Overactive bladder
Information for patients from the Urogynaecology Department
An overactive bladder (OAB) is a very common problem. It can cause distressing symptoms that are difficult to control. These can include a frequent urge to go to the toilet, and can sometimes result in leakage before you reach the toilet. This leaflet is designed to explain what an overactive bladder is, and what causes it. It will also explain some of the treatments that can be done to help to improve these symptoms.
How does a normal bladder work?
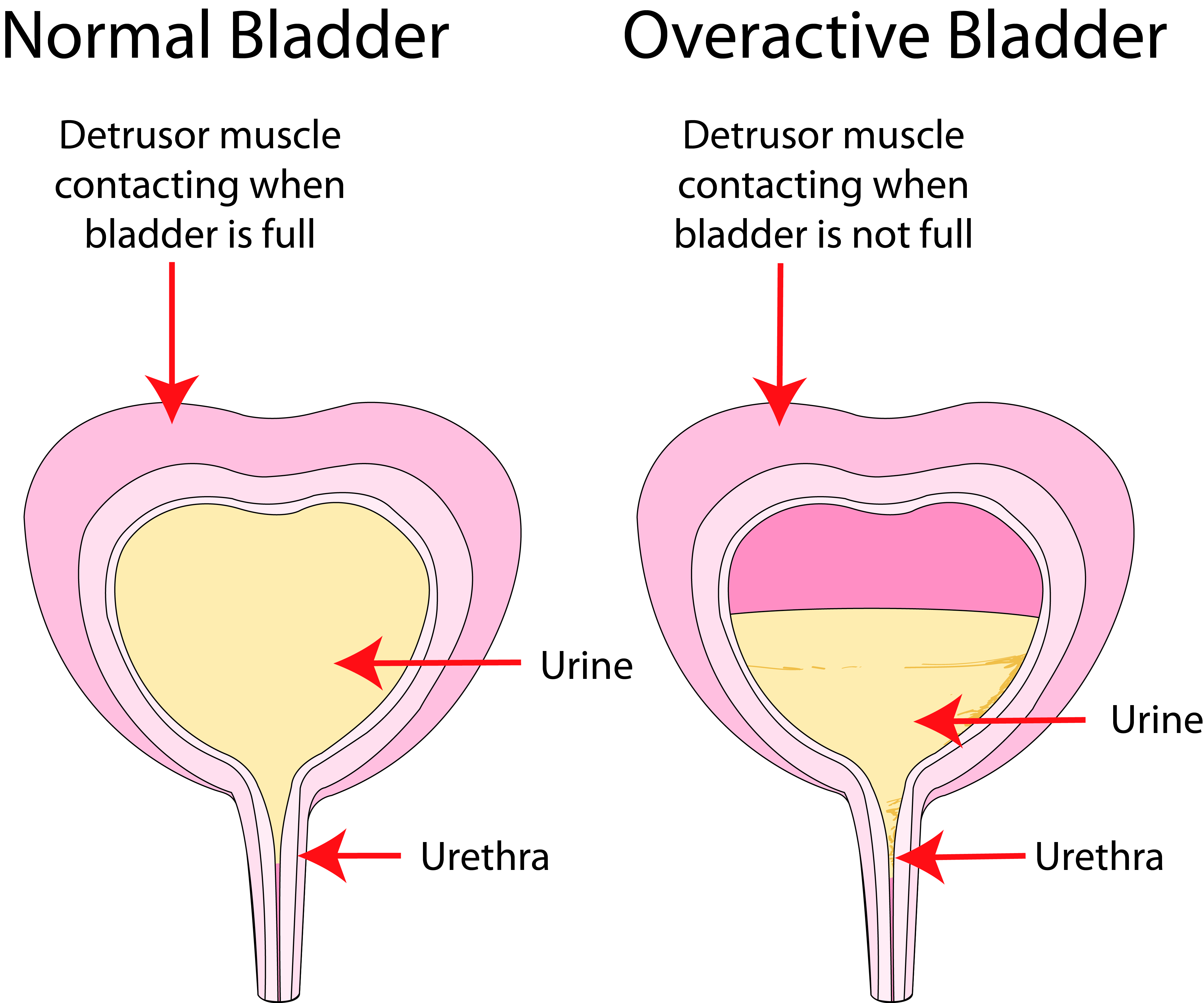
The bladder is similar to a balloon. As urine is produced and the bladder fills, the bladder walls stretch to deal with the extra fluid. Urine is kept inside the bladder by a “valve”, which is called the urinary sphincter. This valve is normally shut (except when you are emptying your bladder).
