Robotic-assisted colorectal surgery
Information for patients from the Colorectal Department
This leaflet explains robotic colorectal surgery, as a surgical treatment for bowel cancer. It covers the following.
What robotic-assisted colorectal surgery is.
What the advantages are to having robotic-assisted surgery
What the alternatives are.
What happens before, during, and after surgery.
What the risks are to having this surgery.
How to look after yourself when you return home.
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
What is robotic-assisted colorectal surgery?
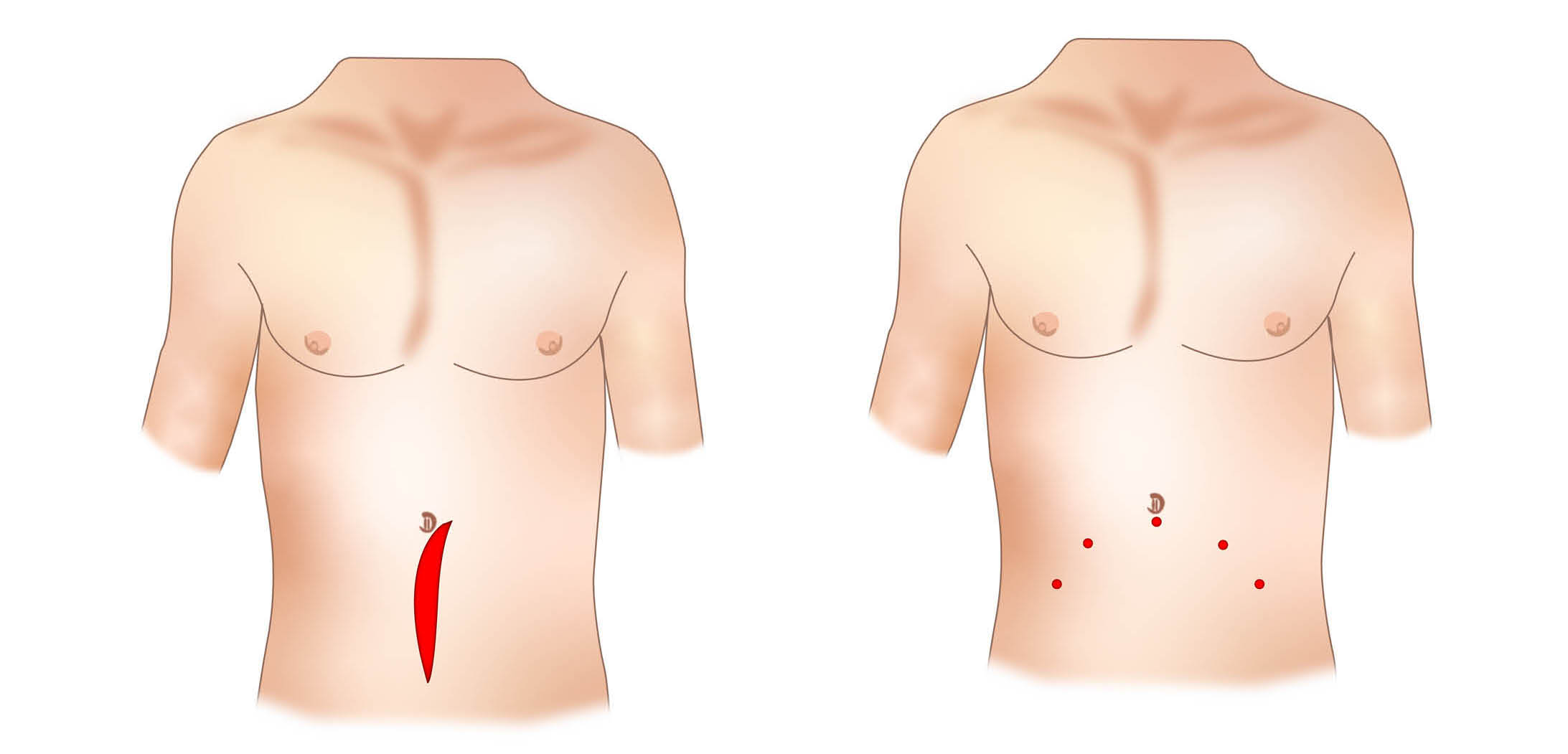
Robotic-assisted colorectal surgery is a minimally invasive “keyhole” surgery. It is used to remove part of the large bowel.
