Reducing the risk of venous thromboembolism (VTE) in pregnancy and the postnatal period
Information for women, birthing people, and their families
This leaflet is about reducing the risk of blood clots in pregnancy and the postnatal period. This condition is known as venous thromboembolism or VTE.
What is a venous thromboembolism?
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are both known as a venous thromboembolism (VTE).
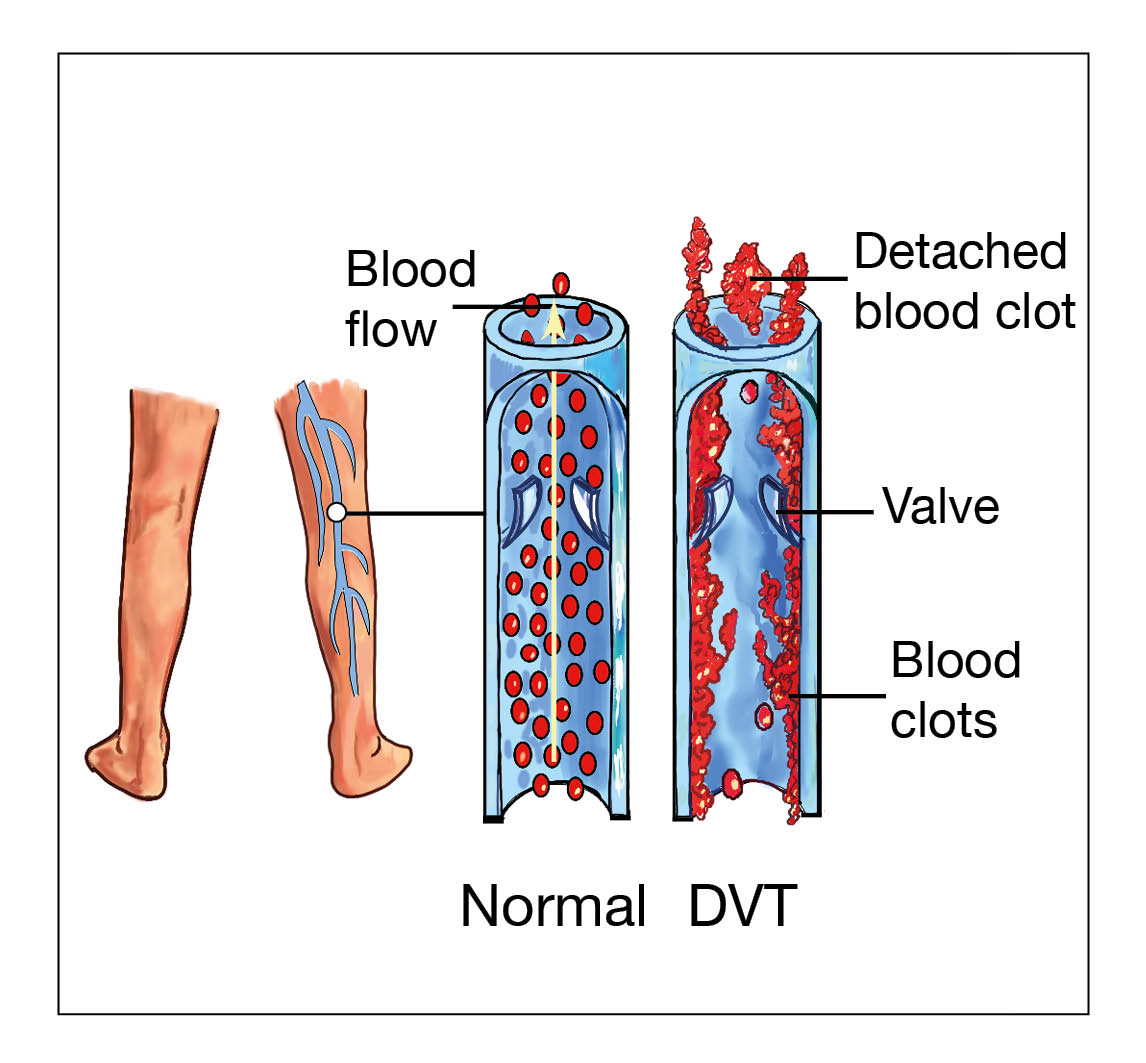
A DVT is a blood clot in a deep vein. Deep veins are large blood vessels which return blood to the heart. These veins lay deep within the body and cannot be seen. A DVT usually involves the deep veins of the legs, thigh, or pelvis, but can occur elsewhere in the body. Calf veins (found in the back part of your lower leg, between your knee and ankle) are the most common site for a DVT.
