Reverse Total Shoulder Replacement
Information for patients from the Trauma and Orthopaedics (T&O) Department
You have been diagnosed with a condition that may need surgery called reverse total shoulder replacement. This leaflet will explain what this surgery involves. It will also provide you with information about what you need to do through the process.
If after reading this leaflet you still have questions or concerns, please speak to your surgeon or anaesthetist at your next appointment.
Contents page
What is shoulder osteoarthritis with rotator cuff disease?
What are the signs / symptoms of shoulder osteoarthritis with rotator cuff disease?
How can I help myself?
What are the treatment options available?
What is reverse shoulder replacement surgery?
Why reverse the anatomy?
Which patients can have a reverse shoulder replacement?
What are the different types of reverse shoulder replacement?
What is the bone-preserving reverse shoulder replacement?
What is computer-assisted shoulder surgery?
Patient specific instruments
How can I prepare for my surgery?
What happens on the day of my surgery?
What kind of anaesthetic will I need?
What are the complications and risks?
How long will I stay in hospital?
Will I be in pain after my surgery?
What painkillers will I be sent home with?
How do I care for my wound at home?
How long will my wound(s) take to heal?
What if my wound bleeds at home?
Can I have a bath or shower?
Why am I wearing a sling after my surgery?
What is the best position to sleep in?
When can I drive again? When can I return to work?
