Renal artery denervation (RDN)
Information for patients from the Renal Department
You are being invited to have a procedure called renal artery denervation (RDN). Some people have blood pressure that is difficult to control with medication. This may be because those medications are insufficiently effective or have caused side effects. Recent research shows that RDN may be an effective treatment for such people. However, our understanding of long-term effects (beyond about three years) are not known. It is important you spend a few minutes reading this information leaflet carefully and discuss it with others if you wish.
Why have I been invited to have renal artery denervation?
You have blood pressure that is elevated above recommend levels either:
despite taking a combination of blood pressure lowering tablets that would usually be effective or
because you are not able to tolerate usual blood pressure tablets.
Having uncontrolled blood pressure will increase your risk of suffering a stroke, heart attack or damage to your kidneys and major blood vessels. The team of doctors involved in your care think that RDN may help lower your blood pressure.
What is the background to this procedure?
High blood pressure is one of the most common and preventable causes of premature heart disease, kidney disease and stroke in the United Kingdom (UK). It affects about one in 4 adults and more than half of those over 60 years old. The cause of the majority of cases of high blood pressure is not fully understood and is generally called ‘essential hypertension’.
Several different factors contribute towards essential hypertension. These include:
increased retention of salt and water by the kidneys
reduced blood flow through the kidneys due to:
nerves involved in ‘stress’ responses (the sympathetic nervous system)
activity of a hormone system (the renin-angiotensin-aldosterone system).
What is the standard treatment for high blood pressure?
The standard treatment for high blood pressure in the UK is a combination of:
blood pressure lowering medicines, and
lifestyle changes including: reducing dietary salt intake; keeping within recommended limits for alcohol consumption; increasing exercise and losing weight where appropriate.
Despite taking medication, about half will still have uncontrolled blood pressure. Common reasons for this include:
Too few or insufficient doses of blood pressure medications. Sometimes people need three or more different types of medication to control blood pressure. Also, although some people don’t tolerate higher dose of some tablets due to side effects, it is quite common for blood pressure medications to be prescribed at low doses without a good reason.
Not taking medications regularly or in amounts suggested by your doctor. Non-adherence with medication is a common reason for uncontrolled blood pressure.
Not making changes to lifestyle. Being overweight, not taking enough exercise and excessive salt and alcohol intake are common reasons for uncontrolled blood pressure.
“White coat effect”. This is where blood pressure rises in response to a stressful situation, for example visiting a GP or hospital. It affects up to a third of people with apparently uncontrolled blood pressure. We identify people with white coat effect by using home or automated mobile blood pressure monitoring (also known as ambulatory blood pressure monitoring, ABPM).
“Secondary” hypertension. Underlying causes are found in about 1 in 20 people with uncontrolled blood pressure. These are usually over-production of certain hormones or kidney artery narrowing.
Before inviting you for RDN your doctor will have ensured that you are taking an optimal combination of blood pressure lowering medication. We will also look for and exclude: non-adherence to medication, ‘white coat effect’ and underlying (‘secondary’) causes.
Will I still need to take my blood pressure medication after the denervation procedure?
It is unlikely that RDN will enable you to stop taking your current blood pressure lowering medication (if applicable). Your doctor will know about the medication you are prescribed, but you know best how often you take your tablets. We may use urine samples collected in clinic to assess whether you are taking medication as recommended.
If you have any problems with taking your tablets regularly please discuss these concerns with your doctor. This is important because treating blood pressure with medications has proved to be very safe and effective over the last 50 years.
Sharing information about your treatment anonymously within the Global GPS Registry
RDN has been shown to be effective at lowering blood pressure in several clinical trials. NICE (the organisation that advises on treatments in England and Wales) requires that doctors who undertake RDN gather information on safety and effectiveness of the procedure. ReCor Medical is the company that manufactures the denervation catheters that we will be using. We are participating in the Global GPS Registry study that is funded and run by ReCor. You will receive a separate Participant Information Sheet about the Global GPS Registry study.
What does renal denervation involve?
Most people have two kidneys, each of which is supplied with blood through an artery (the kidney – or renal – artery). On the outside of these arteries are small nerves (renal sympathetic nerves) which carry signals between kidneys and brain. These are the nerves we are trying to interrupt. Kidneys seem to work perfectly well doing their normal job - i.e. removing waste products and excess water from the body - without these nerves. We have known for many years that cutting these nerves can reduce blood pressure but it has not been practical to do this until very recently.
