Prostate disease and TURP (Trans Urethral Resection Prostate)
Information for patients from the Urology Department
What is the prostate gland?
The prostate gland is part of the reproductive system in men. The average prostate gland is the size of a walnut, and lies in front of the rectum and at the bottom part of the bladder. The prostate surrounds the urethra, the tube that carries urine from the bladder out through the penis.
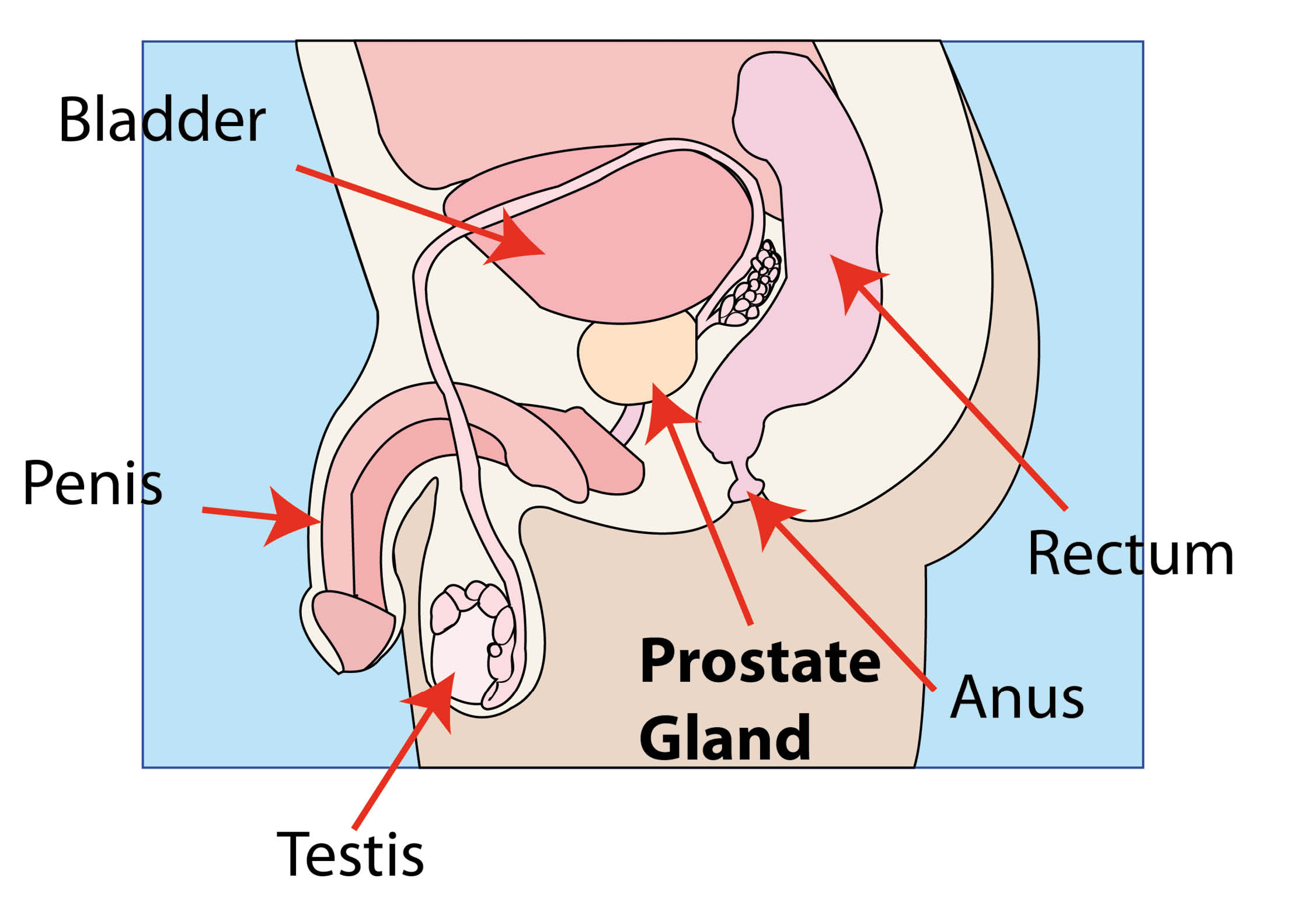
The main role of the prostate is to produce fluid for the sperm to travel in. The prostate fluid mixes with sperm from the testicles to become semen and is then transported out through the urethra with ejaculation during sexual intercourse.