When can I start my normal activities?
When should I start noticing improvement?
Will I have a follow-up appointment?
What if I have any questions or concerns?
Exercises and physiotherapy advice
Contact details
What is shoulder osteoarthritis with rotator cuff disease?
The shoulder is a ball (humeral head) and socket (glenoid) joint, which is surrounded by a group of tendons and muscles called the rotator cuff. These muscles and tendons are important in performing shoulder tasks (such as lifting your arm over your head), and keeping the ball of the ball-and-socket shoulder joint centred. Together, the joint and the structures around it allow a large range of movement in your shoulder.
The joint sometimes needs replacing due to wear and tear (or osteoarthritis). Usually, this happens when severe osteoarthritis affects the joint surfaces, and the shoulder becomes painful and difficult to move. Other reasons are complete loss of the rotator cuff tendons, resulting in loss of movement, or an injury or fracture that damages the shoulder joint badly.
-
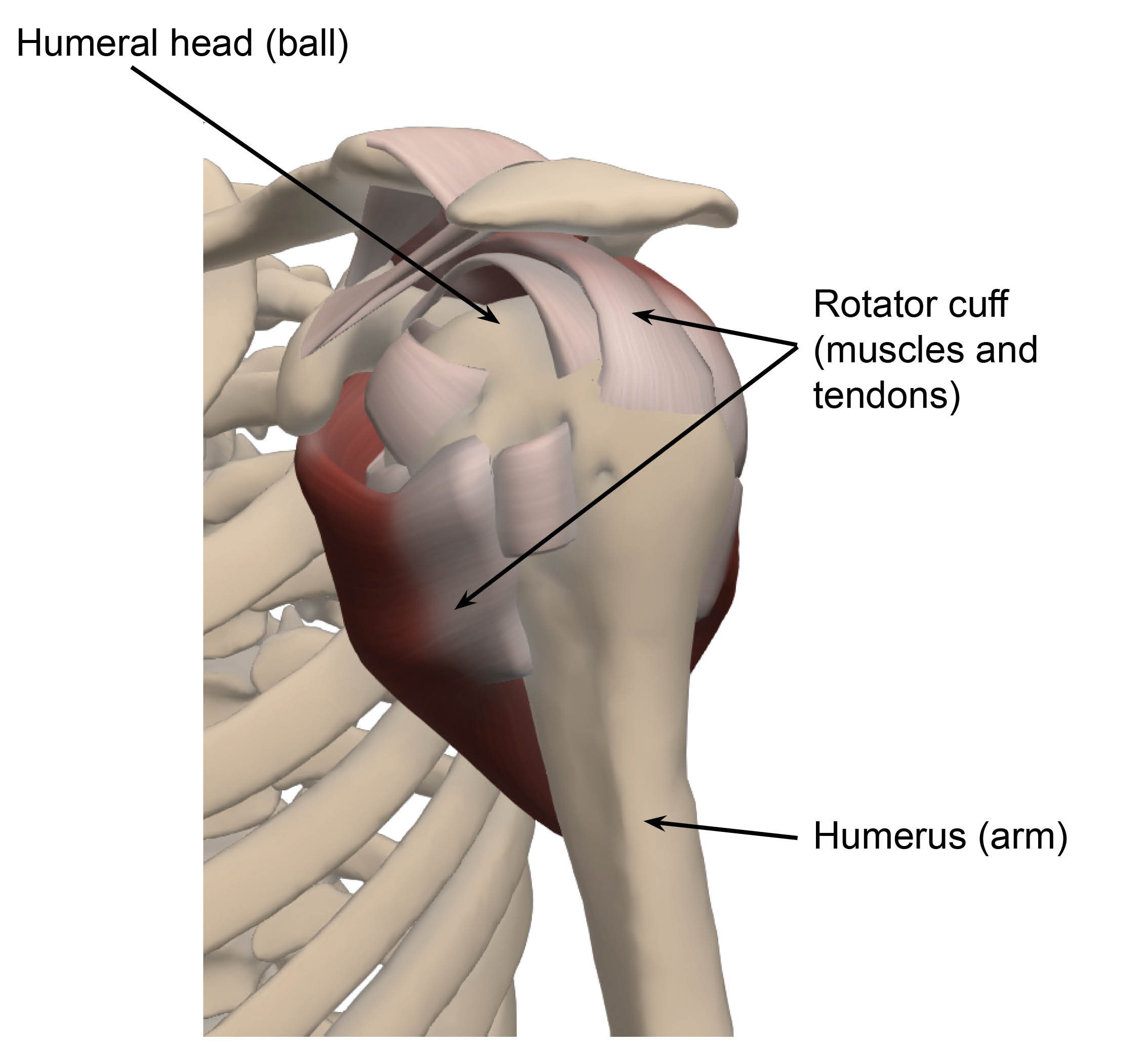 The shoulder and rotator cuff tissue
The shoulder and rotator cuff tissue -
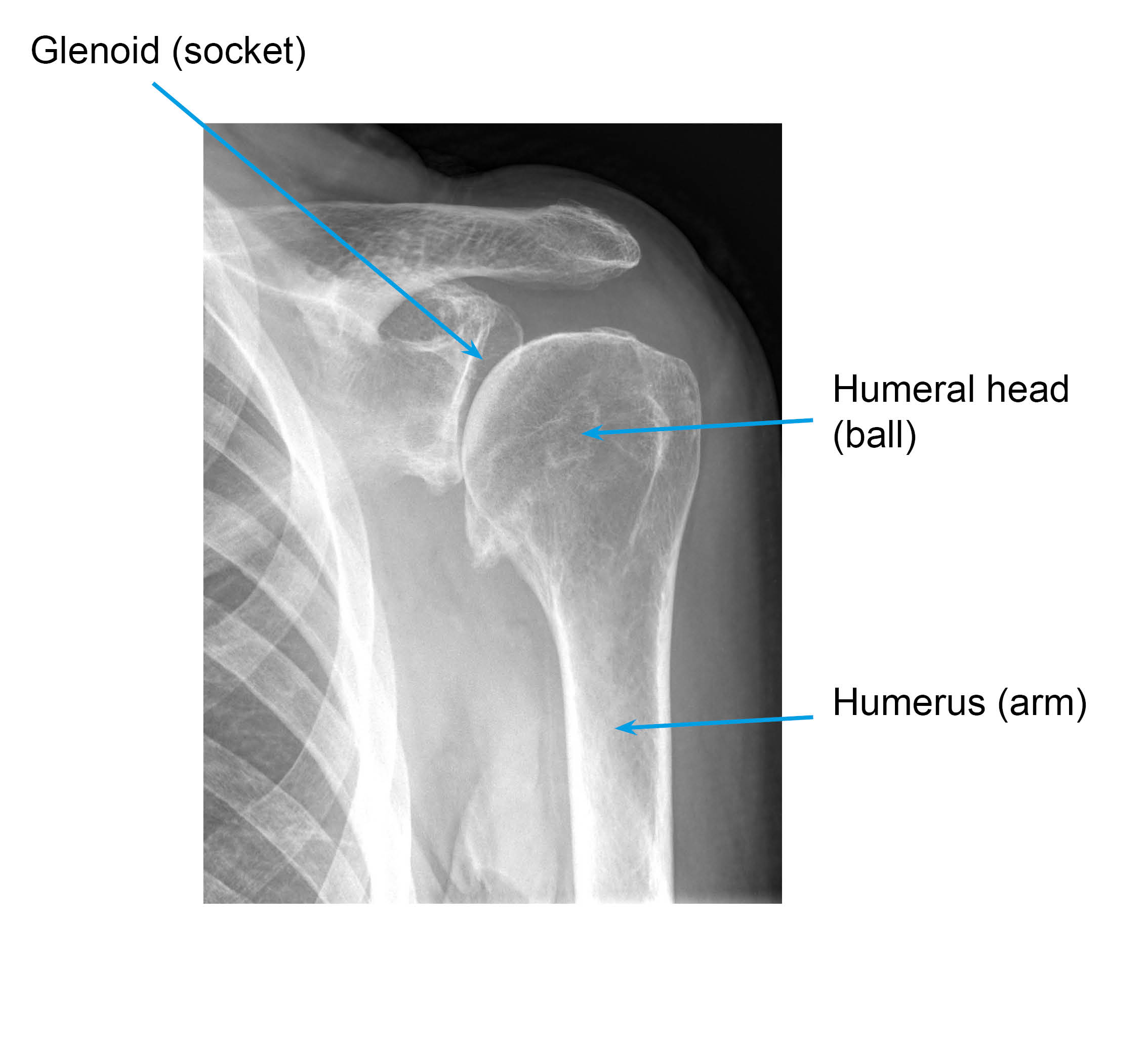 X-ray showing a shoulder with osteoarthritis: decreased joint space and bone growth around the edges of the joint due to wear and tear
X-ray showing a shoulder with osteoarthritis: decreased joint space and bone growth around the edges of the joint due to wear and tear
What are the signs / symptoms of shoulder osteoarthritis with rotator cuff disease?