Symptoms can vary according to the size and location of the clot. They may include:
Swelling of your limb / leg (this can be sudden).
Pain or tenderness in your limb / leg, often in the calf. This can increase when standing or walking.
Change in skin colour. For example red or purple of light skin tones, and darker brown on darker skin tones.
Unexplained feeling of warmth in your limb / leg.
Swollen veins that are hard or sore to touch.
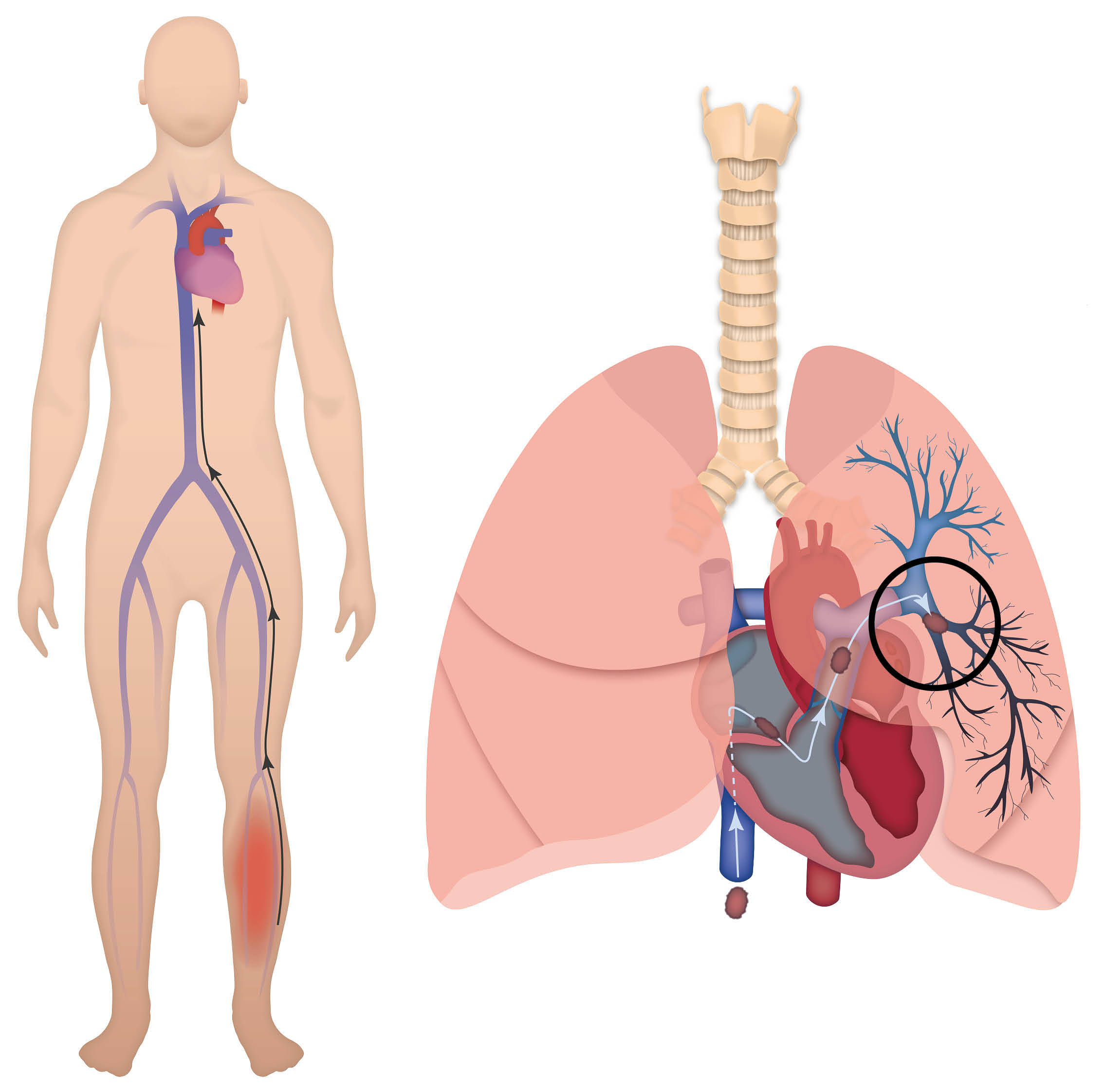
A pulmonary embolism (PE) is a blood clot, which is lodged in one or more of the arteries in the lung. A PE usually originates from a DVT. A PE can be life threatening if left untreated.
