Retinopathy of Prematurity (ROP)
Information for patients from the Orthoptic Department
Your baby has been diagnosed with a condition called retinopathy of prematurity. This leaflet will explain:
what retinopathy of prematurity is
what causes the condition
how your baby is screened for the condition; and
what happens after screening.
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
What is retinopathy of prematurity (ROP)?
ROP occurs when retinal blood vessels do not develop normally in babies who are born prematurely. Premature babies are those born before their expected date of delivery.
ROP can also occur in babies born at term, but who have:
a low birth weight; or
who have general infections or surgeries.
If it is not diagnosed and treated early, it can cause serious loss of vision.
What causes ROP?
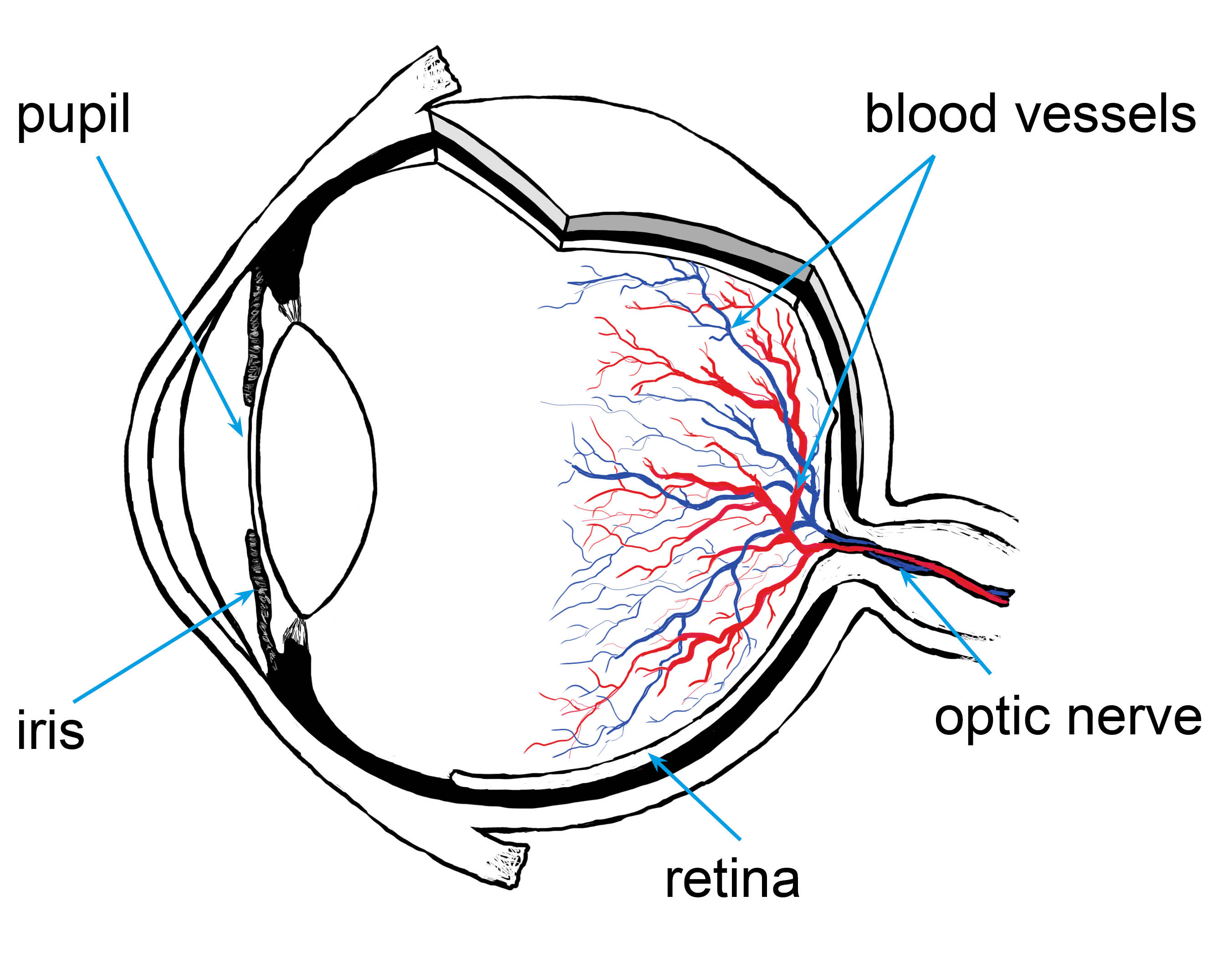
The retina is the layer at the back of the eye containing light sensitive cells. It is responsible for the first image seen by the eye, which it transfers to the brain via the optic nerve. This allows your baby to see.