Pain, usually felt in the shoulder area.
Difficulty sleeping on the affected side, due to pain.
Sometimes you may experience neck pain with your shoulder pain.
It may feel like something in your shoulder is catching, popping, or clicking when you move your arm in certain directions, this may be painful.
Weakness.
Loss of movement and function.
How can I help myself?
When your shoulder hurts, you can place a bag of frozen peas wrapped in a damp tea towel over your shoulder for 10 minutes at a time; this may help to reduce the pain and inflammation (redness, heat, and swelling). Do not use these peas for eating once they have defrosted.
Try to improve your posture (how you sit); hold your back straight and your shoulders back.
If your symptoms get worse with daily life activities, try to make simple changes to avoid pain. If your symptoms are made worse by a sport you may benefit from advice from a coach / instructor regarding your techniques.
Help keep the available movement in your shoulder, by moving your arm through the available comfortable range of movements.
What are the treatment options available?
If you would like to avoid surgery, at least for the time being, you can keep your pain under control with painkillers (paracetamol and / or codeine) and/or anti-inflammatory medication (ibuprofen).
Also, it may help if you make simple changes to your daily routine and carry out physiotherapy exercises.
You could also have a steroid injection to your shoulder to keep the pain under control temporarily.
If none of the above options work for you, surgery could be an option.
All the options available to you will be discussed with you before your treatment plan is decided.
What is reverse shoulder replacement surgery?
The reverse shoulder replacement was designed for shoulders with osteoarthritis and rotator cuff problems.
In a traditional shoulder replacement, the ball of the top of the arm bone (the humeral head) is resurfaced or replaced with a metal ball implant. The socket of the shoulder blade (glenoid) may be kept or replaced with a plastic implant. When the rotator cuff is completely lost, it causes the implant to move abnormally resulting in unusual forces on the artificial joint. If a traditional shoulder replacement is used in these circumstances, it leads to a poor functional result and early failure of the replaced joint.
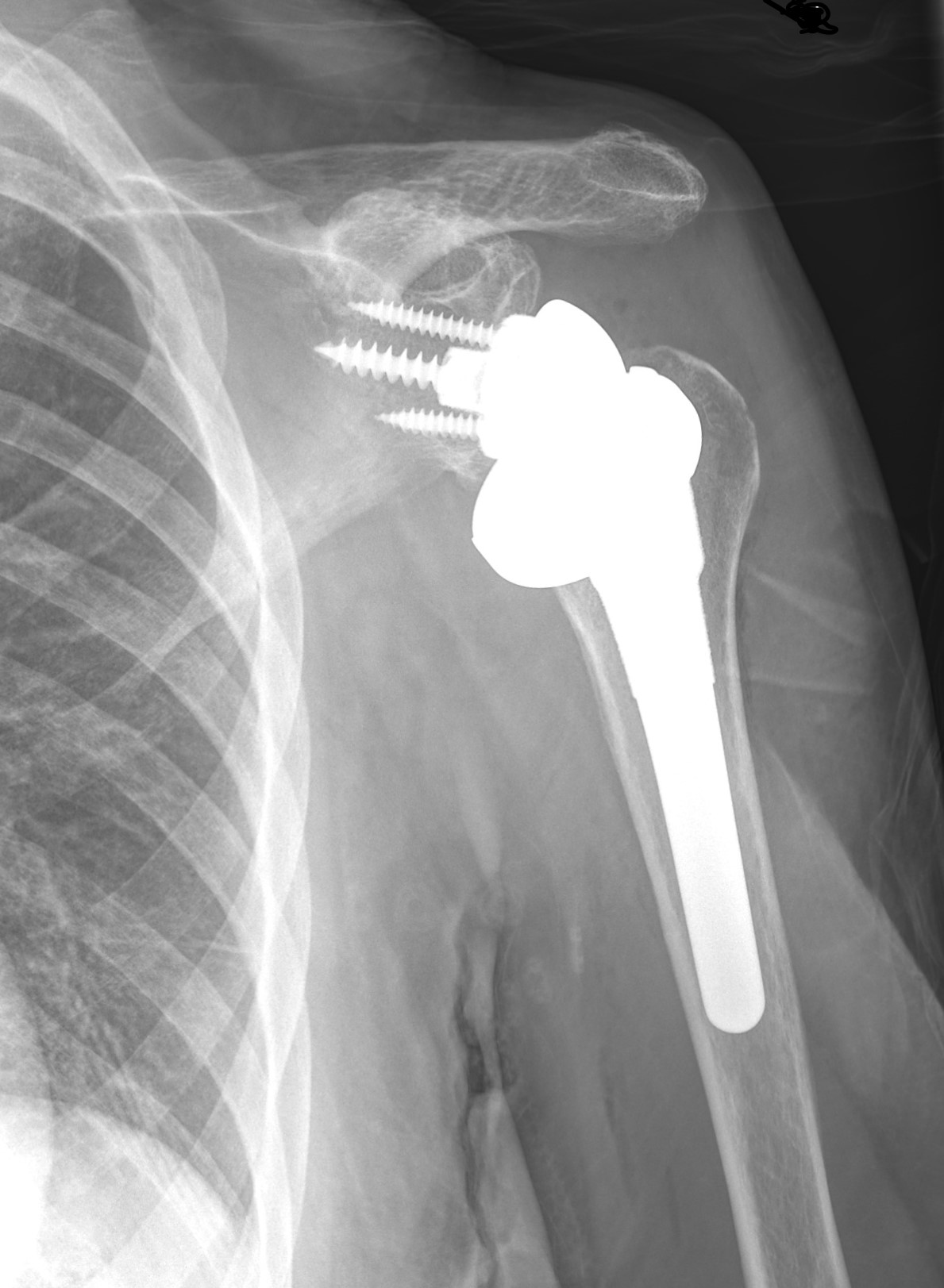
The reverse shoulder replacement uses a ball-and-socket joint as well, but the ball is placed on the shoulder blade, and the socket is placed on top of the arm bone. This is the reverse of our normal anatomy, which explains the surgery’s name.