Symptoms can include some or all of the following:
Shortness of breath, either at rest or on exertion (this may be sudden and unexplained). This is due to the blood clot restricting the blood flow through the lungs. In some cases, oxygen may be needed to help with this.
An increased heart rate. This is due to the heart having to work harder to make sure enough oxygen is transported around the body.
Tightness in your chest or chest pain. This may be constant or only when breathing deeply. This is due to inflammation in the lungs or lining of the lungs.
Coughing. Occasionally, coughing up blood, or blood stained sputum.
Feeling very unwell or collapsing.
May also be accompanied by symptoms of a DVT.
If you have any symptoms or concerns, call our telephone Maternity Triage service. Their phone number is on your lilac notes and at the bottom of this leaflet. In an emergency or if symptoms are severe, call 999.
What are the risk factors?
Pregnancy increases the risk of VTE by four to six times. The highest risk is soon after childbirth. Your risk of VTE increases further if you:
Have had a previous VTE.
Have a thrombotic condition called thrombophilia, which makes a blood clot more likely.
Are over 35 years of age.
Are overweight (have a body mass index (BMI) over 30).
Smoke.
Have a close blood relative that has had a VTE. This includes your brother / sister / mother / father.
Have had three or more babies.
Are pregnant as a result of IVF (in-vitro fertilisation).
Are carrying more than one baby (twins or more).
Have severe pre-eclampsia.
Have a medical condition which might increase your risk of a DVT / PE.
Have severe varicose veins that are painful or above the knee, with redness / swelling.
Have reduced mobility (are not able to move around a lot).
Have recently had a baby by caesarean birth or had a long labour (more than 24 hours).
Are immobile for long periods of time, for example after an operation.
Are travelling for four hours or longer.
Are admitted to hospital.
Are dehydrated.
Are unwell from fertility treatment (ovarian hyperstimulation syndrome).
When will my risk of developing a VTE be checked?
Your midwife will carry out a risk assessment at your booking and again around 28 weeks of pregnancy. They will look at your risk factors (see previous section), and give you an overall risk score for a VTE.
If your VTE risk score is high, you will be referred to the consultant clinic. At this clinic you will receive advice, and discuss your treatment options. At your clinic appointment, we will discuss your options in detail. Please ask any questions at this appointment. You can talk through your concerns before any decisions are made.
We will reassess your VTE risk score if your situation changes during your pregnancy. It will also be reviewed if you are admitted to hospital, and after the birth of your baby.
What if I am already on other blood thinners?
Your GP should arrange a hospital appointment for you if:
you had a DVT or PE before, or
you have a thrombophilia.
You can ask to have this appointment even if you are thinking about becoming pregnant. You should see a doctor who specialises in thrombosis in pregnancy.
If you are taking warfarin, you may be advised to change to enoxaparin injections. This is because warfarin can be harmful to your unborn baby. Most women are advised to change before becoming pregnant. If not you will be changed to an alternative as early as possible in your pregnancy. Do not stop your medication without medical advice.
Can my risk change?
Yes. Your risk can increase if you:
develop other factors, such as becoming unwell
develop severe varicose veins
are travelling for over four hours, and / or
are expected to have a complicated birth. In this case, you may be advised to start taking treatment.
Your risk may also go down, for example if you stop smoking. Treatment may then no longer be needed. If there are any changes, please let your midwife know.
How is VTE prevented?
To reduce your risk of getting a DVT or PE:
Stay as active as you can.
Keep hydrated, by drinking normal amounts of non-alcoholic fluids.
Stop smoking.
Lose weight before pregnancy if you are overweight.
Depending on your risk score, clinicians will discuss appropriate methods to prevent clots.
Enoxaparin (heparin) injections
You may be advised to start treatment with injections of enoxaparin. Enoxaparin is an anticoagulant used to thin your blood. It is a low-molecular-weight heparin. This is the most common type of heparin used in pregnancy.
