Reducing your risk of pressure ulcers
Information for patients from the Tissue Viability Committee
Anyone can be at risk of pressure damage if they are not able to move around as normal; this risk increases when a person is ill. This leaflet explains how we can work together to reduce your risk of developing a pressure ulcer.
What is a pressure ulcer?
A pressure ulcer is an area of the skin which has been damaged by excessive or prolonged pressure. Pressure ulcers can also develop under devices such as oxygen tubing / masks, catheter tubing, and stockings used to prevent blood clots. In full health, we automatically move our body weight so that pressure is not left too long on any one part of the body. Not being able to do this, due to difficulty in moving or loss of feeling, puts us at risk of developing a pressure ulcer.
A pressure ulcer may also be caused by the skin sliding over the underlying body tissues, known as shear. Good supportive postures which prevent slipping and sliding can help to reduce shear forces. Friction (two surfaces rubbing together) can also cause tissue damage.
Am I at risk of pressure damage?
There are many risk factors associated with developing pressure damage. You may be at risk if you answer yes to any of the following questions.
Are you over 65 years of age? As we get older our skin thins and we produce less collagen, making us more likely to get pressure damage.
Do you suffer from heart, lung, or vascular disease?
Do you have diabetes?
Do you need help to move about?
Have you been immobile in a bed or a chair?
Are you eating and drinking less than usual?
Are you in too much pain to move?
Do you have excess fluid in your lower legs?
Are you attached to a device such as a catheter or oxygen mask? Or are you wearing stockings to prevent blood clots?
We will assess your risk on admission to hospital. Ask your nurse if you are at risk.
How can my risk be reduced?
A range of measures may be used to address your individual risk factors. This mainly involves making sure you are drinking and eating enough, together with reducing pressure, shear, and friction. In a small number of cases, pressure ulcers may still develop despite full prevention taking place.
The SKINS bundle is a nationally recognised tool. It is used to show key areas of pressure ulcer prevention.
S = Support Surface such as mattress or chair.
Special pressure redistributing mattresses may be mechanical or high specification foam. All hospital mattresses are high specification foam, which helps to redistribute pressure.
If you are thought to be at very high risk of pressure damage you will be offered an active (air) mattress. These mattresses have air pumped through them to redistribute the pressure underneath you.
Electric profiling beds
Most hospital bed frames are mechanically operated and help to prevent shear forces and redistribute weight. There is a patient’s handset which allows you to help change your bed’s position as needed.
Heel protector boots
Heels are particular risk of pressure, so you may be offered a pair of heel boots if you are unable to move your own legs. These boots are designed to take all the pressure off your heel and should only be worn in bed. If you are unable to tolerate wearing them, a pillow may be used under your legs to take the pressure off your heels.
Seating
It is important that your chair is the correct height and width to support a good sitting position. You may be offered a pressure cushion, although many hospital chairs have this ‘built in’. It is recommended that you shift your weight in the chair at least every 20 minutes. Ask your nurse or therapist about chair exercises.