Nowadays, most prosthesis have a special coating that allows the bone to bond onto the prosthesis over 12 weeks. This avoids the use of bone cement and the issues or complications it might cause.
To do the surgery, the surgeon will make a 10 to 12cm cut at the side of your shoulder. Your wound will probably be closed with dissolvable sutures; these sutures are absorbed by your body. However, the knots at the end of the sutures need to be removed 10 to 14 days after your surgery.
Why reverse the anatomy?
The reverse shoulder replacement is designed for patients who do not have a working rotator cuff, and therefore do not have “normal” shoulder anatomy. By reversing the ball and the socket, the large deltoid muscle, which forms the shape of the shoulder, works better and the patient is able to lift their arm up over their head, to compensate for the torn rotator cuff.
Which patients can have a reverse shoulder replacement?
Patients who can have this surgery have a lot of pain from shoulder osteoarthritis, a rotator cuff tear that cannot be repaired or rotator cuff muscles that do not work, and have a working deltoid muscle. Patients who do not have this combination of conditions can usually have other surgeries to help with their problem.
Patients interested in having this procedure should discuss all of their options with their orthopaedic surgeons. A reverse shoulder replacement should only be performed if simpler, non-operative treatments have not helped with your symptoms.
What are the different types of reverse shoulder replacement?
Reverse shoulder replacement includes a humeral component implant (arm component) and a glenoid implant component (shoulder blade component). The humeral component implant traditionally has a stem, which is inserted into the humeral shaft. However, bone-preserving humeral components implants (short stem or stemless) are becoming more popular.
What is the bone-preserving reverse shoulder replacement?
A bone-preserving reverse shoulder replacement has a special base plate and ball for the shoulder blade, and a short stemmed (stemless) socket for the top of the arm bone. It follows the basic principles of reverse replacements, but it is inserted wasting only a minimum amount of bone (to keep as much good bone stock as possible in case you need surgery in the future) and causes less bone erosion over the longer period.
Please note that this implant is not suitable for all patients and this will be discussed with your surgeon.
What is computer-assisted shoulder surgery?
Occasionally, the operation may need help from a computer; this is known as computer-assisted surgery. This is usually needed when the bone loss is advanced, as computer-assisted surgery will help to make the surgery more accurate.
