Platelet Rich Plasma (PRP) injection
Information for patients from Trauma and Orthopaedics (T&O)
This leaflet is for patients suitable to be treated with Platelet Rich Plasma (PRP) injections. These injections are used to treat various conditions that cause pain to some soft tissue of the body like the shoulder or the elbow. The treatment with PRP may improve your condition. This leaflet explains what PRP injections are and will also provide you with the information about what you need to do through the process.
Contents page
What is Platelet Rich Plasma (PRP)?
How does PRP therapy work?
How long will the procedure take?
What are the potential benefits of this treatment?
What are the possible risks or complications of this procedure?
How will I feel after my injection?
How do I care for my dressing at home?
Can I have a bath or shower?
Can I drive myself home after my injection?
When can I drive again?
When can I start my usual activities, including exercise?
PRP injections and athletes
When can I return to work?
Will I have a follow-up appointment?
What should I do if I have any concerns or questions?
Contact details
What is Platelet Rich Plasma (PRP)?
Platelets are found in your blood and contain granules which help you to heal after an injury.
Platelet rich plasma is blood plasma which contains more platelets and therefore, more healing factors. The healing factors are an important tool to help with tissue repair, development of new blood vessels, and wound healing.
How does PRP therapy work?
A small amount of blood, similar to a blood test, will be taken from you at the hospital and placed in a machine that spins at high speed to separate the different types of blood cells.
Your surgeon will take out the platelet rich part of the blood (PRP), mix it with local anaesthetic, and inject it into the area of your injury (shoulder or elbow).
Local anaesthetic (marcaine or chirocaine) is used to help with your symptoms and reduce your pain.
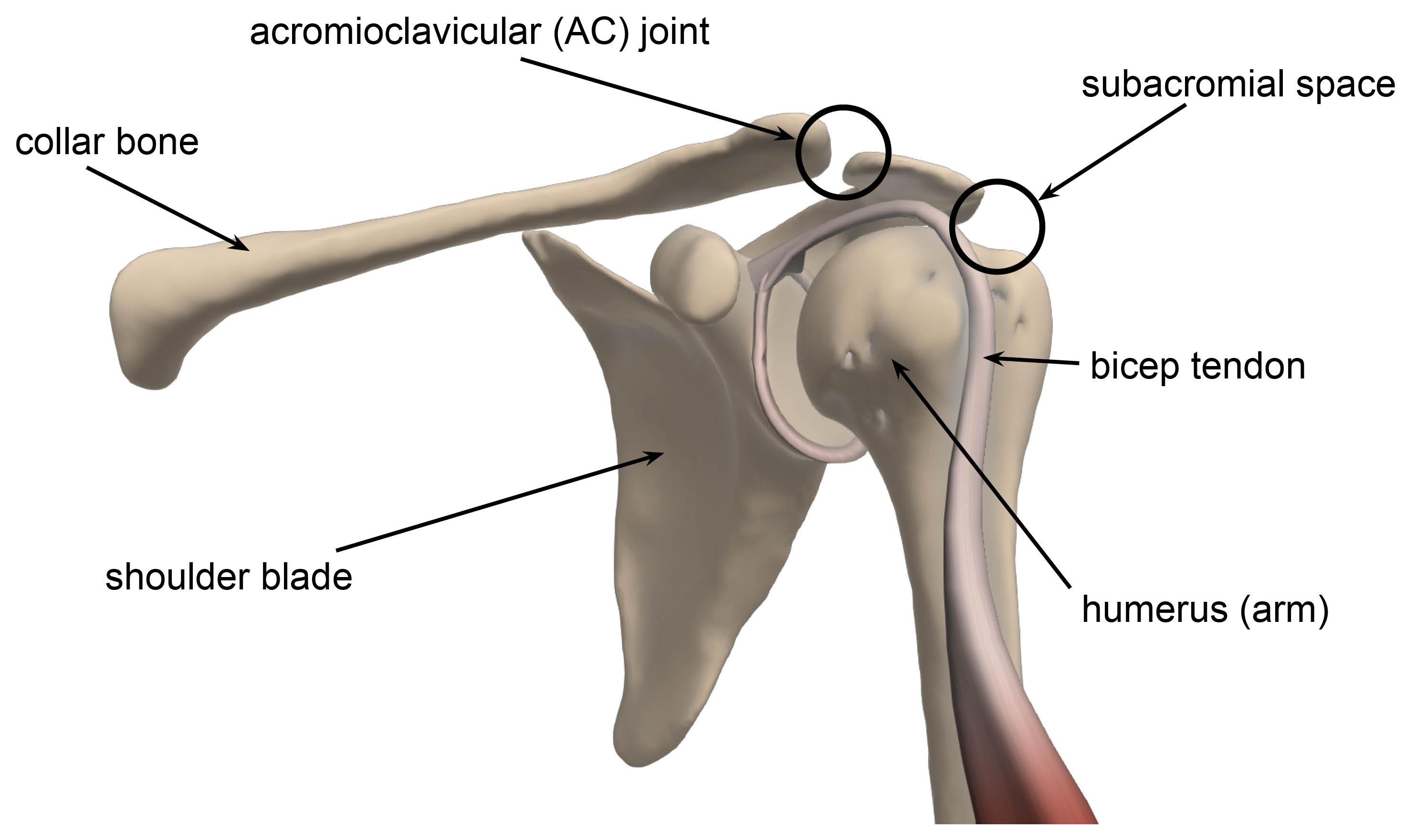
We will find the painful areas in your elbow or shoulder and inject you in that place. In the shoulder the painful area is usually the joint between the shoulder blade and the collar bone (AC joint) at the top of your shoulder, or the area between the arm bone and the shoulder blade (subacromial space). Sometimes your biceps tendon may also need an injection.
If you have pain in your elbow, the medial or the lateral side (epicondyle) of your elbow will be injected. Which side is injected depends on where your elbow pain arises.
According to the published literature, this procedure can satisfactorily increase the number of platelets and growth factors at the site of injury (Source: Mariani E, Pulsatelli L. Platelet Concentrates in Musculoskeletal Medicine. Int J Mol Sci. 2020 Feb 16;21(4):1328).