Why have I been referred for this procedure?
Your doctor has either examined your prostate using a finger examination of your rectum, and found a suspicious lump. Or you have had a blood test which has shown a raise in the prostatic specific antigen (PSA).
The above findings may - but only possibly - indicate that cancer of the prostate is present. The only certain way of knowing if your prostate is cancerous, is to remove a piece of abnormal prostate tissue (a biopsy) which will be examined in a laboratory.
What is Benign Prostate Hyperplasia (BPH)?
Prostate enlargement (hyperplasia) is a non-cancerous (benign) overgrowth of the prostate gland. The prostate gland surrounds the outlet of the bladder (the urethra) and when enlarged it squeezes the urethra and narrows the opening, preventing the urine from easily leaving the bladder.
What are the common signs and symptoms of prostate enlargement?
Early symptoms
Your urine does not flow as fast or as strong as it used to.
You pass urine more often.
When you have an urge to pass urine, it is urgent and needs to be done without delay.
Many men have to get up more often at night to urinate.
Later symptoms
Your bladder does not empty completely.
The flow of your urine weakens and slows to a dribble.
Other problems may include blood in your urine and infection of your bladder or kidney.
How is prostate enlargement diagnosed?
Usually the diagnosis can only be made by taking a record of past and present events (history), carrying out a physical examination, and taking some blood samples. Other investigations can include the following.
Uroflow (flow rate test) to measure how fast your urine is passed.
Residual urine is the amount of urine that is left in your bladder after you finish urinating; this can be measured using an ultrasound scan.
Cystoscopy. Your urethra and bladder can be examined using a special telescope (called a cystoscope).
An ultrasound scan is harmless sound waves aimed at your prostate. The sound waves bounce back (echoes) and are seen as pictures on a screen. Ultrasound is a convenient and harmless way to examine your prostate gland. The probe can either be put on your abdomen (tummy) or inside your rectum.
Will I need an operation?
Your treatment will depend on how severe your symptoms are and whether the enlargement of your prostate is causing you other problems. Your age, sexual activity, and general health will be taken into consideration. Sometimes the flow of urine can be improved with medication.
We usually advise you have an operation if any of the following happen.
Severe obstruction
Early signs of kidney damage
Repeated urinary tract infections
Retention of urine (unable to pass urine)
Repeated bleeding when passing urine.
Are there any alternatives to surgery?
