Overactive bladder (OAB)
Information for patients from the Urogynaecology Department
An overactive bladder (OAB) is a very common problem. It can cause distressing symptoms that are difficult to control. These can include a frequent urge to go to the toilet. It can also result in leakage before you reach the toilet.
This leaflet will explain the following.
How a normal bladder works.
What an overactive bladder is.
What the symptoms and causes of an overactive bladder are.
How patients are tested for an overactive bladder.
What the treatment options are.
What the alternative treatments are.
What bladder training is, and how to improve urgency and urge leakage.
What medication is available to treat OAB.
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
How does a normal bladder work?
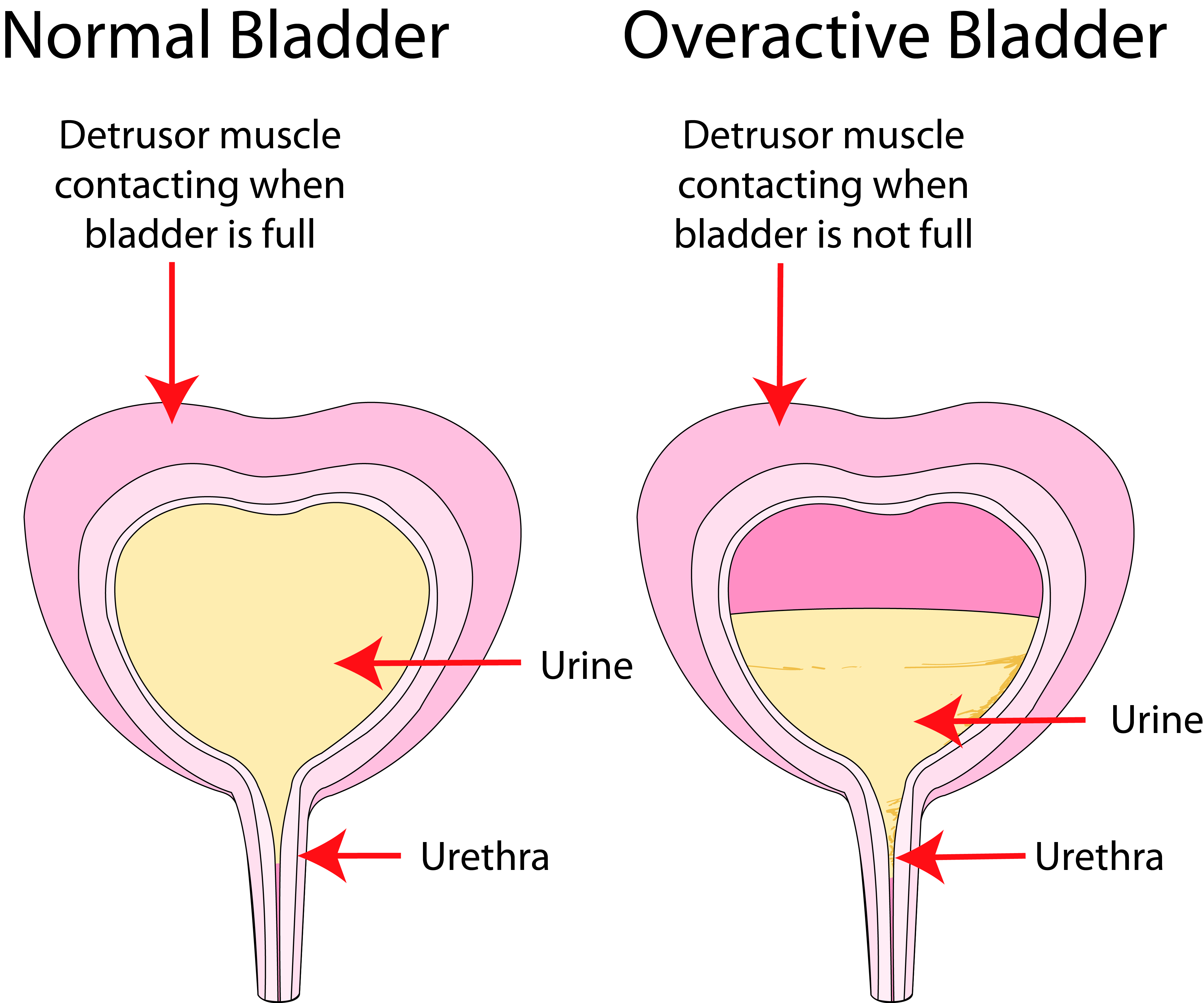
The bladder is similar to a balloon. As urine is produced and the bladder fills, the bladder walls stretch to deal with the extra fluid. Urine is kept inside the bladder by a “valve”, which is called the urinary sphincter. This valve is normally shut (except when you are emptying your bladder).
The pelvic muscles also help to keep urine in. They tense up when you exercise or cough, and help the valve to stay closed.
As your bladder fills up, you may feel an urge, but you are able to hold on. When you decide to empty your bladder (in the toilet), your brain sends a signal to the muscle of your bladder to squeeze and empty your bladder. At the same time, your valve and pelvic floor relax and allow the urine to flow out.
