Oxygen on discharge from hospital
A guide for patients and their carers from the Respiratory Practitioner Team
Why have I been given oxygen therapy to go home with?
Whilst you have been in hospital, your blood oxygen levels have been low, and you have needed oxygen therapy. You have been assessed and it has been decided that you are suitable to go home with a temporary or a permanent supply of oxygen. This leaflet explains how this oxygen works, how to use it safely, and what happens next.
There are many conditions which may cause your oxygen levels to be low. These include long-term respiratory conditions (including chronic obstructive pulmonary disease (COPD) and interstitial lung disease), palliative care, pulmonary hypertension, and ongoing recovery from an acute illness.
How does oxygen therapy help?
Oxygen therapy increases the amount of oxygen in your lungs and bloodstream, taking the strain off your heart. It can improve how you perform daily activities such as walking, and also improve your concentration and sleep. Sometimes you may not feel a noticeable benefit from using the oxygen, but there are long-term benefits from oxygen therapy.
Will oxygen therapy help with breathlessness?
Oxygen is a treatment for persistent low blood oxygen levels, not breathlessness alone. Breathlessness can be relieved in a number of ways which include: medications (inhalers and low doses of morphine), fan therapy, and breathing techniques. These are likely to be much more helpful than oxygen. Please ask your respiratory practitioner or physiotherapist for more information.
How do I use the oxygen therapy?
There are several different types of home oxygen therapy:
Long-term oxygen therapy (LTOT) is used to stabilise oxygen levels for 15 hours or more.
Ambulatory oxygen therapy (AOT) is used to help you be more active. It can also be called portable oxygen.
Palliative oxygen therapy (POT) is used to manage very low oxygen levels in patients with an irreversible life-limiting condition.
Before you leave hospital, a member of the Respiratory Team will explain what type of oxygen therapy you have been prescribed and how you should use the oxygen. Before you are discharged home, the local oxygen company (Dolby Vivisol) will deliver the oxygen equipment to your home and show you how to use it with a friend / carer / family member.
Your prescribed flow rate is: _________________________________________
You need to wear your oxygen for: ____________________________________
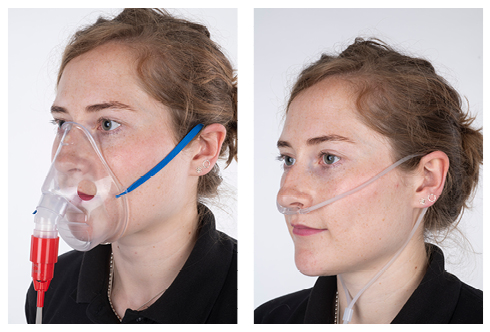
You may use a mask or nasal prongs.
If you use nasal prongs check each day to make sure the tips are not blocked. If needed, wipe tips with a damp cloth.
If your oxygen is delivered using a mask, then this also needs to be cleaned daily with a damp cloth.
The mask or nasal prongs should be changed once a month. The oxygen company will provide these.
If your nose becomes sore, use water-based lubricants such as KY Jelly or Aquagel. Do not use Vaseline or petroleum jelly, as this hardens the prongs and is a fire risk.
Do not increase the flow rate (unless told to do so by your respiratory practitioner or another member of the Respiratory Team); this is unsafe and may cause you to become unwell.
While using oxygen do not drink alcohol or take drugs that relax you (such as sleeping pills, sedatives, or recreational drugs), unless prescribed by your healthcare professional.
Oxygen is a medical gas and is prescribed like any other medication. It is regulated by the Healthcare Products Regulatory Agency.
If you have new symptoms of morning headaches or heaviness, disorientation or confusion, or increased tiredness or drowsiness, you must tell your Respiratory Team or GP immediately.
How do I use oxygen safely?
You must not smoke (including cigarettes, e-cigarettes, and vapes) whilst having oxygen therapy. Smoking around oxygen is a serious fire hazard and also reduces the benefits of oxygen therapy.
