Robotic-assisted laparoscopic prostatectomy: Kent and Canterbury Hospital
Information for patients from the Urology Department
This leaflet has been produced to explain robotic-assisted radical prostatectomy, as a surgical treatment for prostate cancer. This information supports your consultant and specialist nurse consultations.
What is robotic prostatectomy?
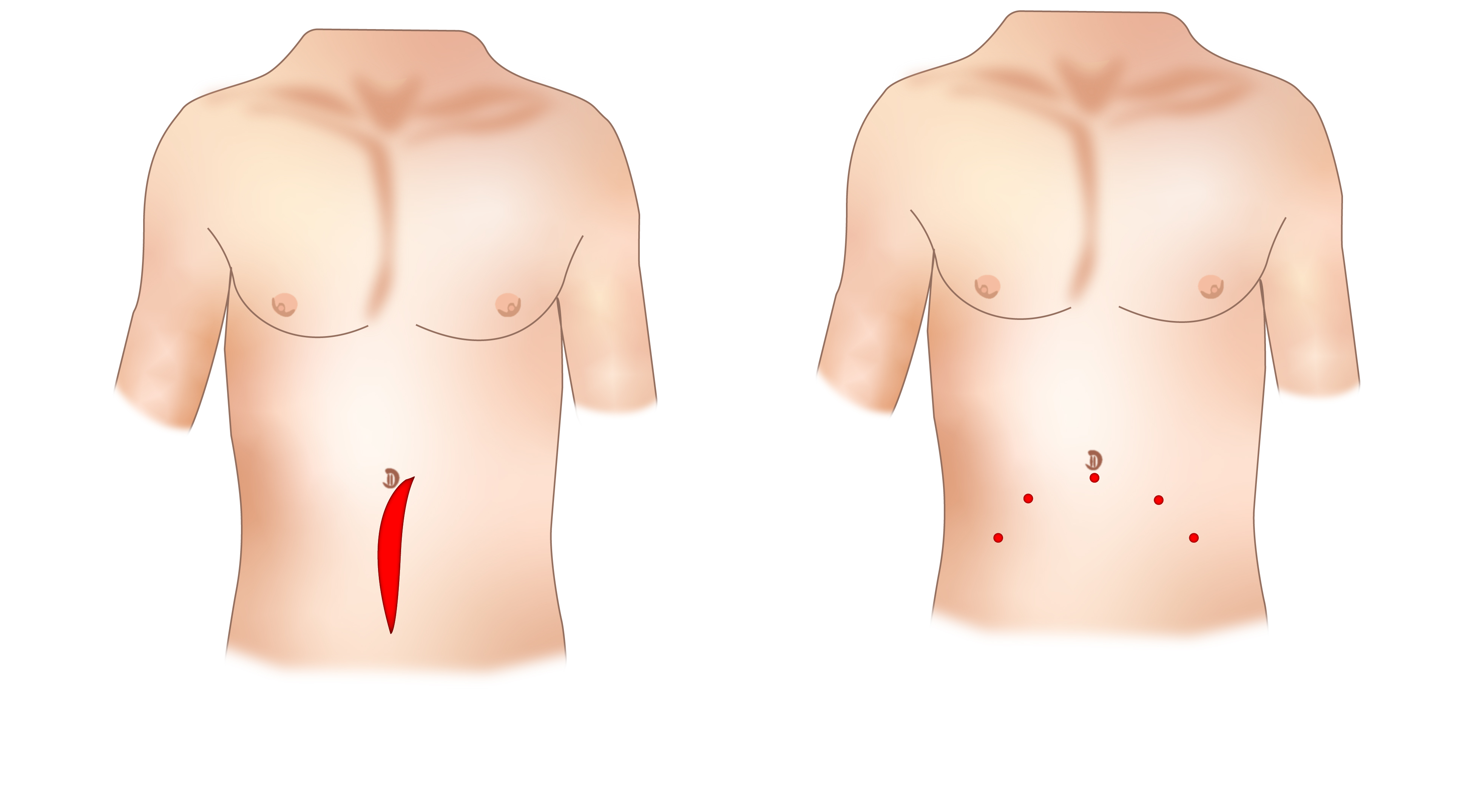
Prostatectomy is the surgical removal of the prostate gland as a treatment for prostate cancer. To do this we now use a surgical robot called the Da Vinci® which enables us to do difficult laparoscopic or keyhole surgery, as opposed to the traditional open surgery. The surgery is performed under a general anaesthetic (you are asleep for the procedure).
.jpg)
The robot is controlled by the surgeon at all times and does not work on its own. The robot is connected to the patient and very small instruments are inserted through small surgical incisions (cuts) in the patient’s abdominal wall. The surgeon sits at a separate console and carries out the operation without touching the patient. The surgeon has complete control of the robot at all times.