Before your operation you will need a CT scan of your shoulder. You will need to lie down in a scanner for about 10 to 15 minutes.
This technology will allow us to position your implants more accurately with the help of the computer systems.
Once surgery is complete, recovery will follow guidelines for a standard shoulder replacement.
Patient specific instruments
In cases of significant bone loss and where navigation is not possible, your surgeon will use the images taken during your CT scan and with the help of a 3D printer, will create guides specific to your personal anatomy. These guides will permit the accurate implantation of your new shoulder.
This will not change anything in the procedure and there will be no differences in your rehabilitation. However, there will be a slight delay before your surgery to allow for the 3D printing and preparation of the instruments.
How can I prepare for my surgery?
You will have a preassessment appointment before your surgery, to check if you are ready and fit for surgery. You will also be swabbed for MRSA and Covid-19, if necessary.
Before surgery it helps if you try to get as fit as possible to avoid anaesthetic risk and / or failure of the surgery. It is important that you lose weight if you are above your ideal weight.
Smoking advice
It is important to stop smoking at least 30 days before your surgery. Studies have shown that wound healing is significantly delayed by smoking/nicotine, and the infection rate is much higher. Smoking also harms how your tendon heals following a repair, so smoking after your operation is also not advised.
If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
How does eating a healthy diet help my recovery?
Recovering from surgery can take a long time and it is normal to get frustrated and anxious. But remember that while you are recovering, there are some things you can do to help your wound to heal. We suggest limiting the amount of alcohol you drink, stopping smoking, eating a healthy diet, drinking plenty of fluids (especially water), and staying active. If you need any extra support, do not hesitate to get in touch with us on the contact numbers listed at the end of this leaflet.
Some painkillers (especially those containing Codeine) can cause constipation. To avoid this, please follow a healthy well-balanced diet rich in fruit, vegetables (including green leafy vegetables), nuts, seeds, wholegrains, and legumes, which contain the necessary fibre, and drink plenty of water. More information is available on the NHS 5 A Day: what counts? web site.
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
What happens on the day of my surgery?
Please arrange for someone to pick you up from the hospital after your surgery, as you will not be able to drive yourself. Please make sure to arrange this before your surgery.
To avoid complications with your anaesthetic, you should not eat anything for six hours before your surgery, or drink anything for two hours. You will be given further instructions during your preassessment.
On the day of your surgery, you can take your usual medication as advised during your preassessment. If possible, do not take non-steroidal anti-inflammatory medication, such as ibuprofen and naproxen, for at least 10 days before your surgery, as they can affect how your wound heals. Please bring any medications that you are taking into the hospital with you.
If possible, please wear loose-fitting clothes, as after surgery you will be wearing a sling.
Bring your appointment letter with you, so you know which department to come to when you arrive at the hospital.
At arrival, you will be asked to put a hospital gown on, and maybe a pair of compression stockings.
You will see the anaesthetic and surgical team before your surgery to go through the consent form and discuss any questions you may still have. Remember you can withdraw your consent for treatment at any time.
You may be tested for Covid-19. All appropriate precautions will be taken during your admission to minimise the risk of contracting the illness as per Healthcare England Guidelines.
What kind of anaesthetic will I need?
This procedure is usually performed under general anaesthetic (you will be asleep for the procedure). However, you may be offered the option of “awake anaesthesia” during your surgery to avoid putting a tube into your windpipe. This may be discussed and decided with you and the anaesthetist on the day of your surgery. Should you be suitable for this type of anaesthesia, it is important to understand and be assured that you will be kept comfortable, and you will not feel any pain during your procedure. Patients describe their experience after this type of “awake anaesthetic” as if waking up from a usual night’s sleep, as it is often supplemented with some light sedation. If you need any more information, please speak to your anaesthetist before your procedure.
In addition, a local anaesthetic or nerve block is used during your operation. As a result, your shoulder and arm may feel numb for a few hours after your operation. It is important to take your pain medications during this time, to allow a gentle and easier control of pain when the nerve block wears off and your shoulder is likely to be sore and uncomfortable.
What are the complications and risks?
As with all surgery, there are a few risks and complications. These are rare and will be discussed with you before your surgery.
Anaesthetic risks will be discussed with your anaesthetist on the day of your surgery.
Infection: we do everything we can to avoid this but an infection might still happen. If your wound becomes increasingly red or swollen after your surgery, please contact your GP or your surgical team for advice as soon as possible.
Bleeding: we will do our best to stop this as soon as possible, but some oozing may happen after your surgery.
