Radiofrequency denervation of facet joints: The Kent Centre for Pain Medicine and Neuromodulation
Information for patients
You have been referred to the Pain Clinic for radiofrequency denervation of facet joints. This leaflet will explain:
what facet joints are
how radiofrequency denervation can help with chronic pain relief
what the side effects could be, and
what will happen during and after the procedure.
If you have any questions after reading this leaflet, please speak to your GP or other relevant healthcare professional.
What are facet joints?
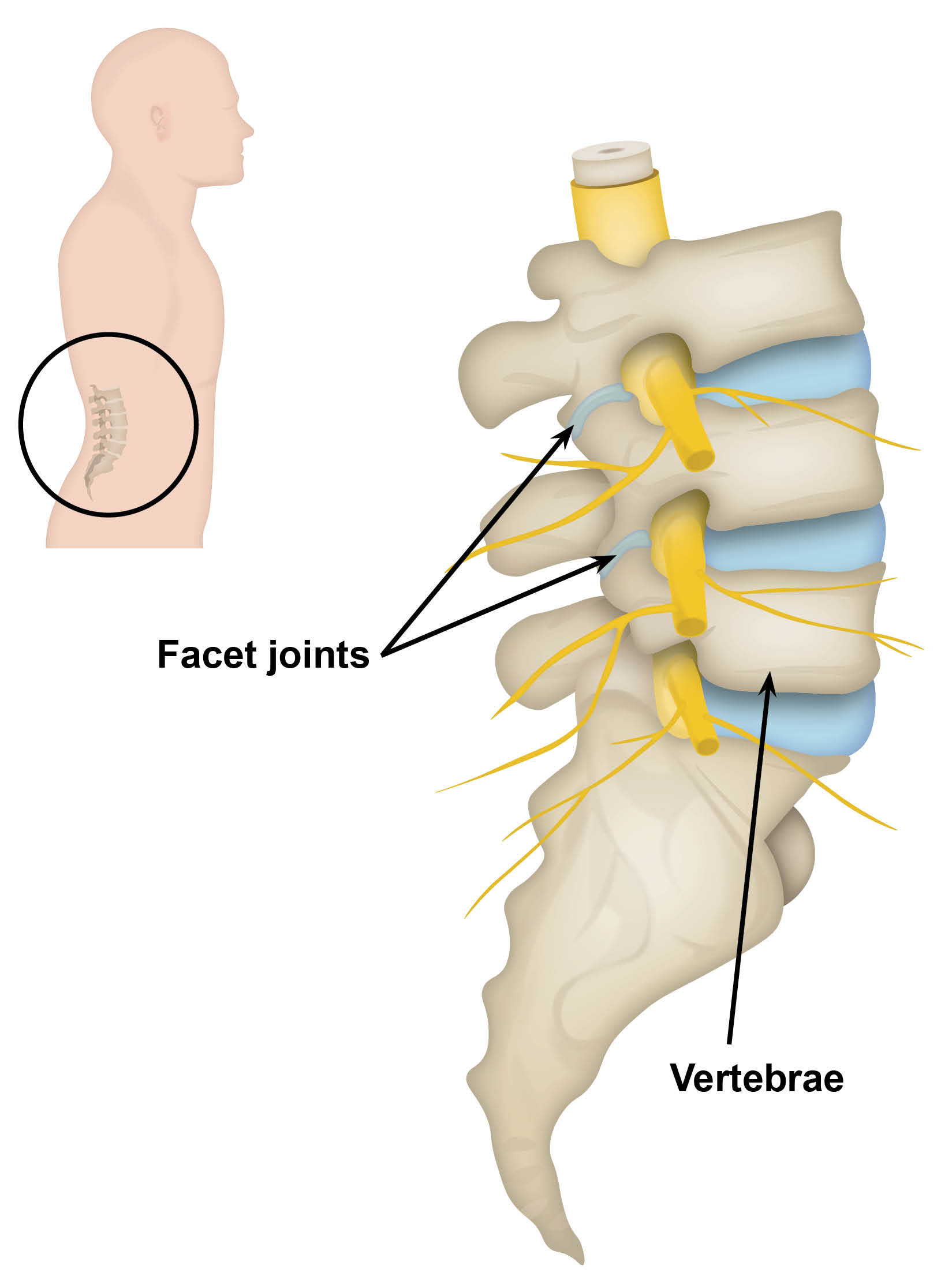
Facet joints are small linking joints. They connect the bones of the spine, also known as vertebrae. They work with the discs, and are responsible for controlling the twisting and sideways movements of the whole spine. Facet joints are found on each side of the spine.