Enoxaparin is also used to treat a VTE. However, the dose used to prevent a VTE is usually less. For most patients, the benefit of enoxaparin is that it reduces the risk of a DVT or a PE developing.
Foot / leg pumps
You may also be advised to wear foot or leg pumps. For more information, see the Foot / leg pumps section below. These increase the blood flow within your legs. They are very helpful, especially if you can't move around after surgery.
What does enoxaparin treatment involve?
Enoxaparin is given as an injection under the skin (subcutaneous) at the same time every day. Dosage depends on your weight and your individual risks.
You (or a family member) will be shown how and where on your body to give the injections. See injecting yourself with enoxaparin below. We understand that you may be worried about this. If you are worried or frightened about this, please talk to your midwife or healthcare professional.
Clinicians will provide you with the needles and syringes (already made up) and a sharps bin. You will be given advice on how to store and dispose of these.
Some blood-thinning treatments contain animal products. Enoxaparin has content that has been derived from pigs. If you are concerned about this, please speak to your midwife or your healthcare professional.
Will being on enoxaparin affect how I give birth?
No. Taking enoxaparin during pregnancy should not affect how you deliver your baby.
Are there any risks to my baby and me from enoxaparin?
Enoxaparin is a low-molecular-weight heparin. It does not cross the placenta, so it cannot harm your baby.
There may be some bruising where you inject, but this will usually fade in a few days.
The medicine may sting a little when you inject it, but this only lasts a few seconds.
One or two patients in every 100 (1 to 2%) will have an allergic reaction. If you notice a rash after injecting, you should tell your doctor so that they can change the type of medicine.
You should also contact us if you have any bleeding. Phone our telephone Maternity Triage service if you have any concerns. Their number is in your lilac notes, and at the bottom of this leaflet.
How long will I need to take enoxaparin for?
How long you take enoxaparin for will vary depending on your individual risk factors. For example:
Treatment may be for the whole of your pregnancy, and for up to six weeks after birth.
It may start at 28 weeks, and continue for up to six weeks after birth.
It may be for only a few days to cover long-distance travel.
It may only be needed after birth, which can be for 10 days or for six weeks after delivery.
What should I do when labour starts while I am taking enoxaparin?
If you think you are going into labour, please do not take any more injections. Phone Maternity Triage and tell them that you are on enoxaparin treatment for VTE. They will tell you what to do. Their telephone number is on the front of your lilac notes, and at the bottom of this leaflet.
Can I have an epidural whilst taking enoxaparin?
There is a 12 hour ‘window’ between when you take your last dose of enoxaparin, and when an epidural can be given. You will be offered alternative pain relief if you are within this time frame. Your midwife will discuss these options with you. If the plan is to induce labour, you should stop your injections 12 hours before the planned date.
What happens if I have a caesarean birth?
For a planned caesarean birth. Your last enoxaparin injection should be 12 hours before the delivery.
For an emergency caesarean birth. If your last enoxaparin injection was within 12 hours, you will not be able to have an epidural or spinal injection. Instead, you will need a general anaesthetic for your operation. The anaesthetist will discuss this with you.
What happens after birth?
It is important to move around as much as possible after you have had your baby, and to avoid becoming dehydrated. A risk assessment will be carried out after the birth of your baby.
You may need to start enoxaparin injections for the first time after birth. This will depend on what risk factors you have for a VTE. Advice can be to have enoxaparin for 10 days after birth, or sometimes for six weeks after birth. If you were on enoxaparin before your baby’s birth, you are likely to be advised to continue this for six weeks afterwards.
If you are not able to move around after birth, you will be measured and fitted with leg pumps. For example, this could be after a caesarean birth. See the section below on foot / leg pumps for more information.
Can I breastfeed?
Yes. Enoxaparin is safe to take when breastfeeding.
Can I still develop a VTE whilst on blood thinners?
Yes. Blood thinners including enoxaparin greatly decrease your risk of blood clotting. But they do not prevent blood clots completely. The symptoms of VTE were discussed at the start of this leaflet.
Enoxaparin
Before injecting yourself with Enoxaparin
Check the expiry date. Do not use if date has passed.
Check the syringe is not damaged and the liquid inside is clear.
An air bubble in the syringe is normal. Do not press the plunger to remove it.
Injecting yourself with Enoxaparin
Wash your hands with soap and water.
