Pterygium and pterygium surgery
Information for patients from South Devon Healthcare NHS Foundation Trust and East Kent Hospitals’ Ophthalmology Department
This booklet provides information about pterygium, and aims to help you make a decision about surgery if needed. The leaflet provides information about what to bring to your appointment and what will happen during your visit.
This leaflet is not meant to replace the information discussed between you and your doctor, but can act as a starting point for such a discussion or as a useful reminder of the key points.
Some of the words used may seem confusing and scientific. At the end of this booklet you will find a list of explanations of commonly used medical words and phrases.
Please speak to your specialist if you have concerns about your condition or treatment.
If after reading this booklet you have any questions, please let us know.
What is a pterygium?
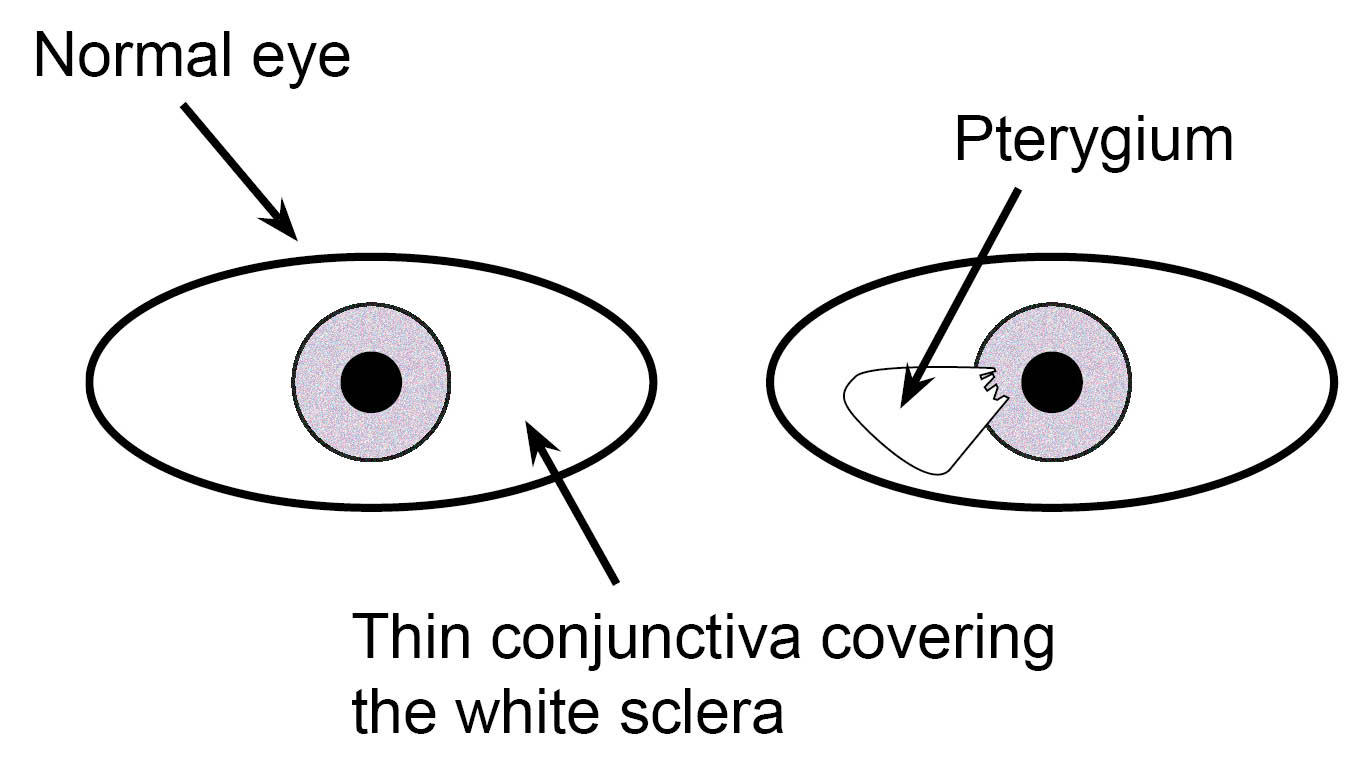
A pterygium is degenerative conjunctiva on the surface of the eye, that grows over the front of the cornea (the clear window at the front of the eye).
