Phacoemulsification and intraocular lens for narrow or closed angles
Information for patients from Ophthalmology
You have been given this leaflet as you have been diagnosed with narrow or closed angles in your eyes that need surgery.
What are narrow or closed angles?
Narrow or closed angles means the area between the periphery (edge) of the iris and the cornea is too narrow (see diagram below). This can lead to angle closure glaucoma, affecting the optic nerve, which carries images from the retina to the brain.
In some cases, the normal fluid pressure within the eye (known as intraocular pressure or IOP) is too high, putting pressure on these nerve fibres. Untreated this may lead to permanent loss of vision (eyesight).
What can cause the eye pressure to increase?
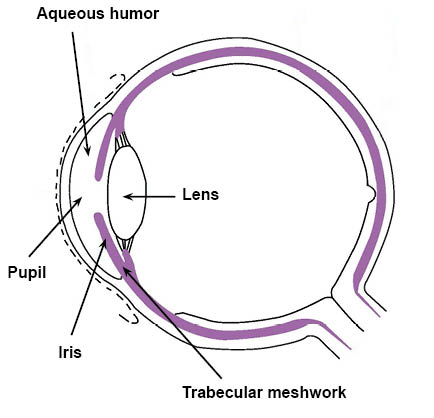
The fluid within your eye (aqueous humor) helps to bathe and nourish the lens, iris, and cornea. It is produced by the tissues around the lens, and drains out of your eye through a meshwork of tissues called the trabecular meshwork, found at the outer edge of your iris.
The fluid then drains into your bloodstream. The drainage angle (the area where the edges of the cornea and iris meet) in people with narrow or closed angles is too shallow, meaning that the fluid may not drain away as effectively.
When your pupils get bigger, for example in dark conditions, the pressure in your eye can rise leading to an episode of acute glaucoma.
What is phacoemulsification and intraocular lens?
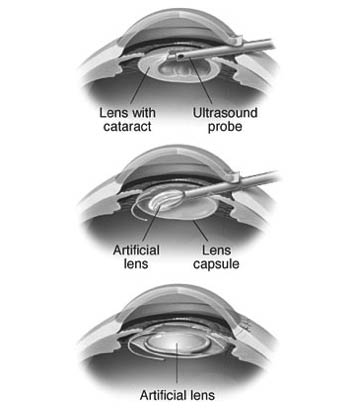
This is an operation on the eye to remove the contents of the natural eye lens, and insert a new artificial lens into the lens membrane.
It is often performed to treat cataracts (clouding of the natural eye lens).
Why has it been recommended for me?
There are three main reasons that this procedure is recommended.
To treat an attack of acute glaucoma.
To prevent an acute attack of glaucoma.
To treat chronic narrow angle glaucoma, where the drainage channel is very narrow.
How does the operation help?
The natural eye lens gets thicker with age, which can make less space for the fluid in the front of your eye to drain away. Having this operation creates more space for the fluid to drain, which usually prevents acute glaucoma attacks.
Will the operation affect my vision?
The operation may affect your vision, for example you may notice improved vision if there is some clouding of the natural eye lens (cataract).
You may not see as well after your operation, for example if there are any complications. The aim of this operation is not to improve your sight, but to reduce the risk of you having an acute attack of glaucoma, which puts you at higher risk of losing your sight.
Your eyesight may stay the same.
Are there any risks?
Yes, every operation carries some risk; however the risk of this operation may be less than not having it done. Every care is taken to avoid complications, but even in the best of hands, complications can happen. All means available will be used to minimise the effects of any complications.
There is a small risk of developing a serious eye infection after surgery; this is rare.
If the bag that holds the lens in place tears, the lens may not be inserted into your eye until a later date.
Bleeding inside your eye is possible and can affect your vision temporarily or permanently.
Some time later your vision may become hazy due to clouding of your natural lens membrane. This is usually helped with a laser procedure in Outpatients.
There is a small risk of a detached retina in the first few weeks following surgery.
There is a risk of some swelling of your retina called cystoid macula odema, which may need treatment with eye drops and take time to settle down.
There is a risk of reduced vision or eye pressure not reduced enough, which may need further medication or surgery.
There is a higher risk of complications from this type of surgery than with a standard cataract operation, due to the narrow angles of your eyes.
If an acute angle closure attack happens, then you will need emergency phacoemulsification surgery. This carries significantly higher risk of complications and visual loss.
What will happen before my surgery?
You will need to have eye measurements taken (biometry) in an eye clinic, and may need a preassessment (general health check) in clinic or over the telephone.
Please check your appointment letter for special instructions. f you wear contact lenses, please leave them out for 24 to 48 hours if they are soft, and one to two weeks if they are hard lenses.
If you are using pilocarpine eye drops, please stop them three days before your operation. Your ophthalmologist may prescribe some Diamox tablets just before your operation to control your eye pressure.
