Portacaths
Information for patients having a portacath inserted
This leaflet is not meant to replace the information discussed between you and your doctor, but can act as a starting point for such a discussion or as a useful reminder of the key points.
What is a portacath?
A portacath is a combination of a capsule (portal) and a tube (catheter).
The capsule is normally placed under the skin of the chest wall and below the collar bone.
The tube runs under the skin and enters into a vein in the neck, before passing down the vein. The end of the tube lies near to the entrance of the heart. Access to this tube is through the capsule. The capsule is about the diameter of a 10p piece, but much thicker.
-
A portacath
-
 Portacath implanted under the skin of the chest wall
Portacath implanted under the skin of the chest wall
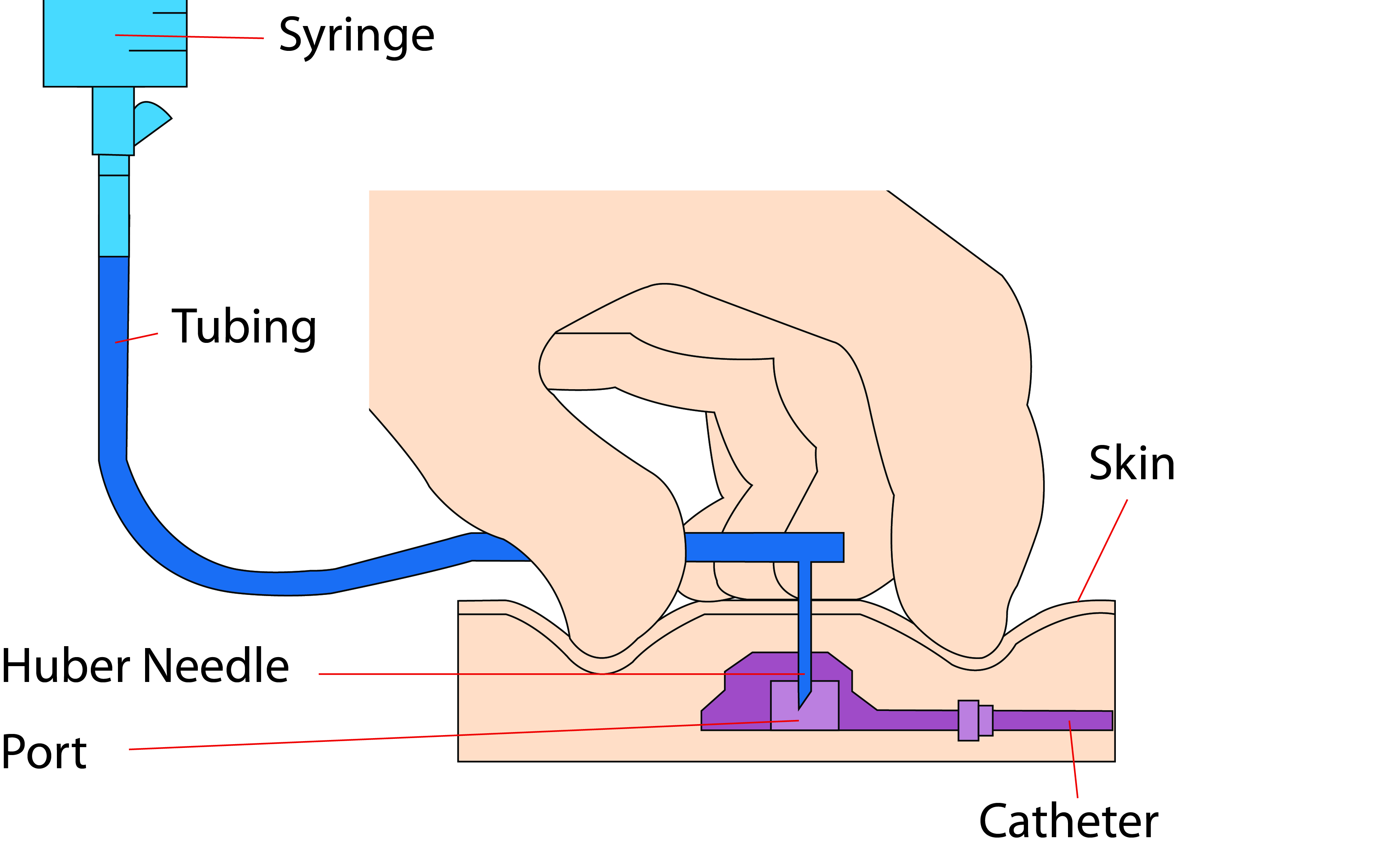
A special Huber (also known as a gripper) needle can be passed through the skin into the centre of the capsule, through a self-sealing silicone septum. Although the capsule is under the skin it does form a small bump. We need to be able to feel the capsule, so that a needle can be placed into it when you have your therapy.