Deep vein thrombosis (DVT) and / or pulmonary embolism (PE). These are blood clots which form in the blood stream and can be serious conditions. Compression stockings and other measures might be taken by the hospital to avoid them.
Soft tissue (nerve / tendon / blood vessel) injury could happen during surgery. We will try our best to avoid any damage.
Continued pain and Chronic Regional Pain Syndrome (CRPS). This is a condition where a person feels persistent, severe, and debilitating pain. Although most cases of CRPS are triggered by an injury, the resulting pain is much more severe and long-lasting than normal.
Stiffness / loss of movement that may cause frozen shoulder (your shoulder is painful and stiff for up to several months beyond the usual period expected for the stiffness to recover from a simple procedure). This could be avoided or improved if you take adequate pain relief and do the exercises listed at the end of this leaflet as your pain allows.
Numbness / tingling in your arm; this should resolve itself after a few months. We advise you to speak to your surgeon at your follow-up clinic appointment.
Fracture to the bones (humerus and shoulder blade) surrounding your shoulder joint.
Dislocation is when the artificial ball comes out of the socket after a replacement surgery. If this happens, you should go to the Emergency Department.
Loosening and / or wear of the replacement components can happen after your surgery; this is usually is a long-term complication.
The surgery may not be successful. If your surgeon is unable to complete your surgery successfully or the implants fail, other options or further treatment can be discussed after your surgery. This could lead to further surgery.
Over time the prosthesis could erode and damage the bone stock. You will be followed up each year to check on the progress of your artificial joint and prevent this from happening.
If you have any questions or concerns about these complications, please speak to your doctor either during your clinic appointment or before your surgery.
How long will I stay in hospital?
You will usually be in hospital for two to three days after your operation, depending on how you recover.
You will be seen by your surgeon, your nurse practitioner (surgical care practitioner), and / or your physiotherapist before you go home from hospital. They will show you what exercises to do and give you further advice to guide you through your recovery.
As you have to stay overnight, make sure you bring with you items you may need, such as hygiene items (toothpaste and toothbrush), a dressing gown, slippers, and your usual medication. Also, we suggest you bring a book or magazine, in case there is a delay.
Will I be in pain after my surgery?
This surgery may be uncomfortable, you will need appropriate pain relief in the period after your surgery. If your anaesthetist has given you a nerve block, your shoulder and arm may feel numb and weak. You may not feel any pain immediately after your surgery, as the block may take 12 to 24 hours to wear off completely.
You will be given painkillers when you leave the hospital, to take at home; these should last for at least two weeks. It is very important that you take your pain relief as advised and as early as you can before the nerve block wears off; this will help you to keep on top of your discomfort. It is advisable to take your painkillers regularly for the first few days.
If possible, avoid non-steroidal anti-inflammatory medication, such as ibuprofen and naproxen, for at least 10 days before your surgery. You could use anti-inflammatory medication for five days after your surgery but you should not continue taking them after this period. Please use alternative methods of pain relieve as mentioned below. This is because anti-inflammatory medication could slow down your healing.
Take pain relief regularly to try and keep your level of discomfort at a bearable level at all times. This allows the inflammation (redness, swelling, and heat) and pain to settle. Do not wait until your shoulder is very painful to take the pain relief, as it is then more difficult to control.
What painkillers will I be sent home with?
Surgical patients might be given some of the following painkillers, depending on their age, body weight, and individual circumstances, unless told otherwise by their doctor.
Take each painkiller as advised on your prescription.
Tablet paracetamol, 1g every four to six hours (no more than 4g per day).
Codeine Phosphate, 30 to 60mg every six to eight hours.
Tablet Tramadol, 50 to 100mg every eight hours.
Oramorph, 10 to 20mg every hour, as needed.
Anti-inflammatories may be prescribed; but you should try and take as few as possible immediately after your surgery.
Please note that Codeine, Oramorph, and Tramadol should not be taken together; you should only take one of the three at any one time.
Ice packs or bags of frozen peas may also help reduce your pain. Wrap the pack / bag with a cloth and place it on your shoulder for up to 15 minutes. Do not use these peas for eating once they have defrosted.
If your pain continues and is not controlled with the medication you have been advised to take, then please contact your GP. You may also contact the East Kent Upper Limb Team if you need further help.
If you notice your wound area is becoming more painful, red, hot, and / or discharging pus (thick yellow discharge), you may be developing an infection. Contact your GP or your surgical team for advice as soon as possible.
How do I care for my wound at home?
It is important to keep your wound and dressing dry and in place until your wound is well healed, and have your stitches removed at your two week follow-up appointment with your GP practice nurse or at the hospital, with your surgeon or your nurse practitioner (surgical care practitioner). You will be told where your follow-up appointment is going to be before you leave the hospital.