Why do I need to clean my eyes before surgery?
We ask all patients to clean their eyelids before their eye procedure / surgery. This is to prevent any problems at the time of your operation, as infection could be transferred from your eyelids into your eye. This does not guarantee that you will not get an infection, but it will minimise the risks.
Who will carry out my operation?
Whilst you will be in the care of a named consultant for your treatment, it does not mean that this is the person that will carry out your operation. All of our doctors work in teams, and it may be another member of that team who carries out your surgery.
What will happen on the day of my operation?
Unless you are having a general anaesthetic we do not usually ask you to change into a theatre gown. Please wear something that is comfortable and easily removed when you get home (button fronted garments are good), as you may be wearing an eye patch after your operation and do not want to be struggling to get clothing over your head. Please bring a book, magazine, or something to occupy you.
Do not wear contact lenses on the day of your surgery, hard or soft. Glasses should be worn where necessary.
Can I eat and drink before my operation?
Unless we have told you otherwise, you may eat and drink normally before your procedure.
Should I take my normal medication before my operation?
Do not stop any medications, including painkillers or eye drops, unless you have been told to by your doctor or preassessment nurse. If you need to take medication during your stay, please bring them with you to hospital.
If you are on insulin or any other diabetic medication, or if you have a GTN spray or inhalers, please make sure that you bring these with you and tell the nurse when you arrive.
What will happen when I arrive at the hospital?
On arrival, please report to the receptionist. A nurse will take your blood pressure and pulse and ask you a series of questions. Please bring the contact number of a relative / friend in case we need to contact somebody in an emergency.
You will be in hospital for approximately four hours. Just before your operation, you will be given eye drops to enlarge your pupil.
The doctor will also see you before your procedure and answer any further questions that you may have.
Phacoemulsification surgery using ultrasound
Normally phacoemulsification surgery is carried out under local anaesthetic (you are awake but the area will be numbed). This is given using either anaesthetic drops or an injection around the area of your eye. However, your ophthalmologist may decide that you need a general anaesthetic (you will be asleep). This will have been discussed with you already in the clinic.
The operation is performed using a microscope and generally takes up to 35 minutes. Normally a small incision (cut) is made in the eye; this incision is designed to self-seal and rarely needs stitches. If a larger incision is needed, you may need stitches.
A pad or shield will be put over your eye to protect it from accidental rubbing and bumping.
A nurse will be with you throughout and you will have some food and drink afterwards.
Before you are discharged home, a nurse will give you all the instructions and advice that you need; this will be in the presence of any relative or friend you bring with you and who will take you home. Please ask any questions and share any concerns that you have.
How can I expect my eye to feel after surgery?
The following are common symptoms and are not to be concerned about.
A feeling of something in your eye / watery eye is usually your eye healing. Some swelling occurs and you can try artificial tears from a chemist to soothe your eye if you like.
Mild discomfort can be helped with your usual painkilling medicine (such as paracetamol).
Light may seem bright, so wearing sunglasses at first can help.
Colours look brighter; this is normal.
Red or bloodshot eye; this usually settles within one to two weeks.
Some swelling and / or bruising in and around your eye: this usually settles within one to two weeks.
Small floaters or double vision; this usually settles down.
Seeing something at the outer edge or a line across your vision, especially when near a window. This should settle as your brain gets used to the new lens.
Blurred distance vision. This can happen straightaway or one to two days after surgery. You can try having the distance vision lens removed from your glasses on the operated side, and give your eye some time to settle down. If your vision is worse than before your operation, please contact us.
Blurred reading vision. The surgeon usually replaces your cloudy lens contents with a new clear artificial single focus lens. It is often clearer for the distance vision than for reading. You can try ready readers (available from chemists, supermarkets, or petrol stations) to help you to read, while you are waiting four to six weeks to see your optician.
When should I ask for help?
These early symptoms should gradually settle down as the days and weeks go by. If you have any of the following or you are worried about your eye, please call the on-call nurse.
Vision getting worse
Severe pain in your eye
Yellow or green discharge from your eye
Straight lines (such as door frames) looking wavy / distorted
Swelling of your eyelids or feeling excessive itching
Bright lights hurt your eye
Feeling nauseous (sick) or having a feeling of “seasickness”
New large floaters in your eye
Flashing lights
Black or grey curtain appearance across your eye.
How do I use the eye drops / ointment?
Read the label for the directions.
Wash your hands.
Sit or lie comfortably with your head tilted backwards looking at the ceiling.
Gently pull down your lower lid with one finger to form a sac.
Holding the eye drops / ointment in your other hand, bring the dropper close to your eye and squeeze one drop into the sac. Do not let the dropper touch your eye or eyelid. If you are using ointment, use about a quarter of an inch on the inner surface of the lower lid of your eye.
-
 Using eye ointment
Using eye ointment -
 Using eye drops
Using eye drops
Close your eye and blot excess solution with a clean tissue.
