Osteoarthritis at the base of the thumb
Information for patients from the Orthopaedic Hand Service
You have been diagnosed with osteoarthritis at the base of your thumb. This leaflet will explain:
what osteoarthritis is
the surgery you might need; and
what to expect after surgery.
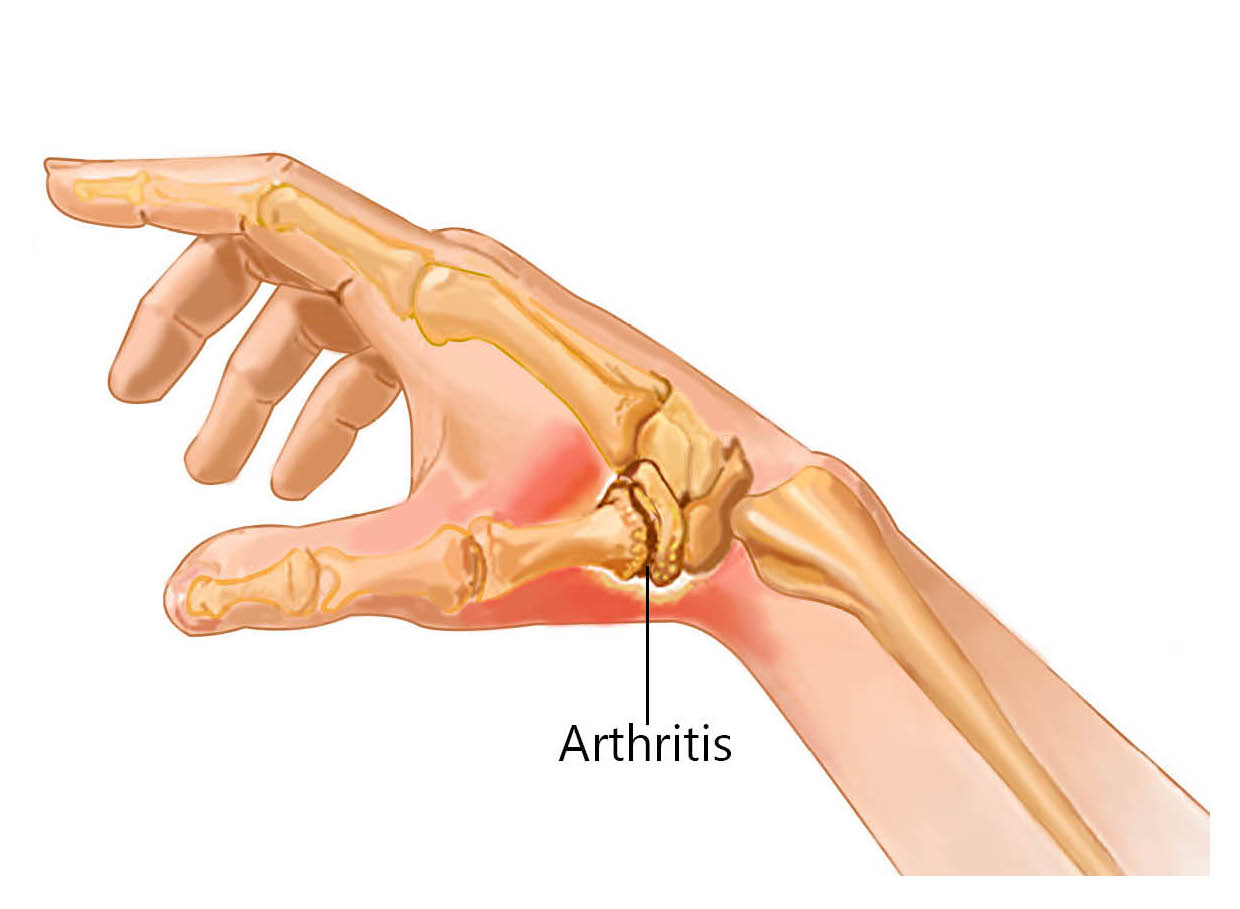
Osteoarthritis around the base of the thumb is a very common condition. It is most often part of the normal age-related changes to our joints. Joints that have been injured before are more likely to develop arthritis and the thumb is more vulnerable to this.
What are the symptoms of osteoarthritis?
To begin with you might feel pain when you carry out certain activities. People often say they feel pain when:
they pinch their thumb to open packets or peel vegetables; or
they do not have a strong grip anymore due to the pain.