Kent and Canterbury Hospital was the first hospital in the South East of England, outside of London, to offer this advanced treatment option.
We are a robotic training centre
We are a national training centre in robotic surgery, and run an international fellowship training programme. The fellow works under the supervision of consultants at all times, and may perform part or all of your surgery.
Is the surgeon able to do the same operation as an open prostatectomy with the robot?
Yes. In terms of cancer treatment it is regarded as the same as open surgery and does not compromise cancer control.
What are the advantages of robotic surgery?
This type of surgery offers many advantages for both you and your surgeon.
Surgical advantages
A highly magnified high definition view of your operation.
A complete 3D view of your prostate when operating.
Much finer more delicate dissection.
Far more precise surgery.
It eliminates tremor.
Patient advantages
Lower complication rates.
Lower infection rates.
Less pain.
Quicker recovery.
Shorter hospital stay.
Shorter catheter time.
Less blood loss and a lower rate of needing a blood transfusion (1% or one in every 100 patients).
Earlier return to work / normal daily activities.
Improved cosmetic result.
Are there any alternatives to this treatment?
Yes. You should have discussed these with your urologist or oncologist. Depending on your age, PSA blood test, type of disease, and other health issues, radiotherapy, brachytherapy, surveillance, or hormone therapy are all treatment options. However this type of surgery is only chosen if we feel it is the most appropriate treatment option for you, and you are happy to proceed.
Are there any complications to having this surgery?
Yes. All surgery has the potential for complications, however robotic surgery minimises these risks. These should be discussed with you by your surgeon before signing the consent form.
Short-term common risks
Bruising in the scrotum and penis and / or around the wounds – wear supportive underwear following surgery for two to three weeks (very common).
More severe bruising across the abdomen, this happens rarely and resolves over the first couple of weeks. It does not necessarily mean there is a problem with the operation (uncommon).
Bladder spasms / pain with catheter (common).
Catheter bypassing – urine may leak down the side of the catheter causing minor leakage, this is common and not a concern.
Constipation – this is important to avoid and you will be given medication for this (uncommon).
Blood in the urine (common).
Urinary or wound infection (uncommon).
Facial swelling lasting a few hours (common).
Shoulder pain lasting a few hours (very common).
Rectal discomfort or a desire to open the bowels which can last for the first hour or two after the operation (common).
A feeling of abdominal bloating or gas inside the abdomen, this can last for a few days after discharge and settles once the bowels are opened regularly (very common).
Short-term rare complications
Bleeding needing transfusion during or after the operation (two in 100 patients).
Return to theatre for complications such as bleeding (one in 200 patients).
Damage to structures around the prostate for example the bowel / rectum / bladder / blood vessels or ureters (tubes between kidney and bladder). Also potential damage to nerve supply to muscles in the leg can occur rarely (less than one in every 100 patients).
Urine leak, this is where urine leaks from the join between the bladder and water pipe. It rarely needs reoperation and just heals up over a few days needing a longer stay in hospital (one in 200 patients).
Risk of clots in the legs (DVT or deep vein thrombosis), or clots on the lungs (PE or pulmonary embolus), again around one in 200 patients. You will have injections to reduce this problem. Keeping well hydrated and early mobilisation / walking helps prevent this problem.
Medical complications such as chest infections or heart attack, again this is rare and is less than one in 200 patients.
Conversion to an open operation – again this is rare (0%).
Readmission to hospital (four in 100 patients).
Urinary retention after catheter removal (three in every 200 patients).
Port site hernias (bowel protruding through wound) (one in 100 patients).
Equipment failure where the operation would be cancelled and rescheduled is rare.
This is major pelvic surgery and as a result there is a risk of death but this is less than one in every 1000 patients.
Removal of lymph nodes
In selected patients with higher grade or higher volume disease, removal of the lymph nodes within the pelvis may be discussed with you. The reason for this is to find out if there has been spread of the prostate cancer to these lymph nodes that is not detectable on scans.
Most patients will not notice any side effects from the removal of the nodes. A small number of patients may have complications related to this part of their operation. These include:
Lymphoceles are collections of fluid in the pelvis. They may cause pain or discomfort which may occasionally need draining (five in every 100 patients).
Lymph leak is where fluid from the lymphatic system is produced that needs drainage from the abdomen, this needs continued drainage at home.
If lymphoedema or swelling of the leg happens patients are referred to the community lymphoedema team. Lymphoedema can last for nine to 12 months and in rare cases is permanent (one in 100 patients).
Damage to pelvic nerves or blood vessels can affect the nerve on the inner thigh, which can cause difficulty when crossing your legs (very rare).