The bladder usually needs to be emptied between 4 to 7 times a day, and once at night.
What is an overactive bladder (OAB)?
An overactive bladder can be caused by the bladder wall muscles squeezing out urine from the bladder at the wrong times. This often happens without warning, and when you do not want it to.
What are the symptoms of an overactive bladder?
An overactive bladder can cause the following symptoms.
Urgency is a sudden and intense need to pass urine that cannot be put off. This can happen even when your bladder is not full. Sometimes you may not make it to the toilet in time and may leak. This is called urge incontinence.
Frequency is going to the toilet too many times during the day (more than seven).
Nocturia is waking up more than once to go to the toilet.
What causes an overactive bladder?
OAB affects people of all ages, and is not simply a result of getting older.
Urinary infections can be a cause of OAB symptoms. It is important to rule out infection at an early stage.
Bladder stones, growths, or inflammation in the bladder can also cause OAB symptoms.
If you have had an operation for stress incontinence or other pelvic surgery, this can irritate your bladder and cause these symptoms.
OAB can be caused by some neurological conditions, such as Multiple Sclerosis (MS).
The amount and type of fluids that you drink are known to significantly worsen OAB symptoms. Try to avoid caffeinated fluids, like tea and coffee.
How will I be tested for an overactive bladder?
A doctor or nurse will assess you, and ask you questions about:
your bladder;
fluid intake (how much you drink); and
general health.
They will also check a Urinalysis. This is where we screen your urine for infection or blood in your urine.
We may examine you to rule out any gynaecology problems, that may be contributing to your problem. We may also ask you to fill in a fluid diary to chart:
your fluid intake (and type); and
how much and how often you pass urine.
This chart can provide valuable information on how to help improve your symptoms.
We may also suggest the following tests.
Residual urine. If your bladder is not emptying completely, this can cause symptoms that suggest overactive bladder. We may ask you to empty your bladder. We will check the residual volume using an ultrasound machine, or possibly a small catheter.
Urodynamics is a series of tests that investigate causes of incontinence. These tests can sometimes diagnose if your bladder wall muscle is squeezing inappropriately.
What treatments are available?
Lifestyle changes
There are changes that you can make to your lifestyle that can help improve your symptoms. Drinks containing caffeine (such as tea, coffee, and coke) can make OAB symptoms a lot worse. Fizzy fluids (including fizzy water), fruit juices, and alcohol can also make your symptoms worse.
Try keeping a bladder diary, to see which type of fluid may irritate your bladder. It is difficult, but reducing or cutting out these fluids can help reduce your symptoms. Swap to decaffeinated, herbal tea, or water. Aim to drink 1.5 to 2 litres of fluid a day (3 to 4 pints).
It is tempting to reduce the amount you drink to less than this, but that can lead to dehydration. It will not help your symptoms.
Bladder training
It is easy to get into the habit of going to the toilet too often. This will make your symptoms worse, as your bladder can become smaller and hold less and less urine. Bladder training aims to help you get rid of bad habits. It helps you relearn ways to stop your bladder from controlling you and your life.
What is bladder training?
The aim of bladder training is to increase the time that you can safely go between toilet visits. This should help you to:
increase the amount of urine that you can hold in your bladder; and
control the feelings of urgency when you need the toilet.
A bladder training program should also help you to identify the messages that your bladder is giving, and to learn when your bladder is full or not.
Remember that it may have taken months or years for your bladder to develop the bad habits. Changing these habits will not mean that you regain control immediately. Although bladder training may take up to 3 months to become established, you will start to notice an improvement within 2 weeks.
Make sure that you have been cleared of any possible urinary infection before you start your training.
How will keeping a fluid diary help?
Keeping a fluid diary can help you to go to the toilet less often. The diary will give you baseline information about your bladder. If you are going more than once in an hour, try to stretch the time between toilet visits to an hour and 15 minutes.
Use the techniques in the next section to help you to hold on for longer.
How to improve urgency and urge leakage?
Try all these ideas to control the urgency and make your bladder wait longer. See which idea(s) suits you, and use them when you need to.
Tighten your pelvic floor muscles as hard as you can, and for as long as you can. Keep doing this until the feeling of urgency goes away or is under control. Contracting (squeezing) your pelvic muscles can help to keep your urethra (tube from your bladder) shut. Tighten your pelvic floor muscles quickly and as hard as you can, and let go. Repeat this several times in a row.
Another way of lessening the urgency is to put firm pressure on your perineum (crotch area). You can do this by crossing your legs or sitting down on a firm surface. This can send a message to your bladder via the nerves that the outlet from your bladder is closed, so it should wait before it tries to empty.
Distract your mind. Some people start to count backwards from 100, but use whatever technique you can.
Change your position and it may decrease the feeling of urgency. Sometimes leaning forward can help.
Stay still when you get an urge. You will not be able to rush to the toilet and stay in control all at the same time.
Try not to jiggle on the spot. Movement will jolt your bladder and make the problem worse.
Extra hints
The following can also make OAB symptoms worse.
If you are overweight or prone to constipation, please discuss this with your physiotherapist or nurse. They may be able to help you.