During the procedure, the surgeon does not hold the instruments directly, instead they sit at a console. The robot is controlled by the surgeon at all times. It does not work on its own.
The robot is connected to the patient. Very small instruments are inserted through small surgical incisions (cuts) in the abdominal wall. The surgeon sits at a separate console and carries out the operation without touching the patient. It is important to know that the robot does not perform the surgery on its own. Your surgeon has complete control at all times.
Is the surgeon able to do the same operation as an open or laparoscopic procedure with the robot?
Yes. In terms of cancer treatment, it is regarded as the same as open surgery. It does not compromise cancer control.
Can the robot breakdown?
This happens in less than 1 in every 200 operations. If this happens, either your operation can be rescheduled or it can be done as an open or laparoscopic operation.
What are the advantages of robotic surgery?
This type of surgery offers many advantages for both you and your surgeon.
Surgical advantages
A highly magnified high definition view of your operation.
A complete 3D view of your bowel when operating.
Much finer, more delicate dissection.
Far more precise surgery.
It eliminates tremor.
Patient advantages
Lower complication rates.
Lower infection rates.
Less pain.
Quicker recovery.
Shorter hospital stays.
Less blood loss and a lower rate of needing a blood transfusion (1% or one in every 100 patients).
Earlier return to work and other normal daily activities.
Improved cosmetic result.
Are there any alternatives to this treatment?
Yes. Depending on your age, type of disease, and other health issues there may be other options. However, this type of surgery is only chosen if we feel it is the most appropriate treatment option for you, and you are happy to proceed. You should discuss any alternatives with your surgeon or oncologist before any decisions are made.
Are there any risks to having this surgery?
Yes. All surgery has the potential for complications. However, robotic surgery minimises these risks. Your surgeon will discuss the following risks with you, before they ask you to sign a consent form.
General surgical risks
These risks are common to most major surgical procedures, regardless of the technique used.
Infection can occur at the incision sites or in the abdomen. Proper surgical technique and post-operative care are used to minimize this risk.
Minor bleeding and bruising around the incision sites are common.
Major internal bleeding is rare, but may mean that you need to have open surgery.
A port-site hernia can develop at the location of an incision.
Colorectal specific surgical risks [1]
Anastomotic leakage is a life-threatening complication. This is where the internal connection made after removing the cancerous section of bowel, does not heal properly and leaks. In some cases, a temporary stoma may be created to reduce the risk of this happening.
The bowel can become blocked by scar tissue or other issues. If this happens, some patients will need more surgery.
Changes in bowel habits are common, but typically resolve over time. Changes include diarrhoea (poo is loose / runny and watery) and constipation (not pooing as often or finding it hard to poo).
There is a risk of nerve injury in the pelvic area, that controls urinary and sexual function.
Robotic specific risks
Failure of the robot (very unlikely).
A traction (pulling) injury to the bowel or blood vessel inside the body. This would be repaired immediately.
Major bleeding is rare, but may need conversion to open surgery.
Factors influencing risk
Your individual risk can be affected by a number of factors.
The surgeon's experience with robotic procedures.
Your body mass index (BMI).
The stage of your cancer, and if other organs are involved.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of:
medical treatment
test; or
examination.
Consent is usually given when you sign the consent form before your treatment. We may ask you to give your consent verbally (spoken rather than written consent).
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. Please speak to staff if:
staff have not given you this information; or
they have but you still have questions.
You must be capable of giving consent. This means you understand the information given to you, and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
What happens before my surgery?
Pre-assessment appointment. Before the day of your surgery, you will have an appointment to check you are fit for surgery. The pre-assessment team will give you specific instructions on what you need to do before your operation.
Bowel preparation. For some bowel surgeries you will be asked to follow a special diet and take a laxative to empty your bowel. If you need to do this, the nurse will tell you at your pre-assessment appointment.
