Pulmonary embolus
Information for patients
What is a pulmonary embolus?
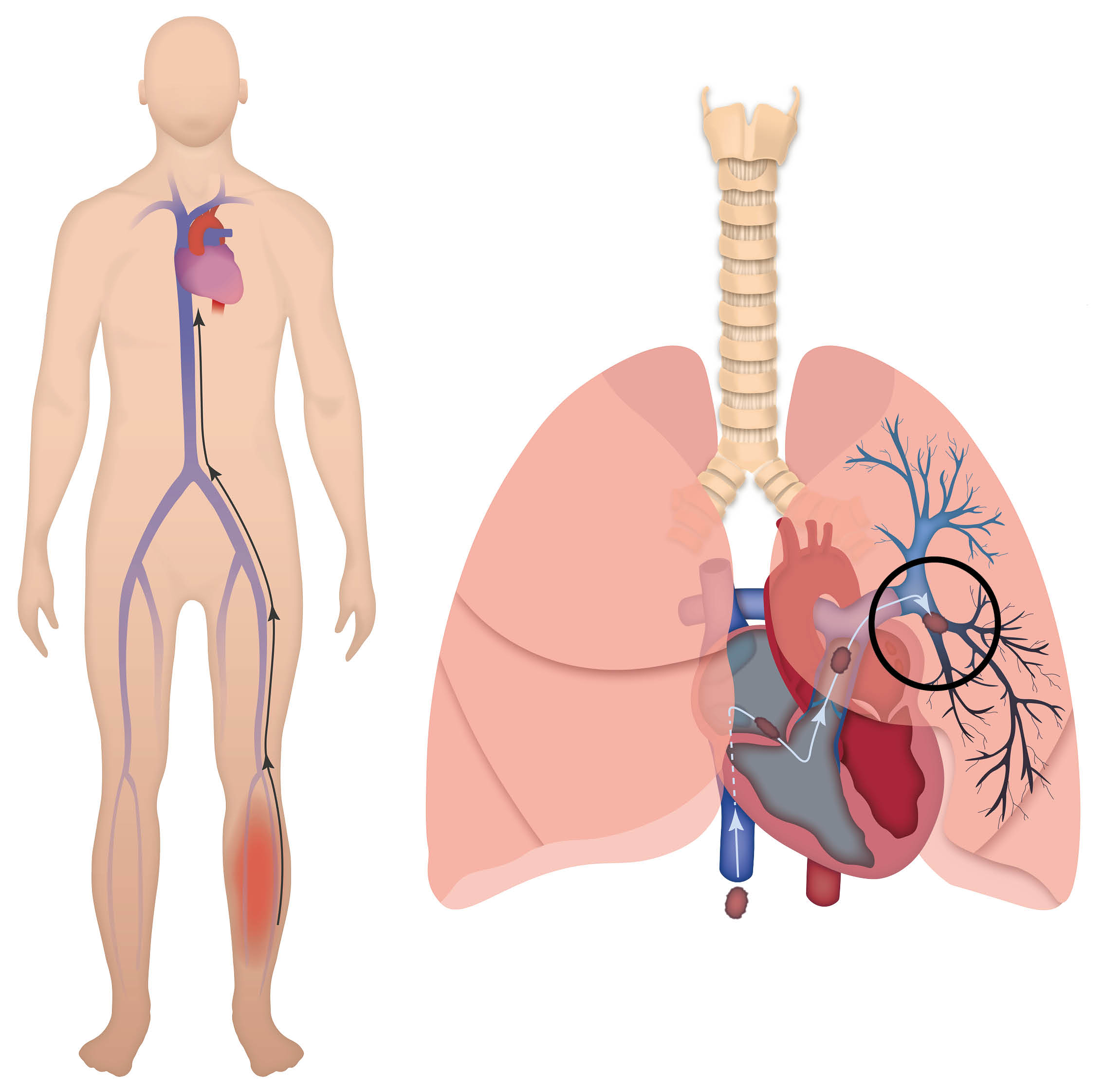
A pulmonary embolus (PE) is a blood clot which is lodged in one or more of the pulmonary arteries in the lung.
A PE usually originates from a deep vein thrombosis (DVT). A DVT is a blood clot in the deep veins, usually in the leg.
What are the symptoms of a PE?
Symptoms will vary depending on the size and position of the blood clot. Not everybody will have all of these symptoms.
Shortness of breath, either at rest or on exertion. This is due to the blood clot restricting the arterial blood flow through the lungs. In some cases, oxygen may be needed to help with this.
An increased heart rate. This is due to the heart having to work harder to make sure enough oxygen is transported around the body.
Chest pain. This may be constant or only when breathing deeply. This is due to inflammation in the lungs or lining of the lungs.
Occasionally, coughing up blood or blood stained sputum. This is rare and will stop.
What tests will I have in hospital?
Vital signs monitoring: your oxygen level, heart rate, blood pressure, respiratory rate, and temperature may be checked regularly. This helps to see how hard your heart is working and how effective your breathing is. It may also help to rule out infection.
Blood tests will be taken to make sure your body is able to cope with the medication needed. Inflammatory markers may be measured to make sure there is no infection.
ECG (Electrocardiogram) shows the electrical activity of your heart. Whilst often not affecting the heart directly, a PE can sometimes be suggested by an ECG.
A chest x-ray is not able to diagnose a PE, but it can rule out other possible conditions, such as a chest infection.
VQ or CTPA Scan: a VQ (Ventilation and Perfusion) scan looks at the air and blood flow in your lungs. A CTPA (Computed Tomographic Pulmonary Angiography) looks at the arteries in your lungs. Either of these scans may be used to diagnose a PE.