K = Keep moving
An individual positioning and repositioning plan should make sure you are nursed in the most comfortable and effective positions. Frequency of positioning is recommended on an individual basis depending on the condition of your skin. Our general advice is:
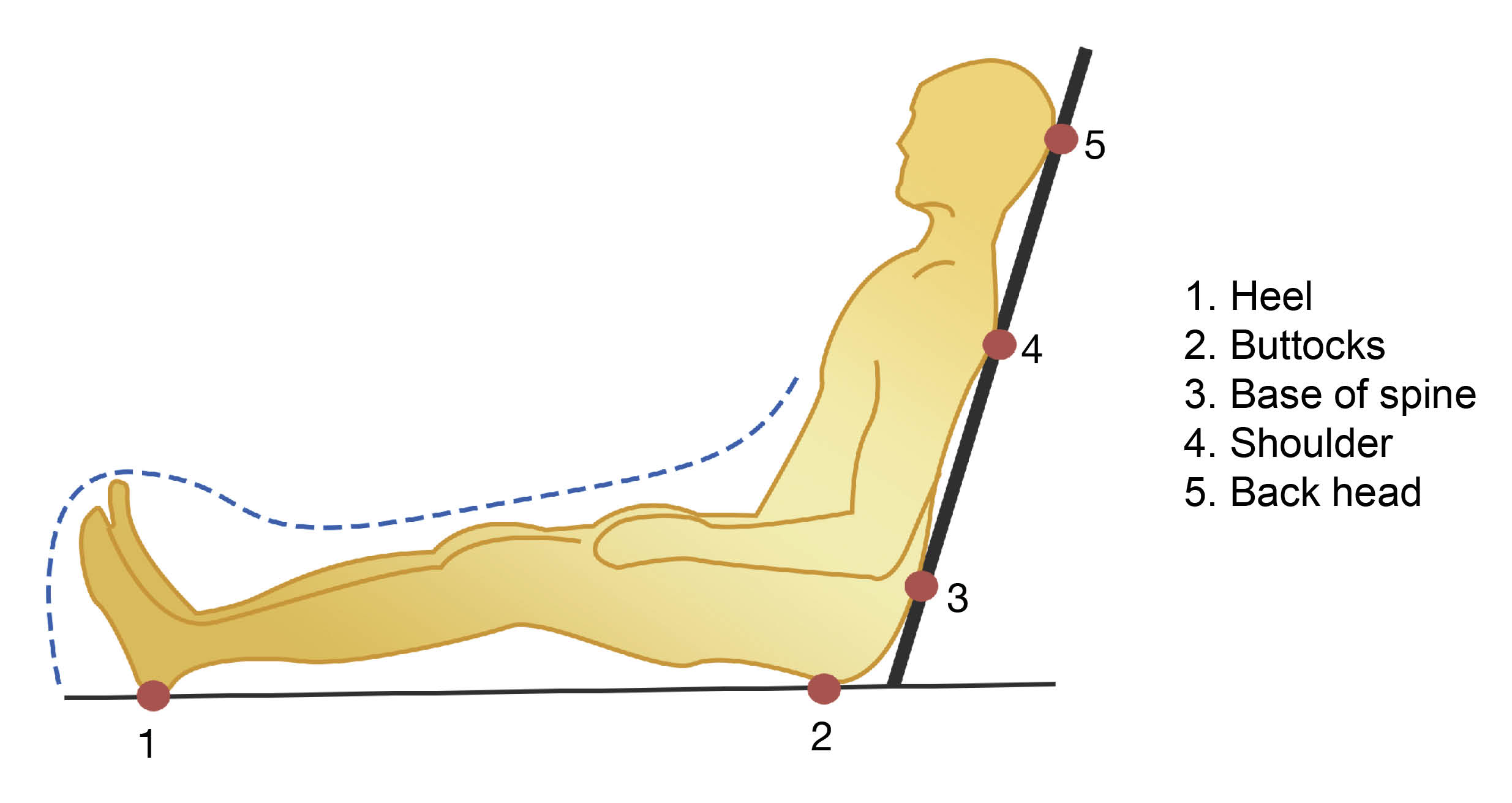
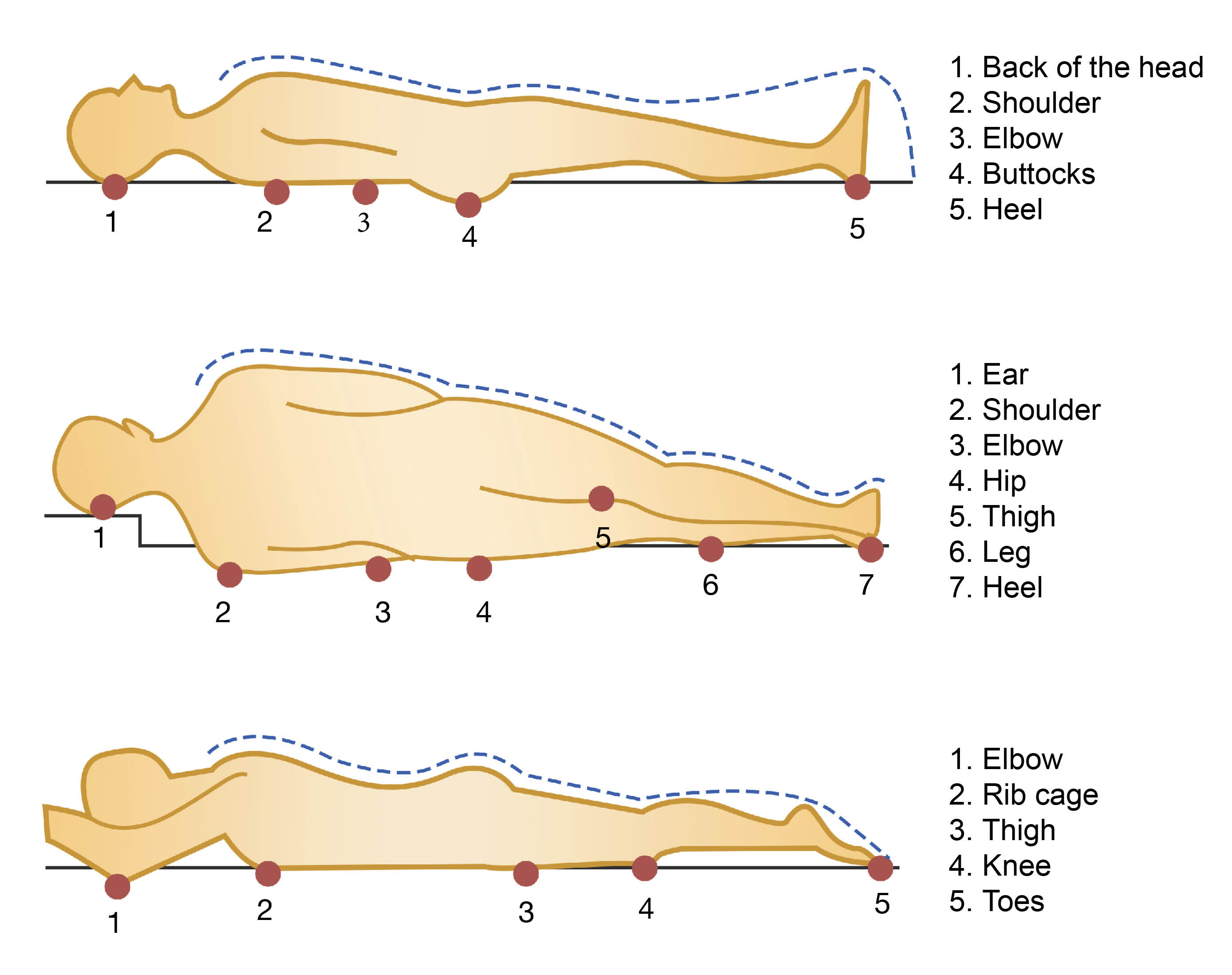
Flatter positions are better, as they spread the pressure more evenly over your body.
Avoid lying on ‘bony areas’ of your body.
It is better to use a slight tilt to the side than lay fully on your hip bone.
Elevating (raising) your knees when sitting up in bed reduces pressure on your bottom and heels, the two most vulnerable areas on your body.
Sit out in a chair for short periods at a time, for example under two hours.
Check your skin regularly for early signs of pressure damage (often a red mark). If you do notice pressure damage, further precautions should be started to avoid pressure on the affected area. These measures may include more frequent repositioning and / or a higher risk mattress.