A pterygium usually grows very slowly over many years. It is more common in people who have been exposed to a lot of sunlight during their lifetime.
What are the symptoms?
A pterygium may cause one or more of the following.
Dissatisfaction with the cosmetic appearance of your eye (you may not be happy with the appearance of your eye).
Redness of your eye.
Discomfort in your eye, which is usually a dry or gritty feeling. This is caused by drying of the normal tear film on the surface of the pterygium or next to it.
In extreme cases, a pterygium can grow over the centre of your cornea and can cause blurred vision or scarring. This may restrict the movement of your eye, causing double vision.
Will I have an anaesthetic?
Pterygium surgery can be done under local anaesthesia (you are awake) or general anaesthesia (you are asleep). Which anaesthesia you have is based on how long or difficult your doctor thinks the operation will be, your suitability for different sorts of anaesthesia, your own preference, and your surgeon’s advice.
A routine pterygium operation would last about 45 minutes and can usually be performed comfortably under local anaesthetic. However, a recurrent pterygium (one that has re-grown after a previous operation) usually needs more extensive surgery and a general anaesthetic is recommended.
You will usually be able to go home on the day of your operation, but you may be asked to return for an eye check the following day.
What can happen during pterygium surgery?
-
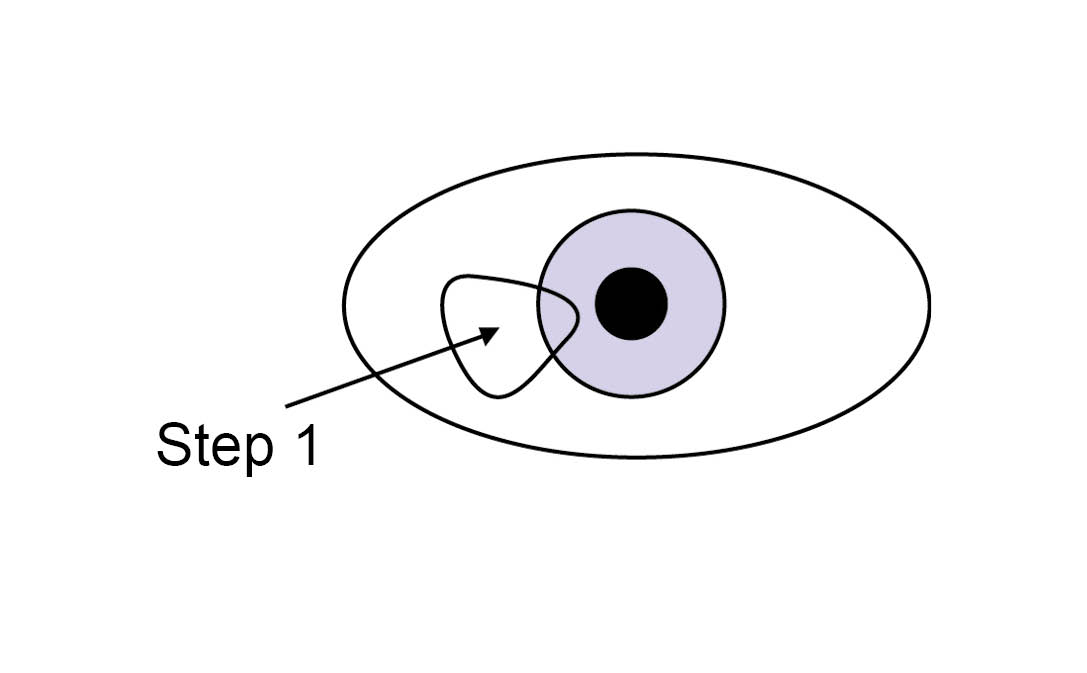 Step 1: the pterygium is removed from the outer layers of the eye, leaving a bare surface.