As osteoarthritis progresses, you may have:
swelling at the base of your thumb
pain even when resting; and
your thumb may appear crooked.
Progression varies from person to person.
How is osteoarthritis diagnosed?
Your GP may be able to recognise this form of arthritis by looking at your hand and discussing your symptoms. Or they may refer you to a hand therapist or hand surgeon to make the diagnosis and begin treatment.
X-rays may be taken, but are not essential for diagnosis in the early stages of the condition.
What are my treatment options?
Hand therapy
Hand therapy can include advice on managing and changing your daily activities, to help manage your pain. This may include:
hand exercises to keep your hand moving and working correctly
hand exercises to strengthen your hand; and
splints to reduce symptoms and help your hand work properly.
Injections
A local steroid injection can be given into your arthritic joint, but whether you have this will depend on how bad your osteoarthritis is. Steroid injections can often provide good pain relief. However, this may only be temporary, lasting from several months to a year or two. Sometimes steroid injections can be repeated.
Surgery
If your osteoarthritis is very painful and other treatments are no longer helping, surgery may be an option. The aim of surgery is to reduce pain and increase what you can do with your hand without pain.
Various anaesthetics can be used for the surgery. These include:
a general anaesthetic, where you are asleep for the procedure; or
a regional anaesthetic, where only your arm is numb and you are awake.
Surgery usually takes around 1 hour.
What are my surgical options?
There are several surgical options available. Your consultant will discuss with you which is the most suitable option for you.
Trapeziectomy is currently the most common surgery. It involves the complete removal of the small bone at the base of your thumb, called the trapezium.
Removing this bone provides more space for your thumb to move, so the arthritic bone surfaces are not rubbing together causing pain.
Some surgeons fill the gap left by the removed bone using a piece of tendon from your wrist, called a ligament reconstruction.
Arthrodesis (also known as joint fusion) is a type of surgery that is less common. It is only suitable for certain people, for example:
those who have developed arthritis at a younger age; and
those who do heavy manual work.
Arthrodesis involves fixing the trapezium bone and the metacarpal bone together at the base of your thumb, to stop the bones rubbing together. However, this procedure does not always stop the pain. If this is the case, the trapezium may need to be removed (see Trapeziectomy above).
Artificial joint implant.
The MAIA prosthesis is a total joint replacement (ball and socket type joint). It also gives good pain relief and good movement to the thumb following surgery. Studies have shown that 9 years after surgery, 9 in 10 patients (90%) who have had this implant fitted, still have good pain relief.
-
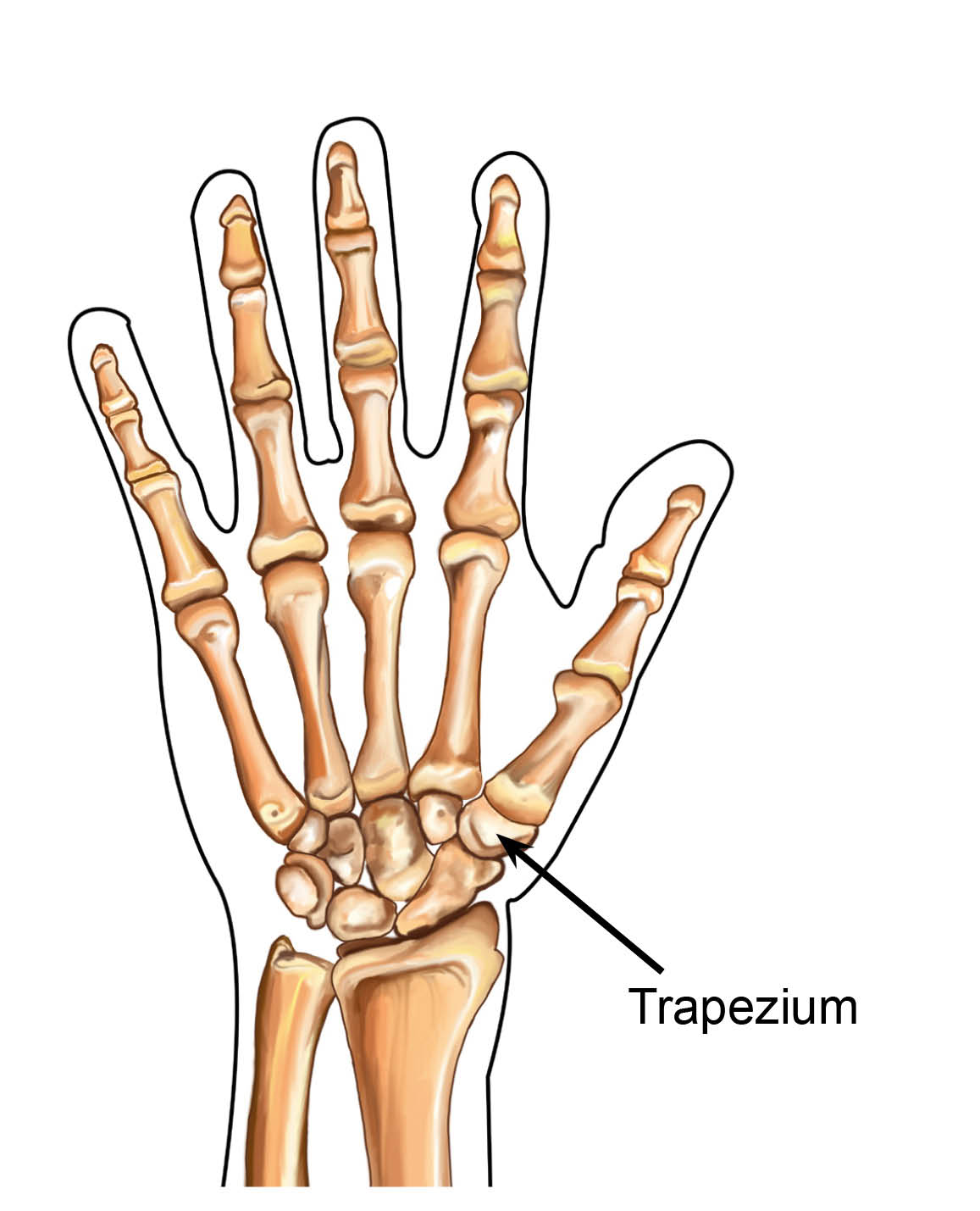 The small bone at the base of your thumb, called the trapezium.
The small bone at the base of your thumb, called the trapezium. -
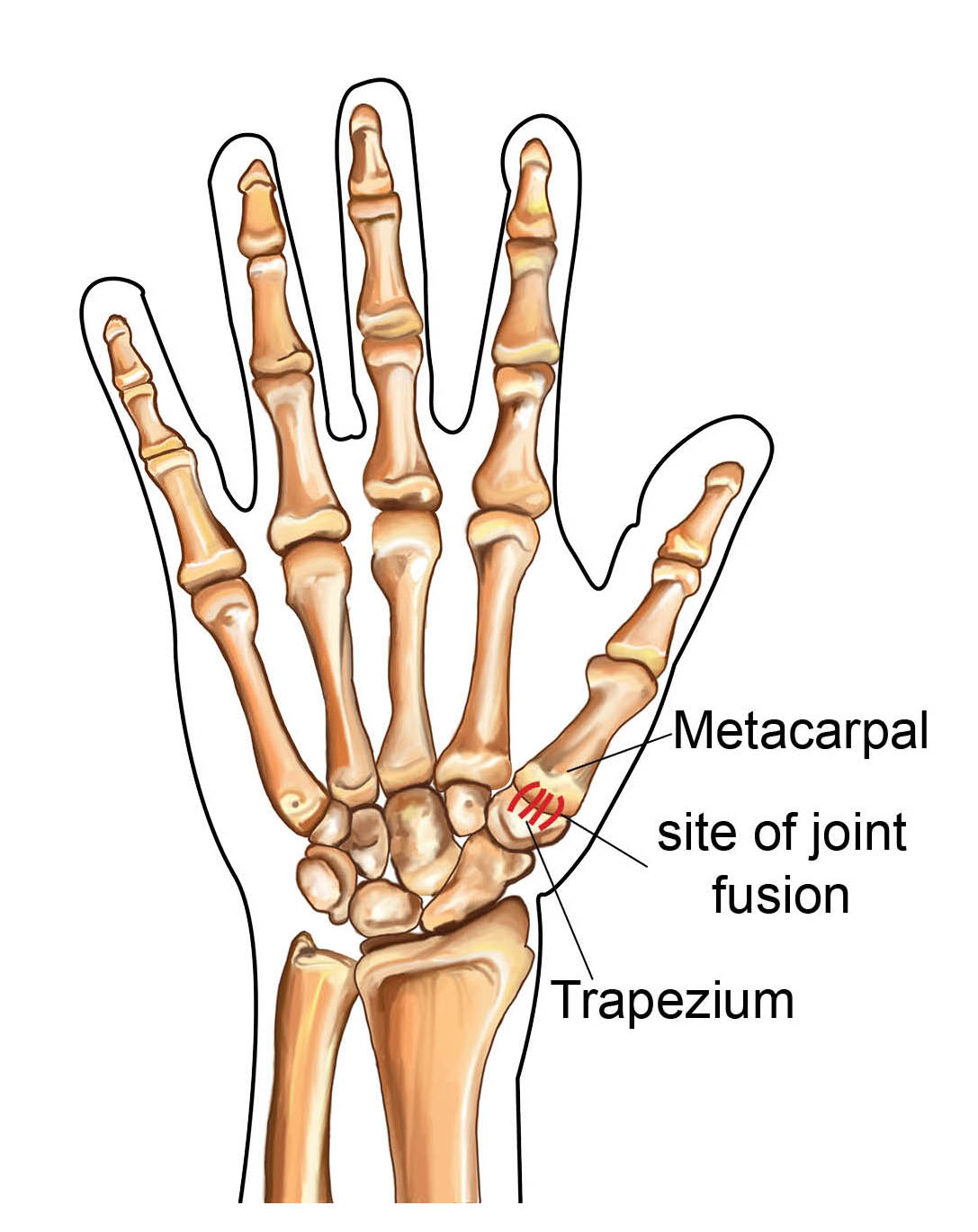 The metacarpal bone and trapezium bone fixed together at the base of your thumb
The metacarpal bone and trapezium bone fixed together at the base of your thumb -
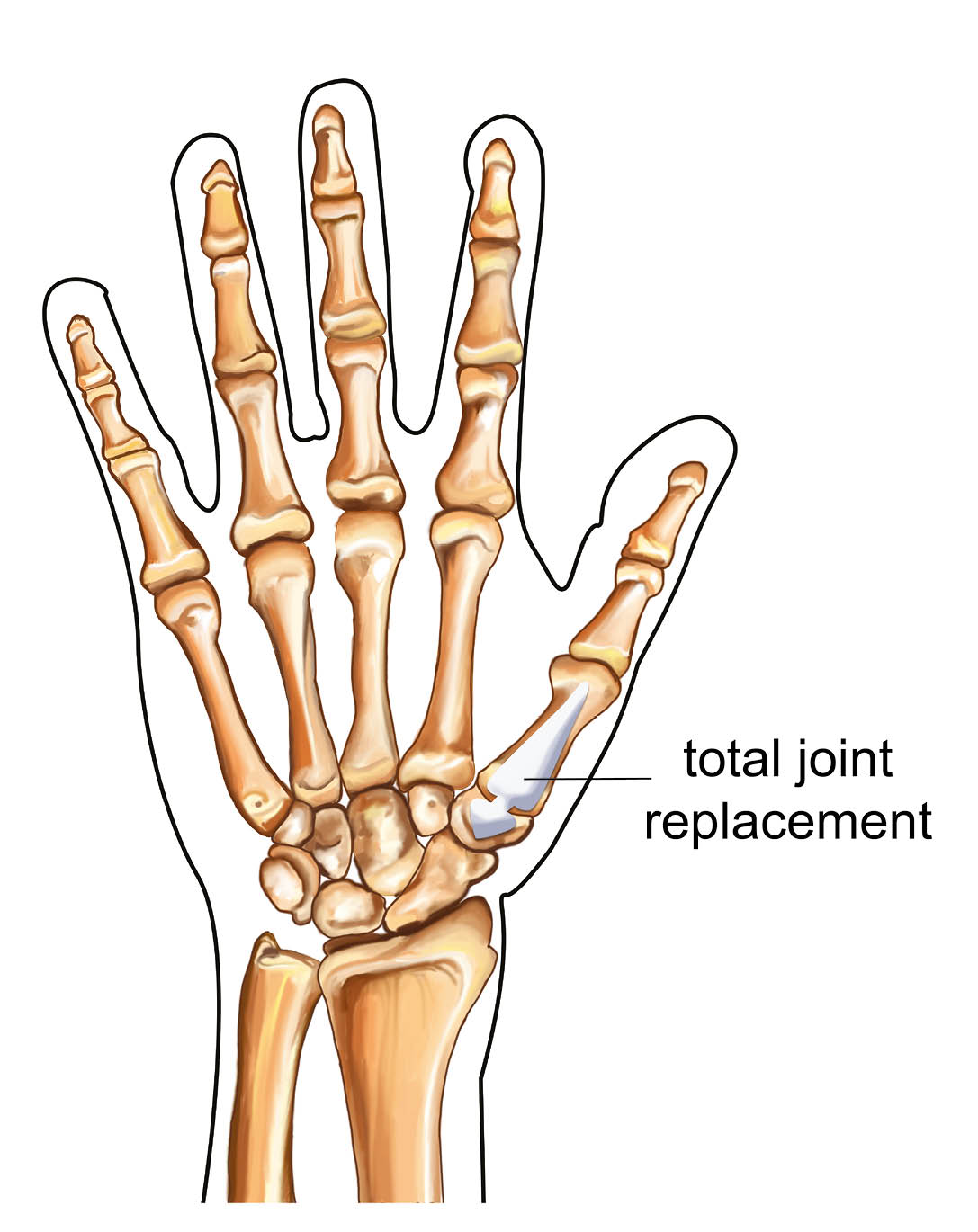 MAIA prosthesis
MAIA prosthesis
How long will I be in hospital?