If the dressing gets wet or bloodstained, you can change them yourself by carefully placing a dressing from a pharmacy. If you are unable or have difficulties doing this yourself, you can ask a relative or a friend to change it for you, or you can make an appointment with your GP practice nurse to do it for you.
If you are being seen by your GP practice nurse for a wound check 10 to 14 days after your surgery, please make sure the nurse reads the following. These instructions are for healthy looking surgical wounds only.
*Colourful stitches are non-absorbable and need to be completely removed to avoid them getting buried under the patient’s skin.
*White / clear stitches are absorbable. If any suture knots have been made outside the patient’s skin, please remove these to avoid suture abscesses. Thank you.
*The appearance and material of the sutures can be different from Trust to Trust, but these are the most common.
If a wound does not seem to be healing appropriately, please leave the stitches / knots in place and make another appointment to remove them in few days.
How long will my wound(s) take to heal?
Wounds usually take between 10 to 14 days to heal.
The area around your wounds may have some numbness, which is usually temporary. You may feel occasional sharp pains or ‘twinges’, as well as itching near your scar as it settles.
What if my wound bleeds at home?
There may be minor bleeding or clear fluid oozing from your wound in the first day or two following surgery. If your dressing gets wet or bloodstained, you may need to replace it. You can change this yourself by carefully placing a dressing from a pharmacy. If you are unable to or have difficulties doing this yourself, you can ask a relative or a friend to change for you, or you can arrange an appointment with your GP practice nurse to do it for you. You should be able to control this bleeding or oozing by pressing firmly but gently on your wound for 15 minutes.
If you are worried about the bleeding, you can contact the hospital on the number given to you (during normal working hours) or attend a walk-in centre or Emergency Department (after hours).
Can I have a bath or shower?
You should have a ‘dry wash’ or a shallow bath instead of a shower. This keeps your arm in the correct position and prevents your dressing and sling from becoming wet.
While your wound is still healing:
do not use soaps, lotions, creams, or powders on your wounds, to avoid any infection getting into your wound(s); and
keep your wound(s) dry at all times.
You can go back to normal cleaning routine once your wound is completely healed.
It is very important to remember to keep your armpit on your operated side clean and dry. Lean forward so you can reach your armpit, as separating it from the body sideways may be difficult or painful and is not allowed for the first three weeks.
Why am I wearing a sling after my surgery?
You will return from surgery wearing a sling. This is used for the first three weeks following your operation.
A physiotherapist will teach you how to take it on and off to do your exercises. It is important that you remove the sling to exercise. You can stop wearing the sling as soon as you feel comfortable.
What is the best position to sleep in?
To begin with sleeping will be difficult. Take regular painkillers and try to support your shoulder by placing pillows behind it. If you lay on your back, a pillow under your arm and elbow may make you feel more comfortable. You may find it easier to lay on your non-operated side.
You can lay on your operated side as soon as you feel comfortable and confident to do so, but it can take few weeks before this happens.
When can I drive again?
You will not be able to drive for at about eight weeks following your surgery, but this will depend on how well you recover. Your surgeon will tell you when you can drive again.
The advice from the DVLA is that you should not drive until you are physically capable of controlling a motor vehicle and can perform an emergency manoeuvre safely and confidently.
Please arrange for someone to collect you from hospital and take you home after your surgery.
When can I return to work?
This will depend on your job and how extensive your surgery was.
You can start light activities which involve using your arm in front of your body about three weeks after your surgery. If your job involves heavy lifting you will need to consider changing your job.
Your surgeon will advise you on how long you will need to be off work; you can ask for a sick note before you leave the hospital.
Please keep in mind that this is a successful procedure, but it is not a quick fix and needs lengthy rehabilitation.
When can I start my normal activities?
A physiotherapist will see you in hospital to give you advice about using your arm and doing exercises. Outpatient physiotherapy will be arranged when you are discharged from hospital.
Your arm will be painful at first. For the first three to four weeks you will be quite one handed, which will affect how you carry out your daily activities. As your pain improves so will how you can use your arm.
Most light activities are usually possible four to six weeks after surgery. However the strength in your arm will take longer to improve, and will be depend on the amount of pain and stiffness you had before your surgery.
You can start gentle swimming and exercises in water four to six weeks after your surgery. You can start practising golf six weeks after your surgery.
When should I start noticing improvement?
This varies and depends on how much movement and strength your muscles had before surgery. After you are discharged from hospital, your pain will slowly get better and you will become more confident. You will be able to use your arm in front of you for light activities. After six weeks your strength will start to improve.
Will I have a follow-up appointment?