How long will the procedure take?
The procedure usually takes around 30 minutes. Most of this time is spent separating the PRP from your blood sample, which takes about 15 minutes.
This procedure is done while the patient is awake.
What are the potential benefits of this treatment?
The main benefit is that patients could see an improvement in symptoms.
This treatment may also mean that other treatments such as long-term medication or surgery, are no longer needed.
A major advantage of this treatment is that no foreign substance is used, we use the patient’s own blood. So there is no risk of any disease transmission, allergic reaction, or rejection.
We believe that PRP might help with your recovery, but although there is no clear scientific evidence yet, there are some case studies that show improvement in symptoms.
What are the possible risks or complications of this procedure?
As with all invasive procedures there are some risks to having this injection.
Infection at the site of the injection. We do everything we can to avoid this, but an infection might still happen. If where you were injected becomes increasingly red or swollen after your injection, please contact your GP or your surgical team for advice as soon as possible.
An increase in pain and inflammation (swelling and redness) at the site of the injection for five to seven days.
Bleeding and / or bruising at the injection site or where the blood was collected from.
Temporary changes in skin colour, around the site of the injection.
Continued pain and Chronic Regional Pain Syndrome (CRPS). This is a condition where a person experiences persistent, severe, and debilitating pain. Although most cases of CRPS are triggered by an injury, the resulting pain is much more severe and long-lasting than normal.
The procedure may not be successful and may need further treatment in the future, if after couple of weeks your initial symptoms continue.
How will I feel after my injection?
A local anaesthetic is used during the procedure, which means that immediately after your procedure your shoulder or elbow may feel numb and pain-free. This may last a few hours. After this the area may well be sore for 24 to 48 hours. You can take simple painkillers (such as paracetamol), following the dosage instructions on the packaging.
We recommend that you try to avoid anti-inflammatory medications (such as ibuprofen) for up to a week before and for up to four weeks after your procedure. If you are unsure whether any regular medication you are on is anti-inflammatory, show it to your doctor or nurse so that they can advise you whether it is safe to take.