These surgeries are carried out as day case procedures, so you will go home on the same day as your operation. Plan to be in hospital for up to 6 hours.
You cannot drive after your surgery. Please make sure you arrange for someone to take you home after your operation.
What are the risks and possible complications from surgery?
As with any surgery, complications can happen. However, with these procedures they tend to be relatively mild if they do. By being aware of the possible complications, you may be able to help your doctor or therapist catch them early.
Complications can include the following.
Delayed wound healing or infection. A small number of patients will develop an infection and may need antibiotics. Very rarely they may need a further small operation to clean out their wound, called a washout procedure. This is more common in patients with diabetes.
Your scar may be tender for a number of months. If it does not get better with time and regular scar massage, you may need a course of therapy.
Joint replacements carry a small risk of implant problems. These problems can include loosening, wearing out, or dislocation of the implant. With the current design this happens to less than 1 in 100 patients (1%). If a problem does develop after this surgery, you may be offered a second trapeziectomy operation.
Stiffness may develop in your thumb or fingers. This is usually short-term, but it is important that it settles quickly (within 3 months) to avoid permanent stiffness.
Pain can continue in approximately 1 in every 10 patients (10%), even after surgery.
Nerve damage can occur during your surgery. This may result in:
a painful spot in your scar (neuroma); or
some numbness around the scar or your thumb.
This often settles within a couple of months.
Complex Regional Pain Syndrome (CRPS) is a rare but serious complication. The nerves in the hand “over-react”, causing swelling, pain, discolouration, and stiffness. If this happens, patients may need therapy to try to settle this.
Your hand therapist and consultant will work with you to help resolve these symptoms.
Please remember that most patients have an uncomplicated routine operation with very satisfactory recovery and outcomes. If you have questions or concerns about the risks and complications, please speak to your consultant or therapist.
What happens before my operation?
Before the day of your surgery, you will have an appointment at the Pre-assessment Clinic.
At this appointment, a nurse will discuss your operation with you.
You may need to have some tests before your operation, such as a blood test.
You will be asked some questions about your general health.
Please bring a list of your usual medicines to your pre-assessment appointment. The nurse will need to know their names and strengths. This includes non-prescription medicines, such as herbal or complementary medicines.
If you need to stop eating or drinking before your surgery (fasting), this will be explained to you at this appointment.
Please feel free to ask questions and raise any concerns that you may have about your operation.
Stop smoking. Compared to non-smokers, smokers are more likely to experience complications in tissue healing and infections after injuries or surgery. If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
Please remove any rings from your fingers before arriving at hospital for your operation.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
How should I look after my hand following surgery?
The care of your hand following your surgery is very important. To start with our aim is comfort and elevation of your hand.
Keep your hand above your elbow at the level of your heart as much as possible to reduce the swelling (this is elevation). You will be given a sling to wear after your surgery to help with this.

It is important that you keep your shoulder and elbow moving regularly. To do this remove your sling to stretch out your arm.
Keep your fingers moving within the limits of the bandages, to prevent them from getting stiff.
Will I have a follow-up appointment?
If you have had a Trapeziectomy or MAIA prosthesis, you will have a hand therapy appointment around 10 to 14 days after your surgery.