These joints usually cause no pain at all. However, if they become inflamed or arthritic (also known as ‘wear and tear’) they can become painful.
What is radiofrequency denervation?
During radiofrequency denervation the nerve fibres supplying painful facet joints, are selectively destroyed by heat. Radio waves produce the heat, which is delivered through an electrode, using the tip of a heated needle.
Why am I having this procedure?
Before radiofrequency denervation is considered, you will have a test block of the nerves supplying your facet joints to confirm your diagnosis (medial branch blocks). You and your doctor think that you have had significant pain relief from this treatment, but the pain relief has worn off.
Radiofrequency treatment can last much longer than injections. Unfortunately it does not always work as well as we would like. If the relief you had from the medial branch blocks was good, the chances are that radiofrequency treatment will work as well. This cannot be guaranteed.
What happens during my procedure?
Radiofrequency denervation is carried out as a day case procedure, so you can go home on the same day.
The procedure is performed in Day Surgery to minimise your risk of getting an infection. Shortly before your procedure we will ask you to change into a theatre gown.
The procedure
The procedure is carried out under x-ray guidance. This allows the doctor to see the specific level to be treated. You must tell your consultant if there is any chance that you may be pregnant, as x-rays may harm your baby.
A self-adhesive foil plate will be placed on your thigh. To make an electric circuit, the plate is connected to the radiofrequency machine.
We will ask you to lie down on your front. Your doctor will clean the area with an antiseptic solution. This can feel cold.
A cannula (a small flexible tube) will be placed in the back of your hand or arm. You may be given something to make you sleepy.
A local anaesthetic is injected at the site of the procedure. This may sting to start with, before your skin goes numb.
You must keep still during your procedure, as a special hollow needle will be carefully inserted under x-ray guidance into the correct position.
The correct position of the probe is checked with two tests.
Sensory: you may feel tightness, pressure, or tingling in your back.
Motor: you may feel some throbbing in your back.
When asked, you must tell us straightaway how you are feeling. If there is throbbing in your leg / arm or you have got no sensations on the tests, the probe will be repositioned.
The machine will be set to lesion the nerve. The machine does this by heating the nerve for about one and half minutes. During this time you may feel some pain at the site of the procedure.
The above may be repeated at different levels on your spine.
After the probe is removed, local anaesthetic and possibly steroids are injected. This will relieve any discomfort you are feeling following your procedure.
What are the possible side effects?
There may be some pain, bruising, and / or bleeding at the needle site.
You may feel a little unsteady when you first stand.
The procedure may make your pain worse. This should settle within one month.
There is a small risk of infection at the site of your injections. This may need antibiotic treatment. Contact your GP or call NHS 111 if:
there is warmth, redness, or tenderness at your injection sites, or
you feel hot and unwell.
You may have some leg weakness or numbness, which should settle within a few hours.
Very rarely, there is a risk of temporary or permanent nerve damage.
If steroids are used:
Female patients may temporarily have irregular periods.
Diabetic patients may have unstable blood sugar levels.
Rarely, some patients may have mood changes.
What will happen after my injections?
A small dressing will cover the injection sites. You can remove this dressing after 24 hours. Do not worry if it falls off sooner.
You will be discharged home 1 to 2 hours after your procedure.
You must not drive for 24 hours following your procedure. Please arrange for someone to drive you home from the hospital. We also strongly recommend that you have someone stay at home with you until the following day.
You may notice an immediate improvement, but this improvement can be delayed for a few days. Sometimes there may be a slight increase in pain for 24 to 48 hours. Steroids work slowly, so even if your procedure has worked well, nothing may seem to happen for several days. It can sometimes take several weeks before you notice the benefits from this treatment.
Will I need a follow-up appointment?
A telephone appointment will be made for a nurse to call you about 3 months after your procedure. You will be told by letter the date and time of this appointment. During your appointment, the nurse will review the outcome of your procedure and plan what happens next.
If you continue to have good benefit from the procedure, you may be discharged from the Pain Clinic.
Further information
If you have any concerns about the information in this leaflet or your procedure, please phone the Pain Clinic.
Kent Centre for Pain Medicine and Neuromodulation (direct lines)
Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783049Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 235094William Harvey Hospital, Ashford
Telephone: 01233 616691
Useful information
East Kent Hospitals. The Kent Centre for Pain Medicine and Neuromodulation: medial branch blocks
East Kent Hospitals. The Kent Centre for Pain Medicine and Neuromodulation: medial branch blocks (fast-track denervation pathway)