Step 1: the pterygium is removed from the outer layers of the eye, leaving a bare surface. -
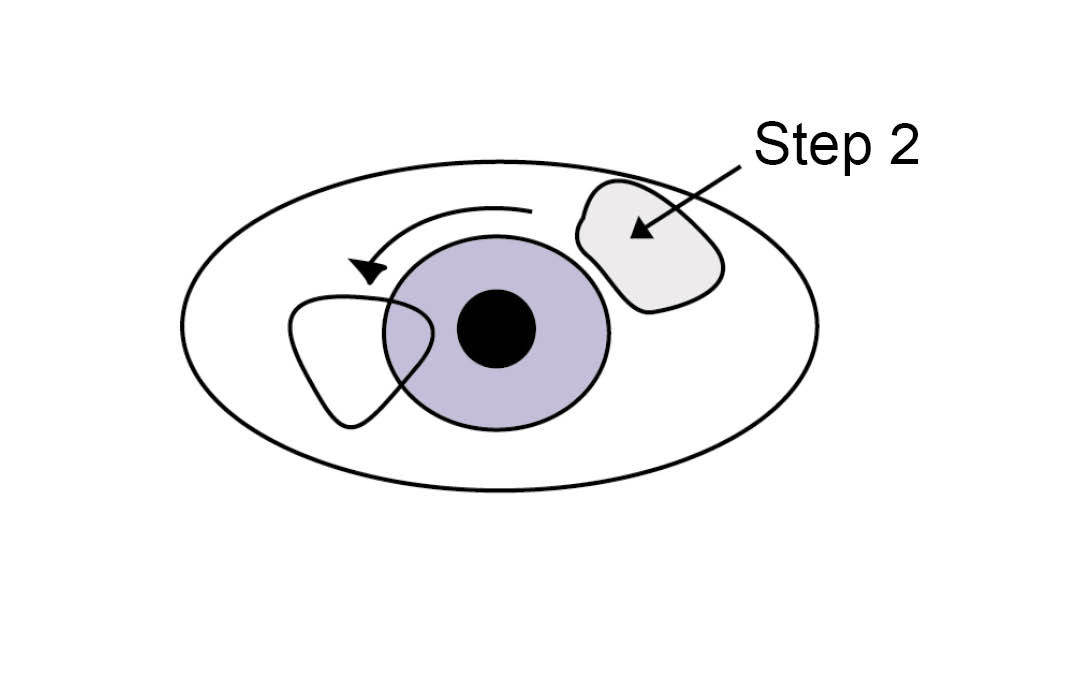 Step 2: a graft of normal conjunctiva is then taken from the surface of the eye.