Pull off the grey needle cap. Try not to bend the needle. Do not let the needle touch anything (this keeps it clean).
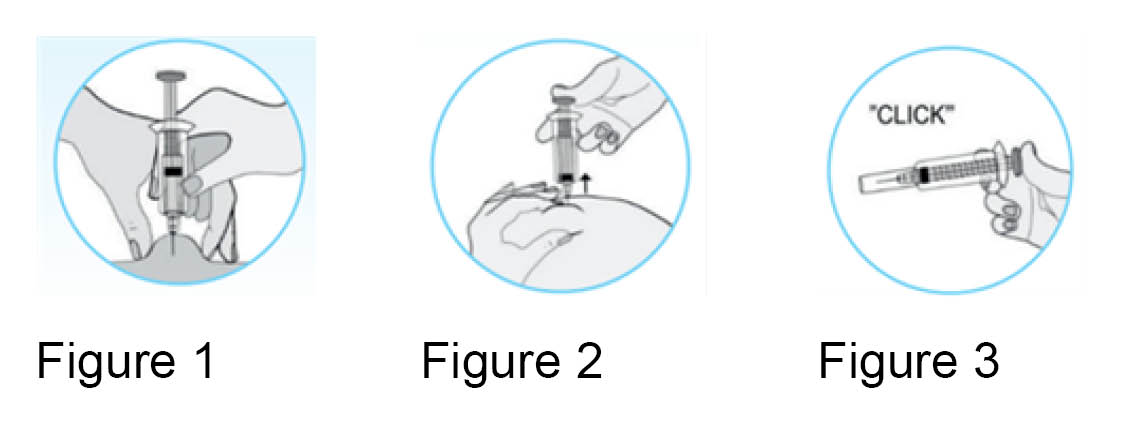
Hold the syringe in your dominant hand (the hand you write with). Pinch your skin with your other hand. Choose an area about 5cm away from your belly button (no higher) and away from any scars. Alternate the side you inject each time. See Figure 1.
Insert the full length of needle straight (at an angle of 90 degrees) into the area of skin.
Make sure to keep the skin pinched throughout the injection (see figure 2).
Press down firmly on the plunger. Injecting the medication slowly until the syringe is empty.
Keep the plunger pressed down and carefully remove the needle. When the needle is out you can let go of the area of skin. Do not rub your skin afterwards, this causes bruising.
Push down on the plunger until it clicks. This releases the protective needle cover (see figure 3).
Place the needle and syringe into the sharps bin. Keep this out of the reach of children.
When the sharps bin is full, you will need to go online to arrange collection. You can arrange collection through the Kent County Council web site. Scroll down to 'Clinical waste collection', and select your local council. Do not put the syringe in your household rubbish.
The preferred site for injection is your tummy. However, if you feel uncomfortable injecting your tummy you can inject into your thigh. Remember to alternate your injection site each time.
What are foot or leg pumps?
These are called intermittent pneumatic compression devices (IPCD). They have also been shown to reduce the risk of DVT by gently compressing your leg. This increases blood flow and stops blood pooling in your leg to create clots.
Your legs should be measured before fitting, to make sure the correct size sleeves are used. The sleeve should fit snugly round your leg or foot but you should still be able to get two fingers under it.
Sleeves should be worn 24 hours a day.
Sleeves should be removed daily for bathing and to check your skin.
Please check your sleeves are inflating regularly and are not switched off.
Let staff know if the sleeve feels either too loose or too tight.
Tell a member of hospital staff immediately if you have any of the following whilst wearing the sleeves:
tingling
numbness
pain
blistering, or
redness in your legs.
For more information on foot and leg pumps, please read our leaflet Preventing a blood clot whilst you are in hospital.
Who can I contact if I have concerns?
For help and advice, contact our Maternity telephone triage service on 01227 206737.
Further information
You can find further information on how to reduce your risk of a DVT and PE in hospital at Thrombosis UK.
Download the Thrombosis UK app, ‘Let's talk clots’ from the App Store or Google Play. They have an extensive section on VTE in pregnancy and after childbirth.
This link takes you to a video showing you how to inject enoxaparin yourself.
References

NICE. Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. NICE guidelines (NG89). Last updated 13 August 2019.
Community Pharmacy Hampshire & Isle of Wight. How to inject with Inhixa (enoxaparin). July 2019.