Each test involves a cannula being inserted into a vein in your arm, and an injection of a ‘dye’ which allows us to see if you have a PE. Sometimes the ‘dye’ used may give the feeling that you are urinating when you are not; this usually stops quickly.
Occasionally, after a clinical assessment other investigations will need to be done. Not all tests will need to be done urgently.
Once diagnosed, what is the treatment of a PE?
Your body will naturally break down the blood clot, but in order to do so safely you will need to take anticoagulant medication. Anticoagulant medication will thin your blood to prevent the blood clot from getting bigger or moving, or new clots from forming.
Anticoagulation may be given as warfarin tablets, heparin injections, a combination of the two, or a newer oral anticoagulant class called direct acting anticoagulants (DOAC).
Warfarin tablets come in three different colours and doses:
1mg: brown tablets
3mg: blue tablets
5mg: pink tablets.
When taking warfarin, you will have regular blood tests to monitor your INR (International Normalised Ratio). This is a measure of how long it takes for your blood to clot.
The dose of warfarin you are prescribed will differ according to your INR. Your specialist will tell you what to take and when, depending on the results of your blood test.
Heparin injections are given according to your weight and kidney function. Heparin is usually given once a day (occasionally twice daily) into the skin of your abdomen (tummy). You may be shown how to do this yourself, or a nurse may do it for you.
Rivaroxaban is an oral anticoagulant. If taken from when the blood clot is diagnosed, it is taken twice a day for three weeks and then once each day after that. After the first three week period, the dose usually does not change and there is no need for blood tests to monitor its effect.
Your kidney and liver blood tests will need to be checked before and every three to six months during treatment with this drug, as this is how your body processes the drug.
Apixaban is an oral anticoagulant. If taken from when the blood clot is first diagnosed, it is taken at a higher loading dose for one week, and then continues on a fixed dose twice daily after that. After the first one week loading period, the treatment dose usually does not change and there is no need for blood tests to monitor its effect.
Your kidney and liver blood tests will need to be checked before and every three to six months during treatment with this drug, as this is how your body processes the drug.
Other oral anticoagulants are dabigatran, edoxaban, and acenocoumarol. You will only be advised to use these if they have advantages for you compared to the ones mentioned above. You should only be on one anticoagulant.
What are the side effects of anticoagulants?
All anticoagulants increase your risk of bleeding, as they thin your blood. Be extra careful when cutting your nails, shaving, or using sharp implements. If you do have any bleeding, apply extra pressure on the affected area and get medical help if it does not stop.
Some people complain of feeling cold when taking anticoagulants.
Heparin can cause your platelets (a clotting component in the blood) to drop in the first few weeks of taking it. Your blood will be tested regularly when you first start taking heparin to see if this happens.
There are some medications (such as aspirin), which often should not be taken with anticoagulants; your specialist will advise you on this. Some herbal medications and food also interact with certain anticoagulants; your specialist will advise you on this aswell.
If your doctor or nurse prescribe you any new medication, you should tell them that you are taking warfarin, so that they can check for any possible interactions.
What will happen if I do not want to take anticoagulants?
You are strongly advised to take the anticoagulants. If you do not take them, the blood clot could get larger, causing further damage to your lung and further restrict your breathing. The clot could also break up and block further arteries.
If untreated, a PE can be fatal. Most people who have a PE and take anticoagulants usually recover without complications.
Do I need to stay in hospital?
Not necessarily. This depends on the size and position of your PE, and how it affects you.
If you have a fast heart rate, fast breathing, or are in severe pain, you may need to stay in hospital for a few days. This may be between one and seven days.
If you are relatively well with your PE, you may be treated as an outpatient on the Ambulatory Care Pathway. If you want more details about the Care Pathway, please speak to a member of staff.
How long will I be on the anticoagulants?
You will need anticoagulant medication for at least three months.
If you are taking warfarin, once your INR becomes ‘therapeutic’ (has reached the desired level), you will be referred to the Anticoagulant Clinic as an outpatient. This is usually between five and seven days after starting warfarin. The clinic staff will continue to monitor your INR and warfarin. Once your INR is ‘stable’ (remains at an acceptable level), you will be referred to an Anticoagulant Clinic closer to your home.
If you are on rivaroxaban, apixaban, or heparin injections, you will be referred to the Anticoagulant Clinic early on in your treatment. The specialist staff at the clinic will tell you how long you will be treated for and arrange follow-up appointments as needed.
What can I do to help my recovery?
Listen to your body. If you do anything that makes you feel breathless or increases your pain, stop.
Do not drive, go on long walks, or exercise (such as gardening or going to the gym), until you have spoken to your specialist. You will be able to return to your normal lifestyle in time.
Until the PE starts to improve, you may feel some discomfort. Take painkillers which have been prescribed for you. Avoid over-the-counter medicine unless you have discussed this with your specialist.
When sitting, keep your legs elevated (raised), ideally above the level of your hips, unless told otherwise by your specialist. This will help with your blood flow and reduces leg swelling.
Look after yourself. Eat a healthy diet and drink plenty of fluid. To begin with you may not be able to move around as normal, due to pain and breathlessness, and this will increase your risk of getting constipation.
When should I call for help?
If your symptoms get worse (chest pain increases or your breathlessness worsens) go to your nearest hospital to be checked. If severe, call 999.
If you have any bleeding which you cannot stop, go to your nearest hospital. If you cough up blood, contact your specialist, your GP, or call NHS 111 for advice.