What are the benefits of a portacath?
Portacaths can be used for taking blood samples and giving drugs, blood products, and intravenous (IV) feed. They are ideal for therapies that are given only every few weeks but over a long period of time. Portacaths can give consistent intravenous access for at least a year.
Patients can still swim if they have a portacath inserted.
How is a portacath inserted? Will it hurt?
A portacath has to be inserted in an aseptic manner to reduce the risk of infection.
The procedure is done in theatre, using both ultrasound and x-ray. We usually use a combination of local anaesthetic (the area is numbed) and sedation. We need to place a small cannula in your vein to give you the sedation. Patients are not normally completely asleep but it is unusual to remember much of the procedure. The most uncomfortable part of the process is usually when the local anaesthetic is injected into your neck and chest wall. This can sting for a few moments until the local anaesthetic starts to work.
During your procedure a small incision (cut) will be made in your neck and a second incision of three to five centimetres in your chest wall. The portacath is flushed with saline near the end of your procedure.
How long will I have to stay in hospital?
You can go home once you are fully awake. However it is important that you do not drive or sign any documents for at least 24 hours, as the sedation takes time to completely clear.
What aftercare is needed?
We usually use absorbable sutures for the chest incisions, so it is not normally necessary for the stitches to be removed. We also close the wounds with steri-strips, which should be kept in place for at least seven days. The stitches can take many weeks to break down completely. If after a week you can still see any of the suture material and it is causing you irritation, it can be removed.
You will also have a small incision in your neck where the tube enters into the vein. This is normally closed with steri-strips, although we may use an absorbable suture as well. Again the steri-strips should not be removed for seven days.
Sometimes your neck can feel a little sore and tight after your procedure. This is usually due to a combination of the dressing and some swelling. This should settle down in a few days.
The areas around the incisions should be kept clean and dry for at least a week after your procedure.
Your portacath needs to be flushed after every use. If it is not being used it should be flushed with 10ml of normal saline every four weeks to reduce the risk of the tubing becoming blocked with a blood clot.
What are the risks of having a portacath inserted?
Most patients have some bleeding and bruising of their neck and chest. This can look worse on the second and third day but normally resolves completely. A simple painkiller (such as paracetamol) may be helpful for the first few days after your procedure.
Infection is a significant risk, but less likely than if a normal intravenous catheter is used, as no part of a portacath is outside of the body.
As part of the procedure involves inserting a needle near the top of your lung, there is a very slight risk of puncturing the lung (a pneumothorax). In the very unlikely event of this happening, we may need to insert a small drain into your chest and admit you to hospital as an inpatient.
There is a small possibility that we may not be able to place the portacath, though this is less likely if you have not had any long-term catheters or chemotherapy before.
There is also a small chance that you may react to the drugs or dressings that we use during your procedure.
Very rarely, your chest or neck wound can open up or become infected.
To start with your wounds may not look good, but long-term severe scarring is not common.
What are the possible long-term problems with a portacath?
Over time portacaths can become blocked, either with a clot within the tubing or by a fibrin sheath, which can form over the end of the tubing. A fibrin sheath is a membrane of clotting factors. It sometimes acts as a one-way valve allowing drugs to be injected in, but not allowing blood samples to be drawn out.
Sometimes the capsule can start to turn on its side or completely turn over (rather than remaining flat on your chest wall). This makes accessing the line more difficult.
If you lose a lot of weight the capsule may start to erode through your skin. Or if there is significant weight gain, then the capsule may become difficult to feel or access with the Huber (gripper) needle.
Very occasionally the tube may rupture at some point along its length. This may result in pain when chemotherapy is given, as it will diffuse into your tissues. If this happens the chemotherapy should be stopped immediately.
When will my portacath be removed?
Your portacath can be removed when treatment is no longer needed. Please discuss this with your consultant.
How is my portacath removed?
Removing a portacath is normally much simpler than inserting it. This is usually done using just local anaesthetic, but it can be combined with sedation if needed. An incision is made close to the original chest wall entry site. The capsule is freed up and pulled out along with the tubing. The wound is closed with absorbable sutures and steri-strips.
What if I have any questions or concerns about my portacath?
If you have any concerns about your portacath, please contact the IV Access Nurse Specialist on 07786 976304, Monday to Friday 8am to 4pm.
.JPG)