I = Incontinence
Keeping skin clean and dry can reduce your risk of developing pressure ulcers. Avoiding soap (which dries the skin) and using a pH balanced cleanser is recommended for regular cleaning of vulnerable skin. If skin is still becoming sore, a skin barrier product may also be used (these can be supplied by ward staff).
The use of incontinence sheets is not recommended as they do not absorb the moisture away from the skin, and can play a part in moisture-related skin damage. If needed, we would advise that you use a shaped incontinence pad instead, as these absorb any liquid.
N = Nutrition
While you are in hospital you may not have as much of an appetite as usual, but think of food as medicine and try to eat something at each mealtime. The hospital menu uses the code HC to show which lunchtime dishes are high calorie; try to pick those to get the most goodness out of what you eat. Top tips include:
Try to have two to three portions of protein rich food daily. This includes meat, fish, poultry, cheese, pulses, and dairy products.
Ask your ward housekeeper for smaller portions if you find the meals are too large. You may find you prefer a lighter meal, such as an omelette or filled jacket potato.
Tell ward staff and the housekeeper if you have any specific dietary needs.
Please ask for help if you have any problems when eating and / or drinking.
A small snack inbetween meals can give additional nutrition without being too filling. Good choices include yoghurt, cheese, and biscuits, or a glass of milk. Snacks are offered mid-morning, mid-afternoon, and in the evening.
Although you may not feel thirsty it is important to drink regularly throughout the day. There will always be water by your bed, and the housekeeper will offer you a drink from the trolley seven times during the day. There are a wide range of drinks available, not just tea and coffee. Try to have a glass of fruit juice each day, as vitamin C helps wounds to heal.
If you have concerns about your diet, please ask to speak to a dietician. They can give advice for while you are in hospital, and if needed arrange for you to have an outpatient appointment with a dietitian when you leave hospital.
S = Skin assessment
What are the signs of pressure damage?
Early signs of pressure damage may be redness or discoloured areas at your pressure points. This may be difficult to see on darker skin tones. Touch may be used to feel for hot, cold, boggy, or spongy areas. Purple bruising can mean you have pressure damage in your deeper tissues.
The nursing staff will ask to check your skin at least each day, to check if your skin is at risk or if you are showing early signs of pressure damage.
What if I develop a pressure ulcer?
Pressure ulcers are given categories to show the depth of the tissues affected. The categories are one to four, with category one affecting only the very top layers of skin, and category four affecting the skin and deeper tissues. It is difficult to assess the depth of some pressure ulcers, as they may be covered with slough or dead tissue. Once this is removed, the pressure ulcer’s depth may be assessed.
The main treatment for all pressure ulcers is to remove all pressure from the ulcer. This may be by repositioning or elevating the affected part of your body. Your nurse will check your ulcer and advise you of the best treatment for you.
When you are sent home from hospital, if you have developed a pressure ulcer the ward will either advise you to book a follow-up appointment with your GP practice nurse, or if you are housebound they will send a referral for the community nurses to come to your home and check your wound for you.
What can I do to help?
You or your carer may wish to take part in your own care. You can help by:
Telling your nurse when you feel you need to be repositioned.
Checking your skin regularly; a mirror may be useful for checking your heels or difficult to reach areas. If you see any changes tell your nurse.
Eating a nutritious diet.
Drinking plenty of fluids.
Asking your physiotherapist about bed and chair exercises.
Telling your nurse if you feel any discomfort at a pressure point.
Working together with your nursing staff to develop the best positioning and repositioning plan for you.
Although we will advise you on the best ways to prevent pressure ulcers from forming, your choice and comfort is important. We will fully support your decisions and change your prevention plan if needed. However, this may result in less than fully preventative care during your hospital stay.
If you need further advice, please contact the tissue viability nurses on 01227 864004.
When you go home
Your hospital nursing team will contact your community nursing team to make sure that any pressure-relieving equipment or treatment you may need is provided at home following your discharge from hospital.