The pelvic muscles also help to keep urine in. They tense up when you exercise or cough, and help the valve to stay closed.
As your bladder fills up, you may feel an urge, but you are able to hold on. When you decide to empty your bladder (in the toilet), your brain sends a signal to the muscle of your bladder to squeeze and empty your bladder. At the same time, your valve and pelvic floor relax and allow the urine to flow out.
The bladder usually needs to be emptied between four to seven times a day and once at night.
What is an overactive bladder?
An overactive bladder can be caused by the bladder wall muscles squeezing out urine from the bladder at the wrong times. This often happens without warning, and when you do not want it to.
What are the symptoms of an overactive bladder?
It can cause the following symptoms.
Urgency is a sudden and intense need to pass urine that cannot be put off. This can happen even when your bladder is not full. Sometimes you may not make it to the toilet in time and may leak. This is called urge incontinence.
Frequency is going to the toilet too many times during the day (more than seven).
Nocturia is waking up more than once to go to the toilet.
What causes an overactive bladder?
OAB affects people of all ages, and is not simply a result of getting older.
Urinary infections can be a cause of OAB symptoms, and it is important that infection is ruled out at an early stage.
Bladder stones, growths, or inflammation in the bladder can also cause OAB symptoms.
If you have already had an operation for stress incontinence or other pelvic surgery, this can also irritate your bladder and cause these symptoms.
OAB can be caused by some neurological conditions, such as Multiple Sclerosis (MS).
The amount and type of fluids that you drink (for example caffeinated fluids like tea and coffee) are known to significantly worsen OAB symptoms.
How will I be tested for an overactive bladder?
When you are assessed by the doctor or nurse they will ask you questions about your bladder, fluid intake (how much you drink), and general health. A Urinalysis will also be checked. This is where your urine will be screened for infection or blood in your urine.
You may be examined to rule out any gynaecology problems that may be contributing to your problem. You may also be asked to fill in a fluid diary to chart your fluid intake (and type), and how much and how often you pass urine. This chart can provide valuable information on how to help improve your symptoms.
The following tests may also be suggested.
Residual urine. If your bladder is not emptying completely, this can be a cause of OAB symptoms. You may be asked to empty your bladder and the residual volume will be checked using an ultrasound machine, or possibly a small catheter.
Urodynamics is a series of tests that investigate causes of incontinence, and can sometimes diagnose if your bladder wall muscle is squeezing inappropriately.
What treatments are available?
Lifestyle changes
There are changes that you can make to your lifestyle that can really help improve your symptoms. Drinks containing caffeine (such as tea, coffee, and coke) can make OAB symptoms a lot worse. Fizzy fluids (including fizzy water), fruit juices, and alcohol can also make your symptoms worse.
Try keeping a bladder diary, to see which type of fluid may irritate your bladder. It is difficult, but reducing or cutting out these fluids can help reduce your symptoms. Swap to decaffeinated, herbal tea, or water. Aim to drink one and a half to two litres of fluid a day (three to four pints).
It is tempting to reduce the amount you drink to less than this, but that can lead to dehydration and will not help your symptoms.
Bladder training
It is easy to get into the habit of going to the toilet too often, and this will make your overall symptoms worse as your bladder can become smaller and hold less and less urine. Bladder training aims to help you get rid of bad habits and relearn ways to stop your bladder from controlling you and your life.
What is bladder training?
The aim of bladder training is to increase the time that you can safely go between toilet visits. This should help you to increase the amount of urine that you can hold in your bladder, and to control the feelings of urgency when you need the toilet.
A bladder training program should also help you to identify the messages that your bladder is giving, and to learn when your bladder is full or not.
Remember that it may have taken months or years for your bladder to develop the bad habits, and changing these habits will not mean that you regain control immediately. Although bladder training may take up to three months to become established, you will start to notice an improvement within two weeks.
Make sure that you have been cleared of any possible urinary infection before you start any training.
How will keeping a fluid diary help?
Keeping a fluid diary can help you to go to the toilet less often. The diary will give you baseline information about your bladder, but continuing to keep a diary can help to reduce the number of times that you go to the toilet. If you are going more than once in an hour, try to stretch the time between toilet visits to an hour and 15 minutes.
Use the techniques in the next section to help you to hold on for longer.