If a baby is born prematurely, their retinal vessels do not develop completely and abnormal blood vessels may grow. This can cause the retina to detach.
What are the stages of ROP?
There are five stages of ROP, starting at stage 1 and progressing to stage 5.
Mild ROP at stages 1 to 2 is common and usually settles on its own without treatment. So, treatment is not usually considered until stage 3.
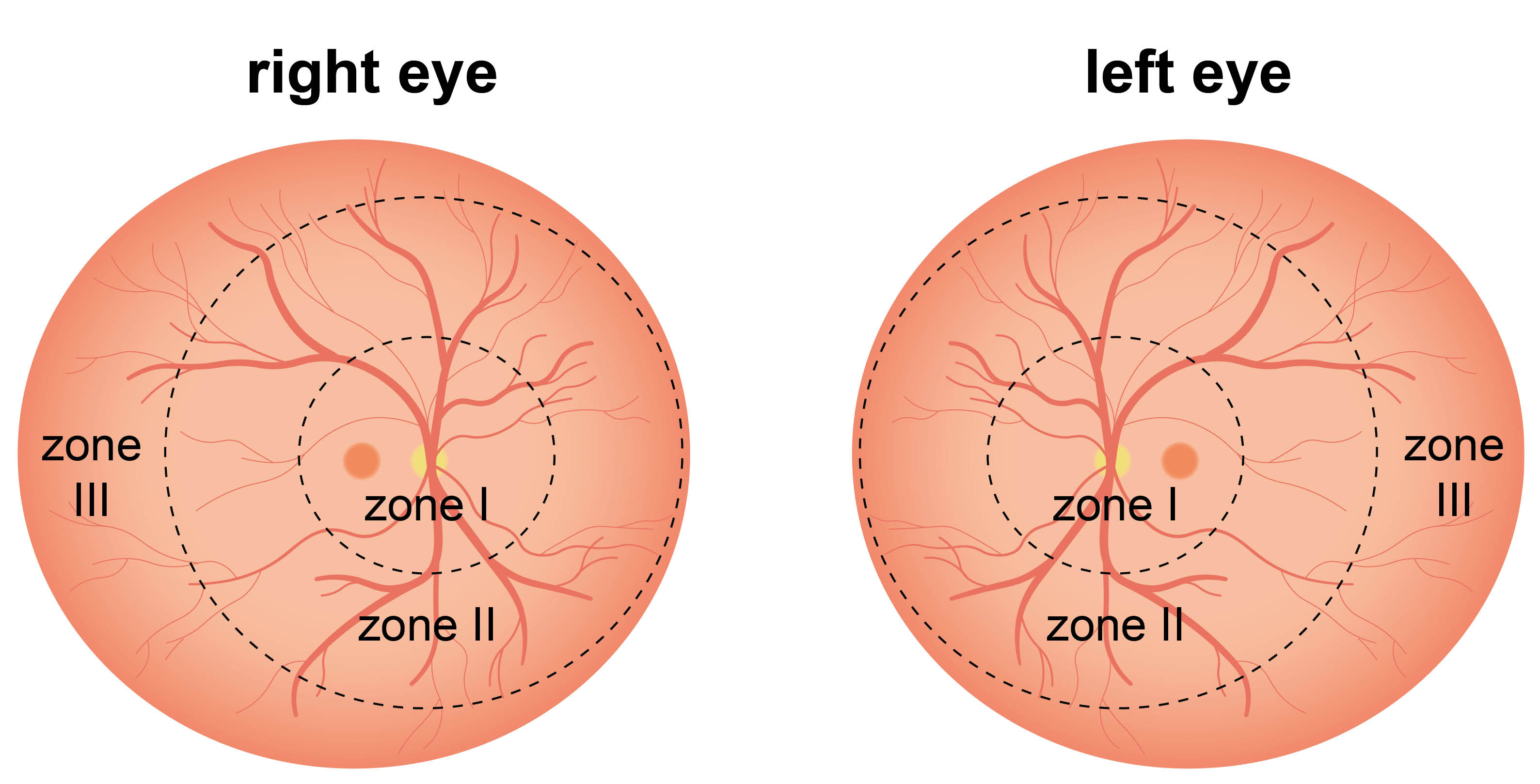
What are the zones of ROP?
The retina is divided into three zones (zone I, II, and III), from the centre of the back of the eye to the outer area. The combination of the stage and zone of ROP will decide how often we screen your baby.
What effects will ROP have on my baby’s vision?
If untreated, higher stages of ROP can cause serious sight problems and may even cause blindness.
Unfortunately treatment is not always successful. Early treatment gives a 50 to 80% chance of preventing blindness.