How do I care for my dressing at home?
After your treatment, a dressing will be covering your wound. Avoid getting it wet for the first seven days.
If your dressing gets wet or bloodstained, you can change it yourself by carefully placing a dressing from a pharmacy. If you are unable or have difficulties doing that yourself, you can ask a relative or a friend to change it for you.
Can I have a bath or shower?
You should have a ‘dry wash’ or a shallow bath instead of a shower for the first week following your injection, to avoid getting your dressing wet.
Can I drive myself home after my injection?
We advise you to come to your appointment with a friend or relative, who can drive you back home or you can arrange hospital transport.
When can I drive again?
You may start driving again when you feel comfortable, usually within one week after your procedure. The advice from the DVLA is that you should not drive until you are physically capable of controlling a motor vehicle and can perform an emergency manoeuvre safely and confidently.
When can I start my usual activities, including exercise?
Do as little as possible for the first three days after your procedure. You can start returning to your normal activities as needed, as long as they do not need you to lift anything heavy.
PRP injections and athletes
Please note that PRP injections are normally not banned for any athlete that is subject to testing under WADA (World Anti-Doping Agency), but please verify this with your team and your sport’s governing body.
When can I return to work?
You may return to work as soon as you feel able, this is usually a few days after your procedure. If your job involves manual work, stay off work for about a week.
If you need a sickness certificate for your employer, please ask your doctor before you leave hospital. If you need certificates in the future, please speak to your GP.
Will I have a follow-up appointment?
You will receive a follow-up appointment six weeks after your procedure. At this appointment you will be reviewed by the physiotherapist, surgical care practitioner, or surgeon who will check your progress. They will make sure you are moving your elbow and shoulder and give you further exercises, as appropriate.
What should I do if I have any concerns or questions?
If you have any questions or concerns, please contact your surgical care practitioner, surgeon, or physiotherapist. Their contact details are listed on the last page of this leaflet.
If you notice your wound area is becoming more painful, red, hot, and / or discharging pus (thick yellow discharge), you may be developing an infection. Contact your GP or your surgical team for advice as soon as possible.
Contact details
Consultants and their secretaries
The teams listed below work at Kent and Canterbury Hospital as well.
| Hospital site | Consultant | Secretary name | Contact number |
|---|---|---|---|
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Mr Sathya Murthy | Tracy Blackman | 01843 235068 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Mr Georgios Arealis | Donna Cannon | 01843 235083 |
| William Harvey Hospital, Ashford | Mr Paola Consigliere | Heather Littlejohn | 01233 616280 |
| William Harvey Hospital, Ashford | Mr Jai Relwani | Dione Allen | 01233 616737 |
| William Harvey Hospital, Ashford | Surgical Care Practitioner | Patricia Velazquez-Ruta | 07929 375381 |
Physiotherapists
| Hospital site | Physiotherapist | Contact number |
|---|---|---|
| Buckland Hospital, Dover | Abi Lipinski | 01304 222659 |
| Kent and Canterbury Hospital, Canterbury | Sarah Gillett (inpatient) | 01227 866365 |
| Kent and Canterbury Hospital, Canterbury | Darren Base | 01227 783065 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Caroline Phillpott (inpatient) | 01843 234575 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Martin Creasey | 01843 235096 |
| Royal Victoria Hospital, Folkestone | Alisa Sutherland | 01303 854410 |
| William Harvey Hospital, Ashford | Cindy Gabett (inpatient) | 01233 633331 |
| William Harvey Hospital, Ashford | Chris Watts | 01233 616085 |
Surgical Preassessment Units
| Hospital site | Contact number |
|---|---|
| Kent and Canterbury Hospital, Canterbury | 01227 783114 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | 01843 235115 |
| William Harvey Hospital, Ashford | 01233 616743 |
Fracture Clinics
| Hospital site | Contact number |
|---|---|
| Kent and Canterbury Hospital, Canterbury | 01227 783075 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | 01843 235056 |
| William Harvey Hospital, Ashford | 01233 616849 |