Medication.
Minimally invasive surgical options such as Urolift or Rezum Steam Therapy.
Other endoscopic surgical options such as laser vaporisation or enucleation.
Catheterisation - either permanent or passed regularly, so you can drain your bladder yourself (self catheterisation).
Open surgery (with a cut in the skin) is only needed in extremely rare circumstances.
Your consultant will discuss your options with you before any decisions are made.
What is a transurethral resection of the prostate (TURP)?
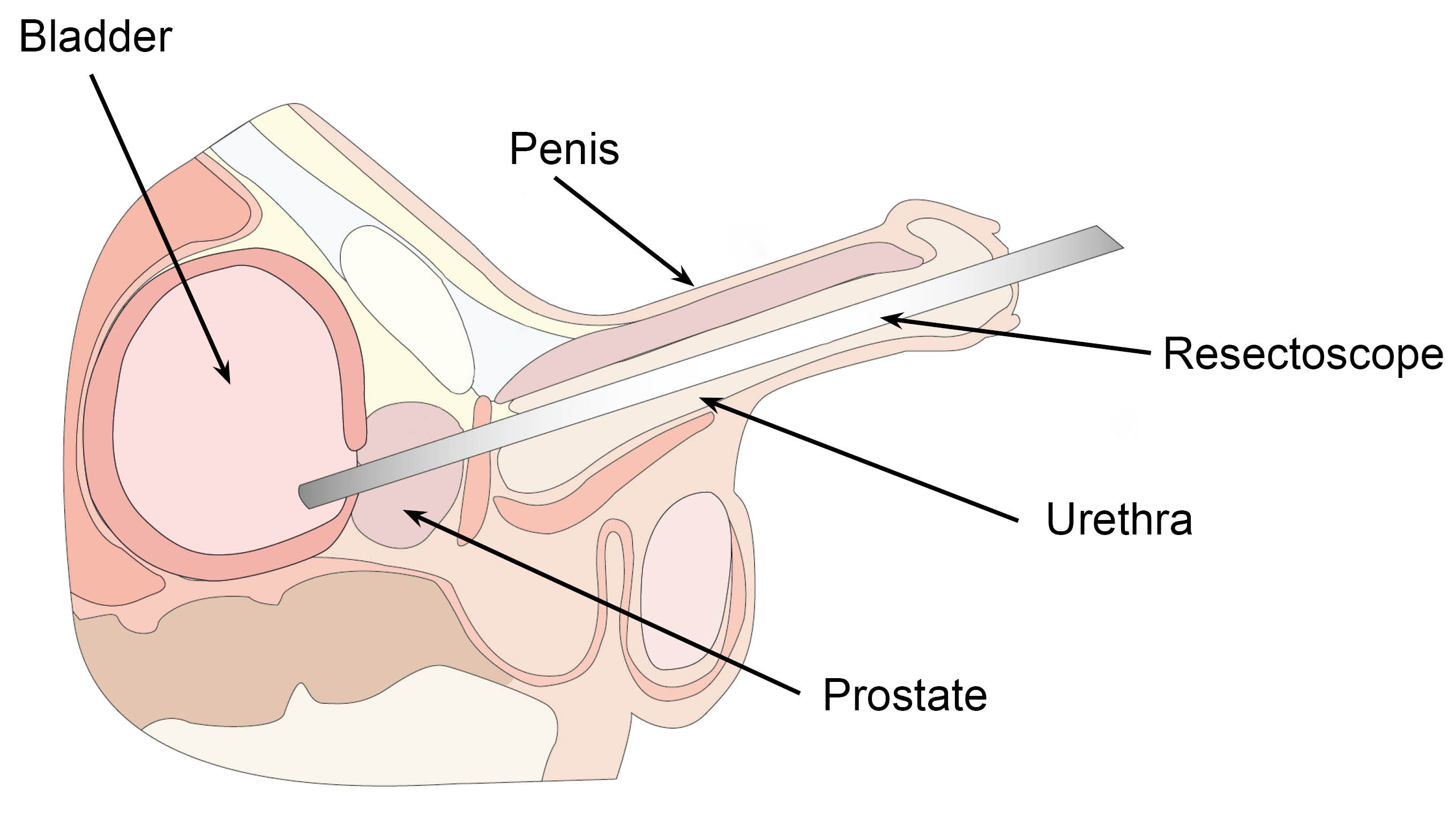
This operation is performed through a special telescope (a cystoscope / resectoscope) which is passed up the tube inside your penis (the urethra). No cut (incision) is made on the outside of your body.
The cystoscope with an electrical cutting device is used to shave down and remove the obstructing part of your prostate gland.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
Will I have a general anaesthetic?
This operation is normally carried out under general anaesthetic (you will be asleep) or spinal anaesthetic (you are numb from the waist down). You will discuss with your consultant which anaesthetic you will have before your operation.
How long will I stay in hospital?
The operation itself can take up to one hour, depending on the amount of prostate tissue being removed.
How long you need to stay in hospital will depend on the type of operation you have, but can range from 24 hours to several days. Your consultant will advise you.
What happens after my operation?
After your operation a tube called a catheter is passed up your urethra to drain urine from your bladder. This will remain in place for a few days.
TURP is usually performed for benign (non-cancerous) growth of the prostate. However, all of the prostate tissue that is removed during your operation will be sent to the laboratory. If there is any problem your surgeon will discuss this with you.
When will my catheter be removed?
The catheter may be in place for a few days or removed the day after your procedure to drain your bladder.
Note: it is sometimes necessary to send some men home with an indwelling urinary catheter for a few weeks to allow things to settle down before removing their catheter. The management of the catheter will be fully explained to you before you go home. An appointment will be sent to you for removal of the catheter (called a trial without catheter) as an outpatient.
My urine is bloodstained / discoloured, is this normal?
There will be some bleeding from inside, and your urine will be discoloured and bloodstained after your operation. The bleeding settles down after two or three days, but often you will continue to see a small amount of bleeding for a few weeks after your operation.