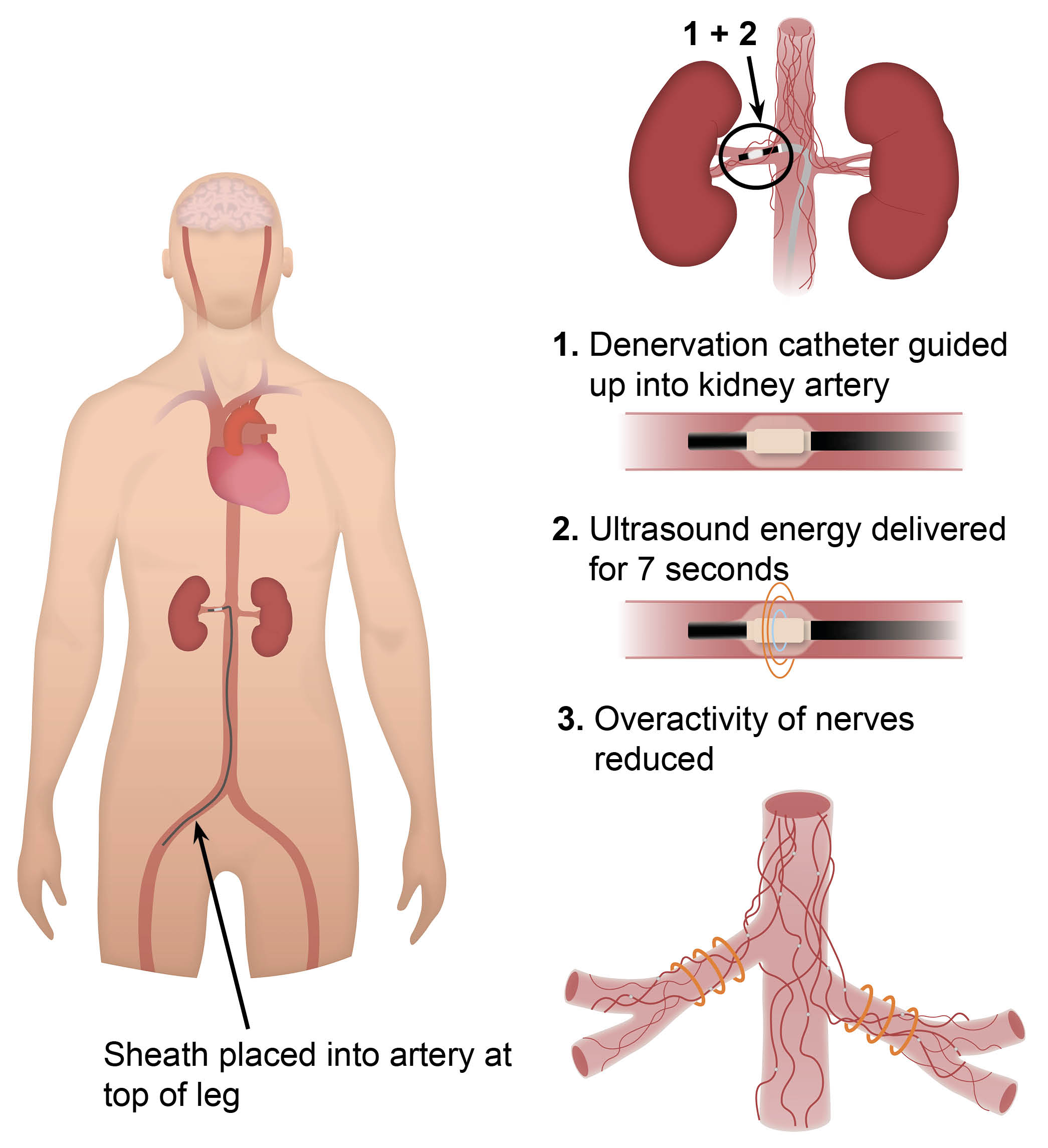
The new method of renal denervation uses a special wire fed up inside the artery from the groin. Ultrasound energy is applied to the wall of the artery from the inside and energy disrupts the nerves that run along the outside of the artery.
What are the steps I have to go through for the renal denervation procedure?