The One You Smoke Free service has friendly advisers who can help you to stop smoking; you are up to four times more likely to quit with support. You can contact them to access their free service on 0300 123 1220.
It is important that nobody else smokes in the room whilst you are receiving oxygen.
Stay at least three metres (approximately 10 feet) away from any gas appliances, lit fireplaces, open flames (including candles), and hair dryers or straighteners.
Your central heating is not a problem; continue to use it as you would normally.
Do not use oxygen therapy in the same room as paraffin or Calor Gas heaters.
If you use oxygen in your car, please switch off your oxygen before refuelling or arrange for somebody else to refuel for you.
Do not use flammable products such as aerosol sprays, oil based lubricants, grease, petroleum based products, or paint thinners near the oxygen supply or when using oxygen.
Do not use vapour rub or petroleum jelly (Vicks / Vaseline), but use water-based lubricants (such as KY Jelly or Aquagel).
Warn visitors of the dangers of tripping over tubing, and take care not to trip yourself. Make sure visitors take the same precautions as you, and are aware that you are using oxygen therapy.
Make sure tubing does not become kinked.
Make sure you have smoke alarms at home and test them regularly. If you do not have smoke alarms, then these should be fitted as soon as possible. Kent Fire and Rescue may be able to support you with this if you ring your local fire station.
Please keep pets / animals away from the tubing, as they may try to chew through the oxygen tubing.
What happens if I choose not to have oxygen therapy?
You are allowed to say “no” to having home oxygen therapy. However, we will want to discuss with you what this decision will mean for your health. You are also entitled to change your mind and ask for oxygen to be considered in the future. We would recommend you discuss this with your GP or the Respiratory Team once you are at home.
Will I become dependent on oxygen?
Oxygen therapy improves your oxygen levels, oxygen itself does not cause dependency.
Will I have to be treated with oxygen forever?
Every person is different, and it is impossible to tell if you will always need oxygen therapy. Before receiving oxygen in the long-term, you will be assessed by a Specialist Respiratory Team to monitor your need for oxygen. Blood tests will look at the amount of oxygen you have in your blood; this allows us to make appropriate changes to your home oxygen prescription, or remove your oxygen if it is no longer needed.
Can I have too much oxygen?
Yes. Oxygen is a prescribed drug that all patients must be carefully assessed for. All patients should be aware that oxygen can cause harm if used inappropriately. When not needed, oxygen can cause several short- and long-term side effects, including raised carbon dioxide levels in the bloodstream, loss of independence, and immobility. Not every person assessed will need home oxygen.
Can I travel with oxygen?
Yes. Plan in advance to make sure that your trip goes well. This can be discussed in more detail when you are reassessed in the community by the Community Respiratory Team / GP.
What happens next?
Your respiratory practitioner will tell you who will review your oxygen when you are at home. The main teams who provide ongoing care and support for people with home oxygen are the Community Respiratory Team, Palliative Care Team, your GP, and the Acute Response Team.
If you have been referred to the Community Respiratory Team and have had no contact within six weeks of your discharge from hospital, please phone 0300 123 1412 (normal working hours) (0300 numbers are charged at your normal standard call rate).
If you are under the care of the Palliative Team they can be contacted for ongoing support with your oxygen.
Community Hospice support
Telephone: 01233 504133.Vivisol (oxygen company)
Telephone: 0800 917 9840
What should I do if I feel unwell at home?
If you have any of the following symptoms, please call your GP / Community Respiratory Team as soon as possible.
Increasingly short of breath.
Restlessness or confusion.
Early morning headaches
You can leave a message, but if you are very unwell or need urgent advice outside of these times, please call 111 or 999.
With thanks to NHS BEN & HoEFT Project Team as part of the Department of Health Lung Improvement Project, for allowing us to use their leaflet in the development of this leaflet.