Retinal tear
Information for patients from the Ophthalmology Department
You have been given this leaflet as your ophthalmologist (eye doctor) has diagnosed you with a retinal tear. This leaflet aims to explain what a retinal tear is and what your treatment options are.
This leaflet is not meant to replace the information discussed between you and your doctor, but can act as a starting point for such a discussion or as a useful reminder of the key points.
What is the retina?
-1729251383.jpg)
The retina is the fine sheet of nerve tissue lining the back of the eye. Imagine the eye as a camera, the retina would be the film. When the rays of light enter the eye they are focused on to the retina by the lens. The retina produces a picture which is sent along the optic nerve for the brain to interpret, in much the same way that we develop the film in a camera to produce pictures.
What is a retinal tear?
As we get older, or because of any of the conditions listed below, the vitreous gel (a transparent jelly like substance filling the back of the eye from lens to retina) begins to degenerate and shrink, pulling away from its attachment to the retina.
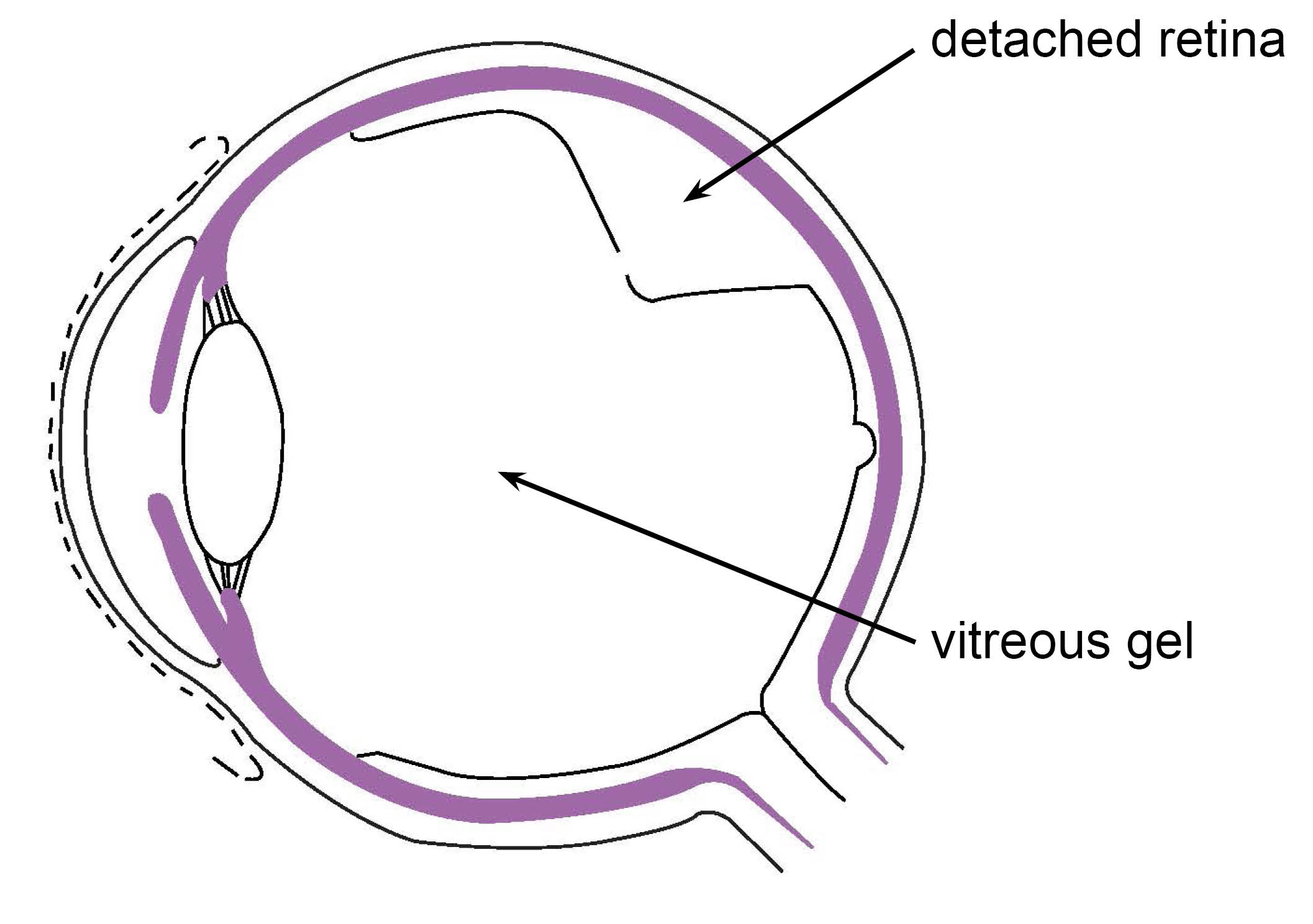
Usually it separates from the retina without causing any problems. However, sometimes the vitreous pulls hard enough, or the retina is so fragile it becomes torn in one or more places. Or the retinal tissue can weaken by itself and tear over time. Left untreated this will lead to a retinal detachment.
For more information, please ask a member of staff for the Trust’s Retinal detachment leaflet.
What can increase the risk of a retinal tear?
You are at a higher risk of retinal tear if you:
are myopic (short sighted)
suffer from glaucoma, diabetes, or Acquired Immune Deficiency Syndrome (AIDS)
have had a previous retinal detachment or tear
have a family history of retinal detachment
have weak areas in your retina (that can be seen by your ophthalmologist)
have had cataract or other eye surgery, or any other eye trauma.
What are the symptoms?
You may see bright flashes of light and/or showers of dark spots called floaters. These symptoms are never painful.
Many people have flashes or floaters and these are not always cause for alarm. However, if they are severe and seem to be getting worse or you are losing vision, then you should ask for medical advice. Quick treatment can often minimise damage to your eye.