For mild cases, once resolved, ROP has no effect on vision.
There is a high risk that children needing treatment will develop a squint and / or need glasses.
Who will be screened for ROP?
All babies born more than 8 weeks early or who have a birth weight less than 3lbs or 1501g are screened for ROP.
The screening is usually carried out on the Special Care Baby Unit (SCBU) or Neonatal Intensive Care Unit (NICU).
If the hospital discharges your baby before their screening is complete, later screenings may be done in a paediatric outpatient clinic
Some babies only need one check, but most need at least two or three. Screenings are done at weekly or fortnightly intervals.
When and how often will my baby be screened for ROP?
The Royal College of Ophthalmology guidelines state that babies who are:
less than 27 weeks at birth have their first ROP check at 30 to 31 weeks (as if still in utero).
27 to 32 weeks at birth have their first ROP check 4 to 5 weeks after birth.
more than 32 weeks at birth but weighing less than 1501g have their first ROP check 4 to 5 weeks after birth.
All the above screenings are carried out while baby is an inpatient on the SCBU or NICU.
All further checks are fortnightly:
until no ROP is found, or
baby is at stage 3, in which case they will be checked weekly until no ROP is seen.
What happens during screening?
The nurses in SCBU / NICU will put a series of drops into both of baby’s eyes. These drops will dilate baby's pupils, so the ophthalmologist (eye doctor) can view the back of the eye and assess the retinal vessels. The drops sting slightly but babies usually tolerate this very well.
The ophthalmologist will use an indirect ophthalmoscope (eye telescope) to view the back of baby’s eye.
The ophthalmologist may need to hold open their eyelids with a speculum (clip). They may also use an indentor to help rotate the eye for a better view of the peripheral retina.
If needed, local anaesthetic drops will be used to numb the area.
The light from the ophthalmoscope is very bright and may be uncomfortable. Baby may cry but it is important to get a full view of the back of their eye. The light, speculum, and indentor do not hurt the eyes. Sometimes a slight mark may remain on the lids from the speculum for a while afterwards. The ophthalmologist will try to keep this to a minimum.
Some centres use a camera to take images of the back of the eye.
Will my baby need a follow-up appointment?
Babies treated for ROP are followed-up in an eye clinic during infancy and early childhood. The eye clinic will be either at the treating hospital or in an East Kent hospital.
If the hospital discharges baby before their screening is complete, before you leave hospital they will give you an appointment to come back to hospital to complete the screening. This will be in the paediatric eye clinic at your nearest main hospital site. It is important that you keep to this appointment. You may feel that there is no problem with baby’s vision. However, you will not be aware of the changes taking place at the back of their eye, until it may be too late to treat. Early treatment has been proven to improve visual outcome.
If you cannot make your appointment, please let us know. The contact number is at the end of this leaflet. We will arrange another appointment within the guidelines.
What will happen at the follow-up outpatient appointment?
You will need to book in at the central outpatient reception desk or self check in at the hospital. You will be directed to the outpatient eye clinic.
The orthoptist will be aware that you are waiting. They will call you into the clinic to apply the eye drops as per the procedure on SCBU / NICU. The drops take approximately 30 to 40 minutes to work. Baby may need further drops if their eyes do not dilate sufficiently with the first instillation.
An ophthalmologist will repeat the examination of your baby’s eyes. They will decide if:
they need to see baby again, for continued screening
baby can be discharged; or
baby needs treatment.
How is ROP treated?
If your baby's ROP needs treatment, they will be sent to a specialist hospital for laser treatment.
Laser treatment involves:
a general anaesthetic (baby will be asleep); or
a sedative (baby will be awake but will not feel any pain).
The laser makes small burns on the retina to stop new blood vessel growth. Occasionally laser treatment will need to be repeated.
Why has my baby been given eye drops after their laser treatment?
After treatment, baby will be given antibiotic and steroid eye drops. These will prevent infection and reduce any swelling.
Are there any side effects of the laser treatment for ROP?
As it is a surgical procedure, baby will be monitored throughout their procedure. They may need to go back on oxygen for a while.
The eye may look red, sore, and swollen after the laser treatment, but the eye drops will help with this.
Although the laser aims to help baby’s vision, it could result in restrictions to their eyesight. You will discuss this with the ophthalmologist before baby’s procedure.
What if I have any questions or concerns about the treatment?
If you have concerns, please talk to your doctor, nurse, or orthoptist.
If you need to cancel or change your child’s appointment, please call the Orthoptic Department. If there is no answer, please leave your child’s name and date of birth on the answering machine.
Orthoptic Department, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 868615
Further information
References
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email