Pelvic Haematomas is a solid swelling of blood in the tissues outside the blood vessels.
Most of the above problems would be identified by your medical team before your discharge from hospital or at your follow-up appointments.
If you are at all concerned, please use the contact numbers listed at the end of this leaflet or on your discharge leaflet.
Long-term complications
Incontinence - continence can be affected by this treatment. However, long term (longer than a year) incontinence that needs further surgery happens in two to three in every 100 patients. The majority of patients will have some incontinence when their catheter is removed and may need to use incontinence pads for a period of time. With robotic surgery continence recovers quicker.
It is important to do your pelvic floor exercises before, during, and after your recovery. You will be given written information regarding pelvic floor exercises. The community physiotherapists will help in this area, and an appointment will automatically be made for you.
Patients who already have pre-existing stress urinary incontinence and / or urge incontinence are at a higher risk of needing pads long term after surgery.
The table below outlines continence recovery. This is taken from our own audited results.
| Time since surgery | % of patients that are pad free |
|---|---|
| one week | 29 to 30% |
| six weeks | 45 to 50% |
| 12 weeks | 65 to 75% |
| 26 weeks | 75 to 85% |
| 52 weeks | 90 to 95% |
Erectile dysfunction - erections will be affected by this surgery. This is more likely in older age groups and if you have weak erections before your surgery. In patients who want to regain their erections there may be the possibility that we can offer nerve sparing technique. This is part of the operation where we protect the nerves that go down to the penis, these run very close to the prostate and can be gently peeled off. We do not offer this in patients with more advanced disease; your surgeon will discuss this with you if appropriate.
Even with nerve spare surgery, erections are not guaranteed. You will be offered a daily tablet to help with recovery. Spontaneous recovery that is going to happen can take up to two years, although we have dedicated clinics for erectile dysfunction that we can refer you to after your surgery.
Some patients will notice a degree of penile shortening. In rare cases this can be severe and permanent.
Urethral / Anastomotic strictures (scar tissue that forms in the water pipe).
Patients may notice a slowing of urinary flow or struggling to pass urine. It can occur soon or many months after the operation. Anastomotic strictures have occurred in one in every 200 of our patients. Sometimes it needs a minor operation to treat it.
Will I lose my desire / libido after surgery?
No. The operation should not affect your libido. It will affect your fertility though. You will have no ejaculate following your operation and in some men they notice a small degree of penile shortening.
When can I start sexual relations?
There is no restriction on resuming sexual relations after the catheter is removed, once you and your partner are happy to do so.
Can the robot breakdown?
Potentially, although this very rarely happens (less than one in every 200 operations). If this happens either your operation can be rescheduled or it can be done as an open operation. Over 4000 robots are being used worldwide and this has only been reported in a handful of cases. We have had to cancel operations on the day of surgery due to equipment failure when testing before surgery, but then rebooked patients onto the next available surgical list.
What happens now?
Once we have decided on robotic surgery:
You will be contacted with a date for your operation.
You will be asked to come to the Preassessment Clinic at Kent and Canterbury Hospital, where routine bloods tests and an ECG (heart tracing) are taken, and an assessment of your fitness for surgery is made.
You and your wife / partner will be invited to a ‘Patients Forum’; this is a group that meets once a month and discusses issues surrounding your surgery, such as continence, physiotherapy, and erectile function.
You will be admitted to the hospital (Clarke Ward, Kent and Canterbury Hospital) on the morning of your operation. You will meet your surgeon, anaesthetist, and nursing staff.
You will be asked to sign the consent form. Remember you can withdraw your consent for treatment at any time.
You will be given an enema before your operation, to make sure your bowels are clear.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
How long does the operation take?
The operation takes two to three hours. It is done under general anaesthetic (you are asleep for the operation). You will wake up in the recovery bay before being transferred back to the ward.
Will I be in pain?
Robotic surgery is less painful than open surgery. Before you wake up the anaesthetist will give you pain relief and we use local anaesthetic (numbing solution) in your wounds and bladder. If you are in pain, please tell the nursing staff so they can give you pain relief.
A lot of patients wake up feeling as though they have a full bladder or get bladder spasms, this is because of the catheter and the surgery around your bladder, not because your bladder is full. This usually settles but if not can be helped with medication.
The anaesthetist may consider giving you a spinal injection before your surgery, to help control any pain afterwards.
How long will I be in hospital?
One day. The majority of patients are discharged the day after their operation. Along with the catheter, you will wake up with a drain tube which is removed before your discharge from hospital. You will also be taught how to give yourself a small injection each day for four weeks, to help prevent clots forming in the veins in your legs.
How can I help prevent blood clots (DVT or deep vein thrombosis)?