If you have had an Arthrodesis (joint fusion) you will normally be followed up in the orthopaedic clinic around 6 weeks after your surgery.
At this appointment your therapist will:
remove your bandages
check your wound
make you a splint, which will protect your thumb for 4 to 6 weeks; and
get you started on some exercises.
You will need to return to the hand therapist around every 2 weeks for a couple of months. At these appointments, the therapist will check your progress and help you return to your normal daily activities.
When will my hand start to feel better?
Most people will return to their normal daily activities 3 to 4 months after their surgery. However, it can take 6 to 9 months for your hand to fully settle.
How will my hand feel following my operation?
You may have some bruising and pain following your operation. This should be controlled by taking simple painkillers, such as paracetamol and ibuprofen.
The anaesthetic can stay in your system for up to 72 hours, so do not be alarmed if your hand remains numb for a few days after your surgery. Please contact your consultant if your hand remains numb after 72 hours.
What should I do if I am concerned about my hand?
You should contact 111 or your local Urgent Treatment Centre if you have any of the following.
Loss of feeling in your hand or fingers.
Discoloration of your hand or fingers.
Your fingers become hot or cold most of the time.
Increased swelling or tenderness in your hand or fingers.
Increase in pain in your hand or fingers.
You are worried about an infection.
When will my stitches be removed?
In most cases, dissolvable stitches are used. These will start to fall out on their own 10 to 14 days after your surgery.
If you have not had dissolvable stitches, you will need to have your stitches removed either by your therapist, GP practice nurse, or consultant. You will be advised of this at the time of your surgery.
What size scar will I have? and, how many stitches will I have?
The length of the scar will vary from patient to patient, but is usually 3 to 4cm long. The number of stitches varies as well, but the surgeon will aim to make your scar look as good as possible.
When can I return to work?
This depends on the work you do, whether you drive to work, and what surgery you had. If you need advice, please speak to your consultant or therapist.
If you are in a supervisory or managerial job that does not need full use of your hand, you could return to work within a few days of your surgery.
Other light manual jobs may need a longer time off, for example 6 weeks.
Heavy manual jobs may need you to be off work for 3 to 6 months.
When can I return to driving?
Please arrange for someone to drive you home on the day of your surgery.
Do not drive for at least 4 weeks following a MAIA Prosthesis, or 6 weeks following a Trapeziectomy or Arthrodesis.
Do not drive again until your whole hand feels comfortable and has regained reasonable pain free movement. Your therapist can guide you with this.
What if I have any questions or concerns?
If you have any questions or concerns about your treatment or condition, please speak to your consultant or hand therapist.
Further information
References
NICE guidelines ‘Osteoarthritis on over 16’s: diagnosis and management’ (NG226) Published October 2022
British Society for Surgery of the Hand Evidence for Surgical Treatment (BEST) Evidence based management of thumb base osteoarthritis (Dec 2023).
Alkar et al. (2011) Trapeziometacarpal Maia prosthesis for basal thumb arthritis. A series of 100 prosthesis with a minimum follow-up of 3 years. Chirurgie de la Main 30:S77-S82.
Andrzejewski, A., Ledoux, P. (2019) Maia trapeziometacarpal joint arthroplasty: Survival and clinical outcomes at 5 years’ follow-up. Hand Surgery and Rehabilitation 38: 169–173.
Davis, T.R., Brady, O., Barton, N.J., Lunn, P.G., Burke, F.D. (2004). Trapeziectomy alone, with tendon interposition or with ligament reconstruction. Journal of hand surgery [BR], 22B (6): 689-694.
Group Lepine (2021) Trapezomatacarpal Joint Prostheis MAÏA™
Seaourt, A-C., Dap, F., Dautel, G., Athlani, L. (2021) Comparison between the MAIA® Implant and Trapeziectomy for Trapeziometacarpal Osteoarthritis: Outcomes at 9 Years’ Follow-Up. The Journal of Hand Surgery (Asian-Pacific Volume) 26(2):158-165.
Toffoli, A., Teissier, J. (2017). MAÏA Trapeziometacarpal Joint Arthroplasty:
Clinical and radiological outcomes of 80 patients with more than 6 years of follow-up. Journal of Hand Surgery Am., 42(10): 838.e1-e8.
Wajon, A., Ada, L. Edmunds, I. (2005) surgery for thumb (trapeziometacarpal joint) osteoarthritis- Cochrane database systematic review, Oct 19;(4):CD004631.
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email