There are some medications that can make it more difficult to control your bladder. Tell your physiotherapist or nurse what medication you take on a regular basis.
Drink normally (around 1.5 litres per day) to keep hydrated. A lack of fluid can make OAB worse and lead to urinary infections.
Make sure that you reduce how much caffeine, energy drinks, fruit juice, and fizzy fluids you drink. Alcohol and green tea can also irritate bladder symptoms.
Space out how much you drink throughout the day. Drinking large amounts at once can overload your bladder and make urgency worse.
Avoid drinking 2 hours before going to bed. This will help you to not get up at night.
Are medications available to treat OAB?
If bladder training and drinks advice does not work, we may prescribe you medication called an anticholinergic.
We may also prescribe anticholinergics if you have overactive bladder syndrome. Overactive bladder syndrome is the frequent need to urinate. It can happen with or without urinary incontinence. Anticholinergic medications include the following.
Solifenacin
Oxybutynin
Tolterodine
Darifenacin
These are usually taken as a tablet you swallow. However, oxybutynin also comes as a patch that you place on your skin twice a week.
You will usually start taking a low dose to minimize any possible side effects. We can increase the dose until the medicine starts working.
If the medication is helping after 4 weeks, we will arrange a repeat prescription from your GP. We will assess you every 6 to 12 months, if the medication remains effective.
If there is no improvement after 4 weeks or you cannot tolerate the side effects, please let us know. We can consider an alternative.
What are the side effects of anticholinergics?
Possible side effects of anticholinergics include:
dry mouth;
constipation (not pooing as often or finding it hard to poo);
blurred vision; and /or
extreme tiredness (fatigue).
In rare cases, anticholinergics can lead to a build up of pressure in the eye, called angle closure glaucoma. We advise you not to take this medication if you have closed angle glaucoma or are susceptible to it.
Other conditions where anticholinergics should be avoided include:
dementia;
severe ulcerative colitis; and
myasthenia gravis.
We also need to be cautious if you have heart disease or gastro-oesophageal reflux disease.
What if anticholinergics don't work or I'm having unpleasant side effects?
We may offer you an alternative medicine, such as mirabegron or vibegron, if anticholinergics are:
unsuitable for you;
they have not helped your urge incontinence; or
you are having unpleasant side effects.
These medicines cause the bladder muscle to relax, which helps the bladder fill up and store urine. They usually come as a tablet or capsule that you swallow once a day.
If the medication is helping after 4 weeks, we will arrange a repeat prescription from your GP. We will assess you every 6 to 12 months, if the medication remains effective. You will need blood pressure monitoring if you continue on mirabegron.
Common side effects of mirabegron and vibegron can include:
constipation (not pooing as often or finding it hard to poo);
diarrhoea (poo is loose / runny and watery);
feeling sick (nausea); and /or
headaches.
If you have kidney or liver disease, we need to take care prescribing this medication. A lower dose may be appropriate or we may need to find an alternative.
Mirabegron needs to be used carefully if you have raised blood pressure, and avoided if this is not well controlled.
Vibegron should not be used if you have:
galactose intolerance;
total lactase deficiency; or
glucose-galactose malabsorption.
Both medications can cause urinary retention and affect digoxin levels.
What other treatments are available?
Changing the amount you drink, bladder training, and medication help a large number of women with OAB symptoms. A small number of women may still have symptoms despite these treatments. In this case, we may offer the following treatments.
Botulinum toxin (Botox)
We can inject botulinum toxin into the bladder wall via a telescope. This is usually done under a local anaesthetic (the area is numbed). Botox causes relaxation of the bladder muscle, which in turn reduces urgency. This allows the bladder to hold on better.
Although we do not have long-term results for Botox, it is thought to be an effective treatment. Up to 8 in every 10 women notice an improvement. The effect lasts around 9 months, so it does need repeating. In addition there is up to a 1 in 5 risk that you may have difficulty emptying your bladder after the procedure. Please ask a member of staff for more information about this procedure.
Tibial Nerve Stimulation
This treatment aims to stimulate the nerves that control how the bladder works. This is done through a nerve that passes around the ankle. It involves inserting a small needle near the ankle. The needle is connected to a device, which stimulates the tibial nerve. This indirectly stimulates and controls bladder symptoms.
Sacral Nerve Stimulation
This treatment directly stimulates the nerves that control how the bladder works. It involves implanting a nerve stimulator inside the body. It is a treatment only offered by some specialists, to people with persistent severe symptoms that have failed to improve after other treatments.
Who will decide what treatment I have?
Your doctor or GP will discuss which treatment is best for you and your symptoms. Please feel free to ask any questions at this stage.
What if I have any questions or concerns?
This leaflet aims to answer any questions you may have about your overactive bladder. If you have any further questions or concerns, please speak to a member of your healthcare team.
We have used the term ‘women’ in this leaflet. When we use this term we also mean people with female reproductive organs who do not identify as a woman. East Kent Hospitals is committed to supporting people of all gender identities. Please tell your nurse or doctor how you would like them to address you, so we can be sure to get this right.
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email