Tests and imaging that are needed
Your doctor will already have investigated you for causes of high blood pressure with a variety of scans, urine and blood tests. You will have a CT or MRI scan of your kidney arteries and an ABPM machine to make sure you are suitable for this procedure. Before your admission your doctors will have discussed your investigations and agreed that RDN is an appropriate treatment for you.
Pre-admission visit
You will be ‘seen’ by one of the Consultant Interventional Radiologists in a clinic. An Interventional Radiologist is a doctor who specialises in manipulating fine guidewires and catheters within blood vessels. Usually this appointment will be by telephone but may take place in the Vascular Assessment Unit (1st Floor, Main Building, Kent & Canterbury Hospital).
You will then have a face-to-face visit with one of the interventional radiology nurses. This will happen a few days before your admission. Here we will ask you standard questions about your health as well as have pre-operative swabs. The Consultant Interventional Radiologist will make final checks to ensure you are ready for the procedure. They will explain what the procedure involves, and ask you to sign a consent form.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
Admission to hospital
You may be admitted to a bed on Marlowe (Ground Floor, Main Building, next to main X-ray), Kent Ward (1st Floor, Main Building, next to Vascular Assessment Unit) or the Surgical admissions unit at Kent & Canterbury Hospital on the morning of your procedure. You should bring clothes, your usual medications and other personal items for an overnight stay. You should take your usual medications on the morning of the procedure, unless advised otherwise at the pre-admission visit.
Having the procedure
RDN is performed by an Interventional Radiologist in a purpose built room called KIRC (Kent Interventional Radiology Centre). You will be given a painkiller and mild sedative by an anaesthetist to minimise any discomfort. However, the procedure does not need to be done under general anaesthetic.
You will lie on an x-ray table and an x-ray camera, mounted on an extendable robotic arm, is positioned over your abdomen (tummy). The Interventional Radiologist inserts a small plastic sheath into an artery (blood vessel) at the top of your leg. This area will have first been numbed by a local anaesthetic injection, and you should feel no discomfort.
The Interventional Radiologist uses the x-ray camera to help guide a fine catheter up into your kidney arteries. Once in position, dye is injected through the catheter to confirm the position inside the artery. A special wire is then fed through the catheter and ultrasound energy is delivered to the wall of the artery from the inside. The right amount of energy is used to make sure that the artery wall does not get damaged. Treating both of your arteries takes a few minutes.
Rarely, we will find narrowed kidney arteries that were not seen on imaging done before the procedure. In this situation, it may not be possible to proceed to RDN.
At the end of the procedure, the catheter and sheath are removed. The puncture in the leg artery is sealed either by applying gentle pressure for a few minutes or using an arterial closure seal. An arterial closure seal, if used, will dissolve slowly over the following weeks and will not need to be removed.
Pain and pain control
During the energy bursts to the nerves many patients feel some pain or discomfort in the back or flank area. You will have been given powerful pain killers in advance and more will be given if necessary so that the discomfort is minimised. Your team will ask you how you feel during the treatment to make sure you get enough painkiller. In a way, the pain is a sign that the wire is in the right place, because it comes from the same nerves that we are trying to treat. It usually passes quite quickly once the treatment has been completed.
After the procedure
Once the procedure has been complete, you will move to the recovery area next to KIRC. When you have recovered from the sedation, you will be taken back to Kent or Marlowe Ward. Your blood pressure and other vital signs will be monitored for the rest of the day and overnight. You will need to remain lying flat for two hours following the procedure.
We will usually discharge you by lunchtime the day after the procedure if you haven’t had any complications and your blood pressure is stable.
After discharge from hospital
Unless we advise you otherwise, you should continue your usual blood pressure medications. We will arrange a follow-up appointment with your blood pressure doctor. This will usually be within 2 to 6 weeks of having the procedure.
If you experience the following symptoms:
Dizziness
Pain in back, tummy or groin
Excessive bleeding or bruising from the puncture site at the top of your leg
Or are otherwise concerned, you should seek advice from:
Dr Doulton (via his secretary on 01227 864229, 8 am to 4 pm Monday to Friday)
Dr Das (via their secretary on 01227 783181 or 01227 864023, 9 am to 4 pm Monday to Friday)
The on-call Renal Registrar via the hospital switchboard on 01277 766877 or Marlowe Ward on 01227 783100
In an emergency you should seek urgent attention at your nearest emergency department, or by calling an ambulance on 999.