Step 2: a graft of normal conjunctiva is then taken from the surface of the eye. -
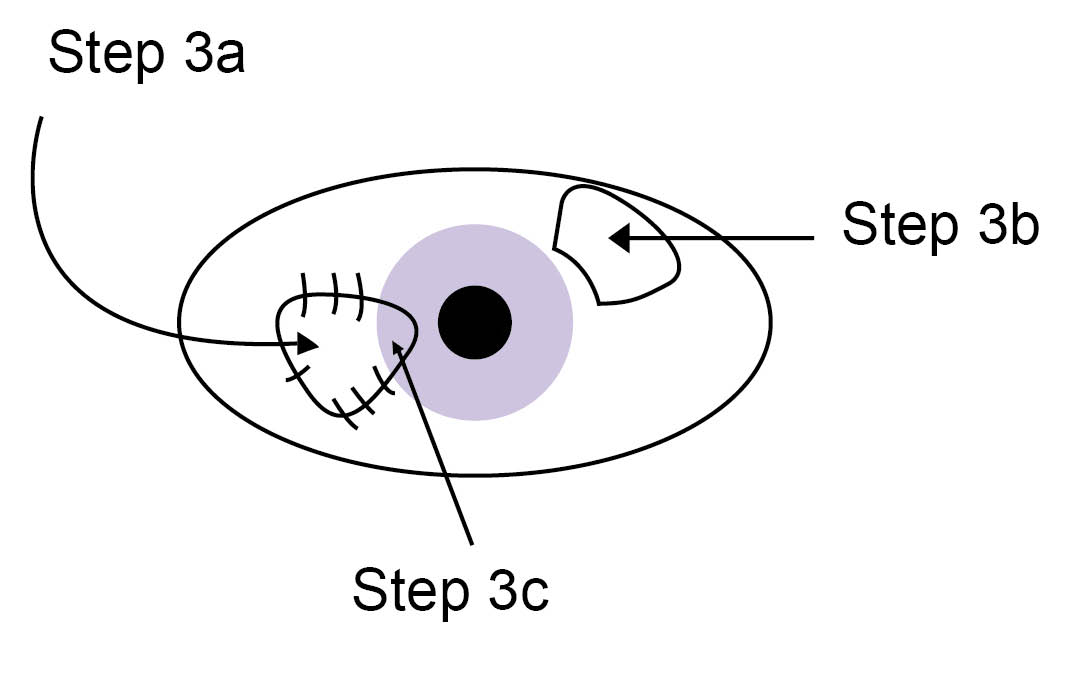 Step 3a: the conjunctival graft is stitched into place to cover the bare area of the sclera. Step 3b: the donor site usually heals over several days without problems. Step 3c: the bare corneal surface usually heals in 24 to 48 hours.
Step 3a: the conjunctival graft is stitched into place to cover the bare area of the sclera. Step 3b: the donor site usually heals over several days without problems. Step 3c: the bare corneal surface usually heals in 24 to 48 hours.
A recurrent pterygium may need additional surgical techniques. This could include the use of other transplantation materials (such as amniotic membrane or sclera), the use of drugs on the eye (such as mitomycin C or 5-fluorouracil), or radiation treatment to try to prevent another recurrence. The choice of techniques depends on the details of each individual case. However, in general the risks of surgery for a recurrent pterygium tend to be higher and success rates lower.
Consenting to your operation
The following gives you information you should know before agreeing to surgery. We encourage you to read this and ask any questions which may arise before signing the consent form. You should only sign the consent form if you are satisfied with the explanations about the operation and you understand the benefits and risks. Remember that you can withdraw your consent for treatment at any time.
What are the benefits to removing a pterygium?
The main reason for removing a pterygium is to prevent future loss of eyesight, by stopping the pterygium from growing over the central area of your cornea. Other symptoms such as redness or discomfort are not as easily treated by surgery, and where possible are best treated using simple methods such as the use of lubricant eye drops.
What are the risks?
As with every operation, pterygium surgery has risks.
Success cannot be guaranteed.
All serious complications are rare.
What complications can occur during my operation?
Because the operation only involves the outer layers of the eye, pterygium surgery is relatively safe compared to many types of eye surgery.
One of the eye muscles lies partly underneath the operation site. It is possible, though unlikely, that this muscle could be damaged during your operation, causing double vision and needing further surgery. This complication is more of a concern when removing a pterygium that has re-grown after a previous operation, when there is much more scarring and the muscle may be difficult to see.
Very rarely, the internal parts of your eye could be damaged, causing loss of eyesight. This is more of a concern when operating on an eye that has already had surgery or where the eye has been damaged by previous injury or by other eye diseases.
What complications and side-effects can happen after my operation?