Before you leave hospital, an appointment will be made for you to have a follow-up appointment at the Upper Limb Unit. At this appointment you will be seen by a physiotherapist, surgical care practitioner, or surgeon who will check your progress, make sure you are moving your arm, and give you further exercises as appropriate.
This appointment will usually be three weeks after your surgery. You will be monitored by a physiotherapist throughout your rehabilitation.
What if I have any questions or concerns?
If you have any questions or concerns, please contact your surgical care practitioner or physiotherapist. Their contact details are listed at the end of this leaflet.
If you notice your wound area is becoming more painful, red, hot, and / or discharging pus (thick yellow discharge) you may be developing an infection. Contact your GP or your surgical team for advice as soon as possible.
Exercises you can do after surgery, before your first physiotherapy appointment
Before starting the following exercises, please take painkillers and use ice, if needed. It is normal to experience some pain and discomfort when you perform any exercises. If you experience prolonged pain or discomfort when moving, then do the exercises less forcefully or less often. If this does not help, speak to your physiotherapist.
It is best if you do a few short sessions (two to four times a day, for five to 10 minutes each time) rather than one long session. Gradually increase the number of repetitions you do.
Physiotherapy guidelines while you are still in the hospital
An outpatient physiotherapy referral will be arranged by a member of the inpatient physiotherapy team.
You will be shown how to put on and care for your sling, and how to keep your armpit clean.
You will be shown the following exercises on the ward:
elbow, wrist, and hand exercises
shoulder girdle and posture exercises
pendular exercises
gentle isometric contractions, except internal rotation
early active assisted shoulder movements.
Hand exercises
Open and close your fist 20 times.
Wrist exercises
Move your wrist up and down 20 times.
Forearm exercises
Turn your palm up and down 20 times.
Elbow exercises
Bend and straighten your elbow 20 times.
This can be completed with help from your other arm.
Shoulder girdle and posture
Try not to slouch after your surgery.
Try pulling your shoulder blades back and down 20 times.
Pendular exercises
Lean forwards, supporting yourself with your other arm.
Swing your operated arm forwards and backwards gently, like a pendulum.
Do this 20 times.
Shoulder exercises
Lay down and lift your operated arm up, with help from your other arm.
Do this 10 times.
When you are able, do this exercise sitting up.
Isometric static contractions (1)
Gently rotate the operated side out to the side, resisting with your other hand.
Hold for 10 seconds.
Do this three times.
Isometric static contractions (2)
Gently push your operated arm out to the side, resisting with your other hand.
Hold for 10 seconds.
Do this three times.
Isometric static contractions (3)
Gently push your operated arm forwards, resisting with your other hand.
Hold for 10 seconds.
Do this three times.
Physiotherapy guidelines once you leave the hospital
You will be shown further exercises at your outpatient physiotherapy appointment or clinic appointment. If you have any questions, please contact the physiotherapists listed at the end of this booklet.
Contact details
Consultants and their secretaries
The teams listed below work at Kent and Canterbury Hospital as well.
| Hospital site | Consultant | Secretary | Contact number |
|---|---|---|---|
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Mr Sathya Murthy | Mr Sathya Murthy | 01843 235068 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Mr Georgios Arealis | Donna Cannon | 01843 235083 |
| William Harvey Hospital, Ashford | Mr Paolo Consigliere | Heather Littlejohn | 01233 616280 |
| William Harvey Hospital, Ashford | Mr Jai Relwani | Dione Allen | 01233 616737 |
| William Harvey Hospital, Ashford | Surgical Care Practitioner | Alphonsa Augustine | 07929 375381 |
Physiotherapists
| Hospital site | Physiotherapist | Contact number |
|---|---|---|
| Buckland Hospital, Dover | Abi Lipinski | 01304 222659 |
| Kent and Canterbury Hospital, Canterbury | Sarah Gillet (inpatient) | 01227 866365 |
| Kent and Canterbury Hospital, Canterbury | Darren Base | 01227 783065 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Caroline Phillpott (inpatient) | 01843 234575 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Martin Creasey | 01843 235096 |
| Royal Victoria Hospital, Folkestone | Ailsa Sutherland | 01303 854410 |
| William Harvey Hospital, Ashford | Cindy Gabett (inpatient) | 01233 633331 |
| William Harvey Hospital, Ashford | Chris Watts | 01233 616085 |
Surgical Preassessment Units
| Hospital site | Contact number |
|---|---|
| Kent and Canterbury Hospital, Canterbury | 01227 783114 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | 01843 235115 |
| William Harvey Hospital, Ashford | 01233 616743 |
Fracture Clinics
| Hospital site | Contact number |
|---|---|
| Kent and Canterbury Hospital, Canterbury | 01227 783075 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | 01843 235056 |
| William Harvey Hospital, Ashford | 01233 616849 |