How to improve urgency and urge leakage?
Try all of these ideas to control the urgency and make your bladder wait longer. See which idea
suits you and use them when you need to.
Tighten your pelvic floor muscles as hard as you can, and for as long as you can. Keep doing this until the feeling of urgency goes away or is under control. Contracting (squeezing) your pelvic muscles can help to keep your urethra (tube from your bladder) shut. Tighten your pelvic floor muscles quickly and as hard as you can, and then let go. Repeat this several times in a row.
Another way of lessening the urgency is to put firm pressure on your perineum (crotch area). You can do this by crossing your legs or sitting down on a firm surface. This can send a message to your bladder via the nerves that the outlet from your bladder is closed, so it should wait before it tries to empty.
Distract your mind. Some people start to count backwards from 100, but use whatever technique you can.
Change your position and it may decrease the feeling of urgency. Sometimes leaning forward can help.
Stay still when you get an urge. You will not be able to rush to the toilet and stay in control all at the same time.
Try not to jiggle on the spot. Movement will jolt your bladder and make the problem worse.
Extra hints
The following can also make OAB symptoms worse.
If you are overweight or prone to constipation, please discuss this with your physiotherapist or nurse as they may be able to help you.
There are some medications that can make it more difficult to control your bladder, so let your physiotherapist or nurse know what medication you take on a regular basis.
Drink normally (around one and a half litres per day) to keep hydrated. A lack of fluid can make OAB worse and lead to urinary infections.
Make sure that you reduce how much caffeine, energy drinks, fruit juice, and fizzy fluids you drink. Alcohol and green tea can also irritate bladder symptoms.
Space out how much you drink throughout the day. Drinking large amounts at once can overload your bladder and worsen urgency.
Avoid drinking two hours before going to bed, as this will help you to not get up at night.
Are medications available to treat OAB?
There are a variety of medications that can help an overactive bladder. Although these can help your bladder, it is still important to control what you are drinking and train your bladder.
The medications are designed to enable you to hold on for longer, reduce how often you need to go to the toilet (day and night), and also to reduce leaking.
These tablets are called Oxybutynin (also known as Kentera or Lyrinel XL), Tolterodine (Detrusitol XL) Fesoterodine, Trospium Chloride (Regurin, Regurin XL), Vesicare (Solifenacin), Darifenacin (Emselex), and Propiverine (Detrunorm).
In addition to these, there is another medication called Mirabegron (Betmiga). This tablet works in a different way, and can be used as an alternative to the treatments listed above.
Are there side effects to taking the medication?
Most of the medications have some side effects such as a dry mouth, constipation, and / or reflux symptoms. It is important to know that not everyone will have side effects; in fact some people have very few or no side effects.
If you do have side effects your doctor or nurse may be able to change your medication to one that you can tolerate better.
What other treatments are available?
Changing the amount you drink, bladder training, and medication help a large number of women with OAB symptoms. A small number of women may still have symptoms despite these treatments. In this case, the following treatments may be offered.
Botulinum toxin (Botox)
Botulinum toxin can be injected into the bladder wall via a telescope, usually under a local anaesthetic (the area is numbed). It causes relaxation of the bladder muscle, which in turn reduces urgency. This allows the bladder to hold on better. Although we do not have long-term results for Botox, it is thought to be an effective treatment (up to eight in every 10 women notice an improvement). The effect lasts around nine months, so it does need repeating. In addition there is up to a one in five risk that you may have difficulty emptying your bladder after the procedure. Please ask a member of staff for more information about this procedure.
Tibial Nerve Stimulation
This treatment aims to stimulate the nerves that control how the bladder works, through a nerve that passes around the ankle. It involves inserting a small needle near the ankle, which is connected to a device which then stimulates the tibial nerve. This indirectly stimulates and can control the bladder symptoms.
Sacral Nerve Stimulation
This treatment directly stimulates the nerves that control how the bladder works. It involves implanting a nerve stimulator inside the body, and so it is a treatment only offered by some specialists to people with persistent severe symptoms that have failed to improve after other treatments.
Who will decide what treatment I have?
Your doctor or GP will discuss which treatment is best for you and your symptoms. Please feel free to ask any questions at this stage.
What if I have any questions or concerns?
This leaflet aims to answer any questions you may have about your overactive bladder. However, if after reading this you still have questions or concerns involving your treatment or condition, please speak to the healthcare professional responsible for your care.