Meeting the team. Before your surgery, you will meet a member of your surgical team. If you are having a stoma, you will also meet a stoma nurse. Please ask any questions.
What happens on the day of my surgery?
Arrival. Most patients are asked to come to the hospital on the morning of their surgery. Please refer to your appointment letter for more information.
Anaesthetic. The operation is performed under a general anaesthetic. You will be asleep and will not feel any pain.
The procedure. Once you are asleep, the surgical team will make a few small cuts. The team will use the robot to remove the section of the bowel containing the cancer.
Lymph nodes. Your surgeon will remove some nearby lymph nodes.
Tumour removal. The part of the bowel containing the tumour will be removed through one of the small incisions. A slightly larger incision may be needed.
What happens after my operation?
Recovery. You will be moved to a recovery ward to wake up. Nurses will monitor you and help you manage any pain.
Getting moving. A key part of your recovery is getting out of bed and walking around as soon as possible. This helps your recovery and reduces the risk of blood clots.
Eating and drinking. Your team will tell you when you can start eating and drinking again.
Hospital stay. How long you stay in hospital will depend on how well you recover. Minimally invasive surgery can significantly shorten your time in hospital.
Discharge. You will be given instructions on how to care for your wounds and manage your pain at home. A follow-up appointment will be arranged.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
How long does the operation take?
The operation takes 3 to 4 hours.
Will I be in pain?
Robotic surgery is less painful than open surgery. Before you wake up:
the anaesthetist will give you pain relief; and
we use local anaesthetic (numbing solution) in your wounds.
If you are in pain, please tell the nursing staff so they can give you pain relief.
The anaesthetist may consider giving you a spinal injection before your surgery, to help control any pain afterwards.
How long will I be in hospital?
Most patients stay in hospital between 2 and 7 days. However, some patients go home earlier.
You will wake up with a catheter, and some patients also have a drain tube. These are removed before your discharge from hospital.
How can I help prevent blood clots (DVT or deep vein thrombosis)?
To prevent blood clots, you will be taught how to give yourself an injection into your stomach. You will need to inject yourself each day for 28 days after your surgery. You will be taught how to do this on the ward before you leave hospital.
Will I have help after I am discharged from hospital?
Yes.
Before leaving hospital, you will be given instructions on how to manage your wound dressings.
Absorbable stitches are used, so no stitches need to be removed.
You will be given:
painkillers to take as and when you need them
tablets to stop gastritis (stomach irritation) to be taken for the first week; and
medication to prevent constipation.
If needed, the community nurse is available. The nurse's contact details are available via your GP.
Call the ward if you have any problems. See the useful contact numbers at the end of this leaflet.
How do I look after myself at home?
To start with, exercise gently. Build up gradually each day, as your symptoms allow.
Do not stay in bed all the time.
Eat a full and balanced high fibre diet and drink plenty of fluids. A good diet is especially important in the first week after your surgery. Please refer to the NHS web site for advice on eating a healthy diet.
Do not drink alcohol for 1 week after your surgery.
Following surgery, energy levels can vary from day to day.
When do I get my results?
It takes our pathologists about 2 weeks to process and examine the removed parts of your bowel. The results will be discussed at a multidisciplinary meeting. After this meeting, you will be contacted by either your surgeon or cancer nurse to discuss the results.
When can I drive?
This varies between patients. You will only be fit to drive if you can do an emergency stop without it causing pain. Please wait at least 1 week before driving again. Arrange for someone to take you home from hospital.
What if I have any questions or concerns?
If you have any queries or concerns, please contact Day Surgery on the numbers below or your GP.
Canterbury Day Surgery Centre, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783114 (7.30am to 8pm)
Telephone: 07887 687645 (8pm to 7.30am)Day Surgery, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234499 (7.30am to 8pm)
Telephone: 07887 651162 (8pm to 7.30am)Channel Day Surgery, William Harvey Hospital, Ashford
Telephone: 01233 616263 (24 hours a day, 7 days a week)
References
Sampat MH & Elgaddal S. A review of local consent practices for colorectal surgery with a focus on postoperative bowel dysfunction. Cureus 2025: 17(6); e86286.
[Websites last accessed 2nd October 2025]
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email