How is a retinal tear diagnosed?
An ophthalmologist can usually see a retinal tear by looking at your retina through a magnifying lamp while your pupil is dilated. Whilst this is often part of your routine eye examination, this condition should be treated as an emergency. You should not wait for your next eye appointment to have your eye examined.
Please contact your GP who will organise an emergency appointment with the Eye Casualty Department on Rotary Ward at the William Harvey Hospital Ashford.
What is the treatment?
Your ophthalmic specialist will decide the best treatment for you, as how retinal tears are treated depends on the number, severity, and the position of the tears.
The possible treatments are listed below. Both procedures are normally performed under local anaesthesia (the area is numbed but you are awake for the procedure).
Cryotherapy is a surgical procedure involving the application of a freezing probe to seal the break.
Photocoagulation is a surgical procedure involving the application of a laser to seal the break.
Is there an alternative to these treatments?
No, at present these are the only options.
What are the complications?
Both procedures are safe and complications are rare. Damage to the eye can happen if there is sudden movement during your treatment. Therefore full co-operation between the surgeon and patient is needed during the procedure.
What if I choose not to have treatment?
If left untreated your vision is likely to deteriorate (get worse). You may also notice a loss of vision similar to a curtain falling across part of your vision, as your retina detaches from the back of your eye.
What is the success rate?
If the break is treated quickly, more than 95 in every 100 patients (95%) will have a successful procedure.
What happens after my treatment?
You will be encouraged to get up and carry on as usual after your procedure.
You may be prescribed eye drops, which you may need to use for several weeks.
You will be given a booklet called Discharge advice for patients following eye surgery when you leave hospital. This leaflet covers caring for your eye after treatment, when you can drive again, and whether you will need a follow-up appointment. Please follow the advice in this leaflet carefully.
Further information
If after reading this leaflet you have any further questions or concerns, please contact the healthcare professional responsible for your care.