We will be able to flush saline into your bladder through the catheter; in some cases bladder irrigation is also used if there are any blood clots. Sometimes blood passes out the end of the penis and the end of the catheter; this can look quite messy.
Please clean around the catheter when carrying out your normal hygiene routine. Please ask nursing staff for help with this if needed.
How will I feel after my operation?
The operation is not normally painful, but you may feel some discomfort and ‘soreness’. This will be controlled by painkillers given to you by the nursing staff. The catheter is often irritating and until it is removed can make you feel like you need to pass urine.
Can I eat and drink normally after my operation?
Please increase the amount you drink by up to two litres per day for the first week you are at home.
Eat normally, including all food groups.
Make sure you do not get constipated by increasing the fibre in your diet or taking a regular laxative if needed.
What should I do if I have bleeding when I return home?
Most men have no problem and are delighted with the outcome.
Bleeding is not uncommon at about 10 days after the operation, when the scab comes away. You need not worry, just increase the amount you drink. If the bleeding is very heavy or it becomes difficult to pass urine, please contact the ward for advice or go to the Urology Urgent Treatment Centre.
What should I do if I get a urine infection at home?
Urine infections can sometimes happen. You may feel burning when you pass urine, bleed, or need to pass urine more often. If this happens, please contact the ward or your GP for advice.
Why is it taking so long for my symptoms to resolve?
Although most men return to near normal within six weeks of their operation, in a few men it takes a number of months for all symptoms to resolve completely. The need to get up at night to pass urine often continues to some extent.
When can I resume normal activities?
Do not carry or lift heavy items for at least four to six weeks, for example suitcases, vacuum cleaners, lawn-mowers, or shopping. Although you have no visible scar, you have had a large operation and need to take things gently. Go for regular walks. Avoid vigorous activity until you have been seen in the outpatients department; about six weeks after your operation.
Will I need a follow-up appointment?
You will be seen in outpatients between six weeks and three months after your operation. Your appointment will be sent to you by post.
When can I start driving again?
Do not drive for at least two weeks after your operation or until you feel comfortable. Legally in an emergency you can drive 48 hours after your operation. Please speak to your insurance company for advice.
When can I have sex again?
You may have sex again two weeks after your operation or when you feel comfortable. We advise all patient to avoid sexual activity completely for two weeks.
It is not uncommon for men not to feel like sex for a while after their operation. This is nothing to worry about and should return to normal when you have recovered. This operation should not affect the feel and strength of an orgasm. It may however alter your ability to father children.
There is a small reported risk of impotence after this operation (five to 10 in every 100 patients). If you have had a problem before, this operation will not improve it.
What is retrograde ejaculation?
This happens in nearly all men after a TURP operation. This is when the sperm in your ejaculate passes back into your bladder, rather than coming out down your penis when you ejaculate. It then passes out from your bladder next time you pass urine.
Are there any complications / risks to this operation?
Discomfort or burning passing urine is common straight after the operation but wears off quickly.
Bleeding is common and may need you to come back to hospital for a bladder washout (five in every 100 patients) or a blood transfusion (one to two in every 100 patients).
Urine infection - particularly if a catheter has been needed before your operation. Significant infection (sepsis) is rare.
Bothersome urinary symptoms can continue after surgery in 10 to 20 in every 100 men.
Incontinence of urine may be experienced to start with but is very rare long term (one in 100 men will have this).
Lack of semen production. Semen may either pass back into the bladder harmlessly and be washed out in the urine, or not be produced at all. This can lead to an inability to father children but the operation cannot be relied upon to make you sterile.
About five in every 100 men will develop new problems getting an erection after their operation.
Scarring in the water pipe (urethral stricture formation) happens in around five in every 100 men.
Regrowth can happen. About one in five patients need a repeat operation by 10 years.
Medical problems such as absorption of irrigation fluid into the circulation or anaesthetic problems needing more medical care. These problems are very rare.
Latex allergy (some catheters are made from latex). Please tell your nurse or doctor if you have a latex allergy.
What if I feel unwell or have questions when I return home?
If you feel unwell or are in pain when you return home after your operation, please contact your GP.
If you bleed a lot or have trouble passing urine, go to the Urgent Treatment Centre at Kent and Canterbury Hospital.
You can contact Clarke Ward on 01227 78 31 03 for advice (24 hours a day).
If you have any questions about your treatment, please speak to the healthcare professional responsible for your care.