Is renal artery denervation safe?
With any ‘endovascular’ procedure (a procedure where we advance catheters through a person’s arteries) there is a small risk of damaging the arteries on the inside. Patients who have RDN will have been investigated for disease of the arteries beforehand to identify those at increased risk. If you have a significant build-up of ‘plaque’ or narrowing in your kidney arteries you may not be able to have the procedure.
RDN is a fairly new technique. The information available so far, from patients followed for 2 to 3 years after the procedure, indicates it is safe. No-one has died and there has been no documented lasting damage to a kidney or effects on kidney function.
Are there any side effects?
The commonest side effects include bruising in the groin.
Other uncommon but more serious side effects that have occurred are:
Damage to the kidney artery. There has been one reported case of this happening. The International Radiologist would treat this by placing a stent in the damaged artery (like an internal scaffold or spring to keep it open).
Persistent abdominal or pain lasting beyond the time of the procedure. This usually settles within a few weeks and you may need to take painkillers.
Low heart rate which usually settles.
Large drop in blood pressure. This may need you to stay in hospital for an extra one or two days to adjust your blood pressure medication.
Damage to the artery in the groin. This occurs in about 1 in 50 procedures is usually treated with a small injection. In very rare cases you may need a blood transfusion or a small operation to repair the artery.
Other possible side effects that have not been seen with renal denervation, but which can occur when we use X-ray dye (contrast) include:
Allergic reaction to the dye (if it occurs, this is usually mild and causes a rash that settles by itself)
Reduced kidney function (may occur in patients who have reduced kidney function at the outset and is usually temporary if it occurs)
Potential side effects from renal denervation that have NOT yet occurred, but might happen in future, include narrowing of the kidney arteries and reduced kidney function.
What is the evidence that renal denervation is effective and safe?
This procedure uses the ReCor Paradise™ ultrasound denervation system. It has been tested in a series of clinical trials in people on and off blood pressure lowering medication. The combined results of these trials have recently published in JAMA Cardiology (see ‘Further Reading’ below).
506 people participated in three trials: RADIANCE II, RADIANCE-HTN SOLO and RADIANCE-HTN TRIO. These participants were allocated at random to receive RDN or to undergo a sham (placebo) procedure. The main outcome from each trial was change in ABPM - considered to be the ‘gold standard’ of blood pressure measurement - from before the procedure (baseline) to 2 months afterwards.
The key findings from the trials are as follows:
Those treated by RDN had an average systolic blood pressure reduction of 8.5 mmHg. This compares with 2.9 mmHg in people having the sham procedure (average difference 5.9 mmHg).
Blood pressure reductions in an outpatient clinic setting were 10.4 mmHg in the RDN group and 3.4 mmHg in the sham group.
Blood pressure reductions tended to be larger in those whose blood pressure at baseline was higher than the average. The average baseline blood pressure across all participants being 151/94 mmHg.
Major procedure related complications occurred in <1% of people having RDN. No new kidney artery narrowing or changes in kidney function were detected 6 months after the procedure.
Pain lasting more than 2 days related to the procedure (usually mild and in any location) was reported in 11 to 16% of participants. There was no difference between those that had RDN and those having the sham procedure. This implies that RDN itself is unlikely to cause lasting discomfort.
There is no absolute guarantee that RDN will lower your blood pressure, even if correctly performed. As with all new treatments, our knowledge of who might and might not benefit will improve as time goes on. We only know about effects of RDN on blood pressure for up to 3 years after the procedure. Whether the effects diminish with time beyond approximately 3 years is presently unknown.
Am I eligible for renal denervation?
It is important to understand that RDN is currently recommended (in England, by NICE) for people who either have:
uncontrolled blood pressure despite an optimal combination of blood pressure lowering medications or
intolerance of a wide range of blood pressure lowering medications
Also, some people may not be able have the procedure, for example if you have:
Moderate or severely impaired kidney function (eGFR under 40 ml/min), or
Kidney arteries that are too small, too large or narrowed due to ‘plaque’ or
Only one kidney
We will offer you RDN if you fulfil the criteria outlined above, are already taking an optimal medication regimen, and you have made reasonable lifestyle modifications.
Thank you for taking the time to read this information leaflet.
You can get more information when you next attend your blood pressure clinic appointment, or via Dr’s Doulton or Das (contact details as above).