Replace the cap of the eye drops / ointment immediately after use.
You may find it easier to get someone else to help you.
Use only for the eye mentioned on the label, unless told otherwise.
Discard the bottle / tube once treatment is completed, or use a fresh bottle every four weeks.
Get more from your GP before you run out if you do not have enough.
It is important to use the eye drops for the whole month, to settle your eye and prevent infection. If you need to, you can buy a plastic device to help with using the eye drops from a chemist, Glaucoma UK, or the Kent Association for the Blind.
Can I still use my other eye drops?
Yes, please continue using all your usual eye drops, such as artificial tears or glaucoma medicines. Use a fresh bottle for your operated eye and a separate bottle for your other eye for the first month after surgery.
Please leave a gap of three to five minutes between different eye drop medicines.
Can I clean my eye?
You can gently clean your eye (after washing your hands) using some boiled cooled water, made fresh every time, with some cotton wool pads. Please do not use a flannel or handkerchief on your eye for the first month to reduce the risk of infection.
What can I do for the first week after surgery?
You can do your normal activities such as reading, watching television, going out, and light housework.
Please avoid lifting anything heavy.
Do not lean forward to wash your hair, lean backwards instead, keeping soap and tap water away from your eye.
Use your eye drops as instructed and avoid rubbing your eye.
If you wear glasses, place your thumbs over the ends of the frame when putting them on, to avoid any chance of poking your eye.
What can I do two to four weeks after surgery?
Continue to use your eye drops. You can wash your hair normally again. Gradually get back to your usual routine, and return to activities such as gardening, golf, bowling, and cycling with care, if you wish.
When can I swim or use eye make-up?
You can swim and use eye make-up again when you have finished your eye drops, four weeks after your surgery. This is to reduce the risk of getting an infection in your eye.
When can I drive?
You can drive a car or a mobility scooter when you feel safe to do so and are meeting the DVLA standard as follows:
People driving a Group 1 car / motorcycle, in good light (with the aid of glasses or contact lenses if worn) should be able to read a vehicle registration number plate:
plate registration before 1st September 2001 at a distance of 20.5 metres
plate registration after 1st September 2001 at a distance of 20 metres.
People driving must also meet the recommended national guidelines for visual field.
Often this can be a four to five days or more after surgery. It may help to have the lens removed from the operated side of your driving glasses, as the old lens may make your vision seem more blurry. If in doubt, speak to your optician.
Will I still need my glasses?
The best vision is often not achieved until both eyes have had surgery. In a very few cases, it may be necessary to cover one eye for certain activities until the second eye has been operated on.
Your glasses may no longer be useful after phacoemulsification surgery. Unfortunately, there are no rules to say what will give you the best vision. Here are a few suggestions.
If you can see better without your spectacles, then do not wear them.
If your glasses still work well, then you can continue to use them.
For most patients you will need glasses only for the eye that has not had surgery. If it is possible, you may ask somebody to remove the glasses lens from the eye that has had the surgery.
If you have some old glasses at home you may wish to try them.
Will I need to see my optician?
Yes, please make an appointment to see your optician about four to six weeks after surgery, when your eye has settled down. Please take the paperwork the hospital staff gave you to show the optician.
What about my other eye?
If you have a cataract on your other eye, you can discuss it with your optician who will send a report back to the surgeon. You may then be placed on the waiting list for your second eye cataract surgery; we do not usually need to see you at the hospital again before your second operation unless there is a problem. There are usually a few months between the two operations, as the first eye needs to settle down and be measured by your optician before a decision is made about your other eye.
When can I go back to work?
You can usually return to work after about one week, depending on what work you do. Office / computer work can be resumed as soon as you feel able.
Can I travel after surgery?
Yes, it is fine to travel after your surgery, this includes flying. Please make sure you have enough eye drops to use for the whole month.
Avoid swimming for one month, and consider travel insurance / how to get medical help for foreign travel.
What if I have concerns or questions once I am home?
Please remember that most patients have a very good result from their surgery. If you develop any problems after your operation, please contact the hospital on one of the following numbers.
Kent and Canterbury Hospital, Canterbury
Waiting List Co-ordinator Telephone: 01227 866444
Ophthalmology Suite Telephone: 01227 866493
Queen Elizabeth the Queen Mother Hospital, Margate
Waiting List Co-ordinator Telephone: 01843 234364
Day Surgery Telephone: 01843 234458
William Harvey Hospital, Ashford
Waiting List Co-ordinator Telephone: 01233 616757
Channel Day Surgery Centre Telephone: 01233 616263
We have tried to cover most of the more common problems that can happen after phacoemulsification surgery. However, it is not possible to cover them all. Please remember that all eyes are different and your experience of phacoemulsification surgery may not be the same as other peoples.
If we are operating on both eyes it is possible that the experience will be different on the two occasions.