Pain or discomfort
Some pain is very common in the first 24 to 48 hours after surgery. This is because the corneal surface, previously covered by the pterygium, is left bare (see diagram above) and takes 24 to 48 hours to heal. If there are no medical reasons why not, you may take simple painkillers such as paracetamol.
Frequent use of eye lubricants may also help. Dissolving stitches may cause a gritty feeling for several weeks. The inflammation caused by surgery may take several weeks or sometimes months to settle fully. If this happens your eye may still be slightly red and feel mildly dry or gritty.
After corneal surgery the eye surface is often slightly bumpy. The tear film, which keeps the eye moist, tends to dry out on the surface of the bumps. If the drying is severe your eye can be more likely to get infected or ulcerated. Lubricant eye drops are often needed in the first few months after surgery, and possibly long-term in some cases.
Cosmetic appearance
The cosmetic appearance following surgery is usually very good, although not absolutely perfect. If you look very closely you may see differences in the normal patterns of the red blood vessels between each eye. Removal of the pterygium usually leaves a faint scar on the cornea that may be visible.
Poor eyesight
After the operation the corneal surface, previously covered by the pterygium, is often slightly bumpy and scarred. This means that in cases where the pterygium has grown over the central cornea, the vision may remain poor even when the pterygium has been removed.
Recurrence of the pterygium
The chance of a pterygium coming back after the first operation is between one in six and one in 20 approximately.
Corneal ulceration or infection
Severe problems, such as corneal ulceration or infection, are rare but may need intensive treatment such as antibiotics. These problems can lead to scarring and opacity of the cornea or, very rarely perforation of the eye. If the ulceration is severe a corneal transplant may be needed, sometimes as an emergency.
Further surgery
Further surgery is unlikely but patients who need further surgery, including surgery for recurrent pterygium, may also have complications arising from the additional surgery or treatments.
These complications could include corneal or scleral thinning or ulceration, perforation of the eye, cataract, glaucoma, poor eyesight, or complete loss of eyesight in the operated eye, loss of the operated eye or inflammation in the other eye (extremely rare).
What happens during pterygium surgery?
You will be given some drops to numb the front of your eye, and the skin around your eye will be cleaned with an antiseptic that may feel cold. You may be asked to look at a mark on the ceiling, this helps you keep your eye still whilst the anaesthetic is being given.
The local anaesthetic mixture goes into the corner of the eye socket and spreads from there to make the whole eye numb for several hours.
A small pad applying light pressure may be placed over your eye for about five to 10 minutes, whilst the anaesthetic starts working.
You will then be taken in to theatre. You will be lying flat in theatre with your head supported on a special pillow.
You may feel sleepy but we would like you to stay awake throughout your operation. The anaesthetic will keep your eye numb and still, but it is important that you keep your head and body still. We will do our best to make you comfortable before starting the operation.
After we have cleaned around your eye we will place a sterile sheet over your head and upper body. This will be held away from your face and you will have plenty of fresh air blowing under the sheet. A member of the theatre staff will always be close by in case you feel any discomfort during your operation.
After your operation you will return to the Eye Surgery Unit with a pad over your eye whilst you wait to go home.
What happens after my operation?
We may ask you to remove the eye pad yourself. Otherwise it should stay in place until you see us the following day.
It is common to feel slightly unsteady on your feet while you get used to the eye pad, so please take care when moving around and do not rub your eye.
We usually check your eye one to two days after surgery, and then again one week after surgery.
How will my eye feel after my operation?
Although your eye can be painful to start with, the pain and discomfort should quickly improve in the first 24 to 48 hours after surgery. After the first 24 to 48 hours there is usually some mild discomfort, which then improves slowly over time.
Your eyesight in the operated eye is often blurry to start with, but it improves steadily as the surface of your eye heals. If at any stage your eye discomfort or redness increases, or your eyesight starts to become worse, please contact us (see contact details at the end of this leaflet).
How do I use my eye drops and ointment?
