts of pain. If you need to, you can take simple painkillers such as paracetamol, but only if you are able to take this kind of medication.
Can I drive after my surgery?
You cannot drive home after your surgery. Please make sure you arrange for someone to take you home after your operation.
Only return to driving when your arm feels comfortable. When you can use it for general daily activities and you can safely control your vehicle. This not usually while it is in plaster, or within six weeks of your surgery.
When can I go back to work?
When you can return to work depends on the work you do. For example, if your job involves light duties, you can return one to two weeks after your surgery. But, if your job involves more demanding work, you may not be able to return for around three to six weeks. Avoid any heavy manual work for eight to 12 weeks. If you are unsure, please speak to your GP or therapist.
If you need a Statement of Fitness to Work (sick note) you should contact your GP. Take this information and any other documentation from the hospital to your appointment. More information is available on the NHS When do I need a fit note? web page.
When can I go back to my normal daily activities?
Avoid any significant weight-bearing activities for the first four weeks following your surgery. This includes pushing-up from a chair or heavy gripping.
Avoid any heavy gripping, pulling, and pushing for the first six to eight weeks after your injury. However, you can use your hand immediately for light activities such as feeding, drinking, dressing, typing, and light housework.
Avoid contact sports for eight to 12 weeks.
Will I need a follow-up appointment?
If you have a confirmed or suspected scaphoid fracture you may be offered a follow-up appointment in the Fracture Clinic. If we feel that you do not need this appointment, you will be given details on how to organise a review yourself, should you have any concerns once you return home.
When will my dressing and stitches be removed?
You will be sent home with your hand in a back slab and bandage. This will remain in place for two weeks. After this, your hand will be in a cast for four to six weeks. This will be managed by the Fracture Clinic staff.
You may have:
dissolvable stitches, which will disappear on their own, or
non-dissolvable stitches, which will need to be removed. These will be removed between 10 to 14 days after your surgery, by either your GP, therapist, or consultant. This will be discussed with you when you have your surgery.
How do I care for my scar?
The length of the scar and number of stitches needed varies between patients. Your surgeon will aim to make your scar look as neat as possible.
Your scar may become sensitive to touch while it heals. It is very important that you massage your scar as soon as you can after surgery. You do this with a small amount of water-based hand cream for up to eight weeks after surgery. This will help to soften the scar tissue and reduce its sensitivity. For more information, please ask a member of staff for a copy of the Trust's Scar massage leaflet.
What should I do if I am concerned about my hand?
Please contact your GP or local Urgent Treatment Centre if you have any of the following.
Loss of feeling in your hand or fingers.
Discoloured skin on your hand or fingers.
Your fingers become hot or cold all the time.
You have increased swelling, tenderness, or pain.
Excessive pain, swelling, or tenderness around your wound, as you may have an infection.