To prevent clots you will be taught how to give yourself an injection in to your stomach; you will need to do this each day for 28 days after your surgery. You will be taught how to do this on the ward before you leave hospital.
You will also be given surgical stockings to wear for a time after surgery.
Will I have help after I am discharged from hospital?
Yes.
Before leaving hospital you will be given instructions on how to manage your catheter and wound dressings.
Absorbable stitches are used so no stitches need to be removed.
You will be given painkillers to take as and when you need them, tablets to stop gastritis (stomach irritation) to be taken for the first week, and medication to prevent constipation.
For men whom erectile function is important, a medication will be offered. This should be started once the catheter is removed.
If needed the community nurse is available (contact details are available via your GP).
The Community Continence Team are available and you can refer to them for support.
The ward can be called if there are any problems.
See useful contact numbers at the end of this leaflet.
How do I look after myself at home?
To start with exercise should be gentle but gradually built up each day, as your symptoms allow.
Do not stay in bed all the time.
You should take a full and balanced high fibre diet and drink plenty of fluids, especially in the first week after your surgery.
Do not drink alcohol for one week after your surgery.
Energy levels can vary from day to day following surgery.
How long will I need a catheter for?
The catheter is a very important part of your recovery. It protects the join between your bladder and your urethra (water pipe) in the early stages of healing. We like to leave the catheter in place for as short a time as possible, between 7 to 10 days after your operation.
Removal of the catheter is very straight forward and only takes a matter of seconds.
Patients are encouraged to remove the catheter themselves at home.
This is a very safe and painless procedure. It will be demonstrated at our Prostate Forum and by the ward nurses before discharge.
Before you are discharged from hospital, we will give you a date to remove your catheter. A telephone appointment will be made for that day. A member of the team will call you before and after you remove your catheter, to make sure this went well.
Your surgeon may decide to leave your catheter in for longer. If this is the case, your surgeon will explain the reasons why.
Once the catheter is removed, please continue doing your pelvic floor exercises regularly.
Remember that to start with, most patients have some leakage once their catheter is removed and you may need to use pads for a period of time. This is where the Kent Continence Service will help you.
When do I get my results?
It takes our pathologists about two weeks to process and examine your prostate. You will discuss the results with your surgeon at your follow-up appointment.
Will I need any other treatment?
Most patients do not need any other treatment. However some patients with more advanced disease may be offered radiotherapy either immediately after their surgery, or later if there is a rise in their PSA levels. Others may be given a long course of hormones. Your surgeon will discuss this with you. Further appointments with the oncologists may be needed in this situation.
Will I have follow-up appointments?
After your initial pathology results you will be seen by your surgeon six weeks after your surgery, and then every three months to check your PSA levels. If all is well, then the time between your appointments can be lengthened. You may also have appointments with the physiotherapist to make sure your pelvic floor muscles are recovering. Erectile dysfunction will be discussed at a specialist clinic, if this is important to you.
When can I drive?
This varies between patients. You will only be fit to drive if you can do an emergency stop without it causing pain. Please wait at least one week before driving again.
When can I return to work?
Again this varies between patients. You can return to work when you feel able. Some patients are back to work after one week, others take three to four weeks. It is important to only do light duties to start with and to do no heavy lifting for four weeks.
We have found that after robotic surgery patients return to work quicker, on average at three weeks compared to 11 weeks after open surgery.
When can I fly?
You can fly on short haul flights from two weeks after your surgery, and long haul flights from four weeks. These are recommendations, if you have any concerns please delay your travel. You must also check with your carrier and travel insurance company.
What can we do to improve our service?
We are constantly trying to improve the high quality care we provide. We continually audit and assess our results. We will ask you to fill out questionnaires on your continence, erectile dysfunction, and overall quality of life. We would like you to fill these out before your operation and at all your follow-up appointments. We also want you to record the first day you manage without pads and when you return to work. Please let us know these dates at your follow-up appointment or by email.
All this information is handled sensitively. Please feel free to add any other comments, whether good or bad. All these comments will be taken seriously and will be used to improve the experience for future patients.
Where can I get further information about my operation?
Useful contact numbers
Macmillan Urology Cancer Nurse Specialists
Telephone: 01227 868666
EmailMacmillan Urology Support Workers
Telephone: 01227 868666
EmailClarke Ward, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783103Kent Continence Service
Telephone: 0300 123 3167Prostate Cancer UK
Telephone: 0800 074 8383Macmillan Cancer Support
Free helpline: 08088 080000
Practical, financial, and emotional support for people with cancer, their family and friends. Macmillan also has further information on sex, relationships, and cancer.Sexual Dysfunction Association
Helpline: 08707 743571
For support and information on erectile dysfunction