Make sure you know which eye drops or ointments you should be taking. Please remember the names, or if you cannot remember the names write them down or bring the drops with you to every appointment. This is so your doctor can discuss your treatment with you. If you are using any eye treatment in the eye to be operated on before your operation, please check with your eye specialist whether it will need to be continued after your surgery.
In the first week, eye treatment usually consists of:
an antibiotic such as chloramphenicol (drops or ointment) four times daily; and
an eye lubricant such as lacrilube or celluvisc to be used frequently, at least four times daily, in between the times when you use the antibiotic.
This means that you will be using eye drops or ointment at least every two hours in the first week.
In the second week, if the surface of your eye is healing well, you will start using anti-inflammatory drops. These will need to be continued with the lubricants for at least two months, unless you are told otherwise. The antibiotics are usually stopped two weeks after the operation.
If you run out of eye drops or ointment do not wait until your next appointment, please ask for a repeat prescription from your GP.
You should continue to use any other regular medication (including any treatment for your other eye) as usual.
How do I avoid infection after surgery?
Remember that your eye surface is vulnerable to infection until it has healed fully. This means that you must take every precaution to keep your eye clean.
If you feel grittiness or discomfort in bright light, this suggests that your eye has not fully healed.
Do not do any activities that may introduce dirt or dirty water in to your eye.
Wash your hands before touching your eye.
Do not swim until you have been cleared to do so by your doctor.
Keep the nozzles of your eye drop bottles or ointment tubes clean, by not touching them with your eye or fingers.
When can I start driving again?
Take care to avoid accidental injuries. This advice applies particularly to driving or doing any other dangerous activity, such as operating machinery.
Avoid driving for at least 48 hours after your surgery. If you still meet the legal eyesight requirements for driving, and if your insurers are told of your surgery and are providing insurance cover, you can drive after 48 hours.
Do not drive if you have double vision or if your eyes are uncomfortable or watering.
When can I resume normal activities?
Please do not rub your eye or take part in any activities that carry an extra risk of eye injury (such as contact sports) for a month. Wear eye protection for activities such as grinding, hammering, or chiselling. Avoid working with any chemicals that may irritate your eye, until the surface of your eye has healed fully.
If you are uncertain whether you can continue one of your normal activities, please ask us.
When can I go on holiday?
Remember to tell your insurance company about any recent eye treatment. Remember that insurance policies may not cover pre-existing eye problems or recent surgery.
How do I clean my eye?
It is normal for your eyelids to be sticky after your operation, however the stickiness should improve within the first two weeks. Use a clean piece of cotton wool and cooled previously boiled water to clean your eyelids. Wipe gently from the nose outwards then throw away the cotton wool and repeat as necessary. Use separate cotton wool for each eye. Do not try to clean inside your eyelids.
Commonly used words and phrases
Cornea: The clear window at the front of the eye.
Conjunctiva: The thin, semi-transparent tissue (membrane) that lines the inner surfaces of the eyelids and the outer surface of the sclera.
Sclera: The tough opaque white outer coat that together with the clear cornea makes up the eyeball.
What should I do if I am worried about my eye?
Please remember that most patients have a very good result from their surgery. However, if you develop any problems following your operation, please call us using one of the numbers below.
Kent and Canterbury Hospital, Canterbury
Waiting List Co-ordinator
Telephone: 01227 866444Ophthalmology Suite
Telephone: 01227 866493
Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Waiting List Co-ordinator
Telephone: 01843 234364Day Surgery
Telephone: 01843 234499
William Harvey Hospital, Ashford
Waiting List Co-ordinator
Telephone: 01233 616757Channel Day Surgery Centre
Telephone: 01233 616263
We hope you have found this booklet informative and useful, and that it has helped to make your experience of surgery as relaxed as possible.
We regularly update the information and if there is anything we have left out or could have done better, please let us know.
This leaflet is produced with grateful acknowledgment to the South Devon Healthcare NHS Foundation Trust.