Nerve block catheters for pain relief in rib fractures
Information for patients from the Anaesthetics Department
You have been admitted to hospital with a rib fracture. Your doctor has recommended that you have a nerve block to help with any pain. This leaflet will explain the following.
What a nerve block is, and how it can help.
What happens during the procedure.
What the risks are to having the nerve block.
What will happen if you choose not to have the block.
What to do if you have any concerns.
If you have any further questions, please speak to a doctor or nurse caring for you.
What are nerve blocks?
When bones (such as ribs) break (fracture), pain is often caused by the nerves surrounding the broken bones.
Nerve blocks use local anaesthetic to block the nerves supplying the broken bones. The local anaesthetic blocks the signals (including pain) travelling along the nerves. This means that you will not feel the pain from the rib fractures.

The nerve block is given by an injection through the skin, to the area where the nerve is located. This is done using an ultrasound machine, so that your doctor can:
see directly where the injection is going, and
make sure other structures like blood vessels (arteries and veins) are not affected.
A catheter (small plastic tube) is then placed in the correct position and used for continuous pain relief.
The skin is numbed before we perform the nerve block, to make it less painful. However, you can expect some discomfort.
What are the benefits of nerve blocks in rib fractures?
The nerve block will give fast and effective pain relief. The pain relief will allow you to breathe, cough, and move more easily. This will help you sit up and move around sooner. It also reduces the chances of you developing complications of rib fractures, like pneumonia.
Nerve blocks mean you have less need for stronger painkillers, such as codeine and morphine. These painkillers can make you feel:
sick
drowsy or lightheaded, and
may cause constipation (not pooing as often or finding it hard to poo).
What happens if I choose not to have the nerve block?
If you choose not to have a nerve block, the Pain team will continue to see you whilst you are in hospital. They will make changes to your pain medication. These changes are based on how well the medication is working and whether your pain is under control.
If you wish to change your mind and have a nerve block for pain relief, you can do this at any time during your stay in hospital.
What happens during the nerve block?
The procedure takes around 30 minutes to prepare and perform. We usually perform the procedure at the patient’s bedside. If your doctor needs to carry out the procedure in a theatre, they will explain why.
The skin around the injection site will be cleaned.
An injection of local anaesthetic will numb your skin; this will sting a little.
The doctor will use an ultrasound machine to directly see the area to be numbed. Most people find that the injection is no more painful than having a cannula (drip) inserted into a vein.
A continuous peri-neural local anaesthetic catheter is inserted through the needle. This is held in place with dressings to the skin.
The injection usually gives some relief quite quickly, but it can take between 20 and 40 minutes to work fully.
About 30 minutes after the procedure, your doctor or nurse will check:
your pain, and
whether you can take a deep breath and cough.
If the block does not work fully, you will be given more pain relief.
What is a continuous peri-neural catheter?
A peri-neural catheter is a long, thin tube. It is positioned next to the nerves that supply feeling to your broken ribs. You may have one or two of these catheters in place.
The catheter is attached to a pre-programmed pump. The pump delivers local anaesthetic to continuously numb the nerves. The purpose of a peri-neural catheter is to provide continuous pain relief, to allow you to take deep breaths and cough effectively.
Living with the catheter
The injection site will not be painful. You will be able to lie on it if you wish.
You can wear a hospital gown over the top of the catheter, and move around freely. Please be careful though, as you will be attached to a pump via an infusion line.
If you wish to be disconnected for any reason, please tell your nurse.
If the line is pulled or knocked, please tell your nurse. They can check whether the catheter has dislodged.
What happens afterwards? And, how long will the nerve block last?
The nerve block usually lasts 8 to 12 hours after a single injection.
The peri-neural catheter will usually stay in place for 48 to 96 hours. It can stay for as long as 2 weeks, if needed.
Whilst you are on the ward, you and the catheter will be checked regularly to make sure it is working well.
Once your team decides to remove the peri-neural catheter or the local anaesthetic infusion is stopped, it will take several hours for the feeling in the numbed area to return to normal. If your discomfort increases, you may need to take more oral painkillers.
The catheter will only be removed when your pain is controlled on oral painkillers. If your pain is not controlled after stopping the continuous infusion of local anaesthetic, this can be restarted and your oral painkilling medication checked. The infusion will be discontinued again a couple of days later.
What are the risks, side effects, and complications of nerve blocks?
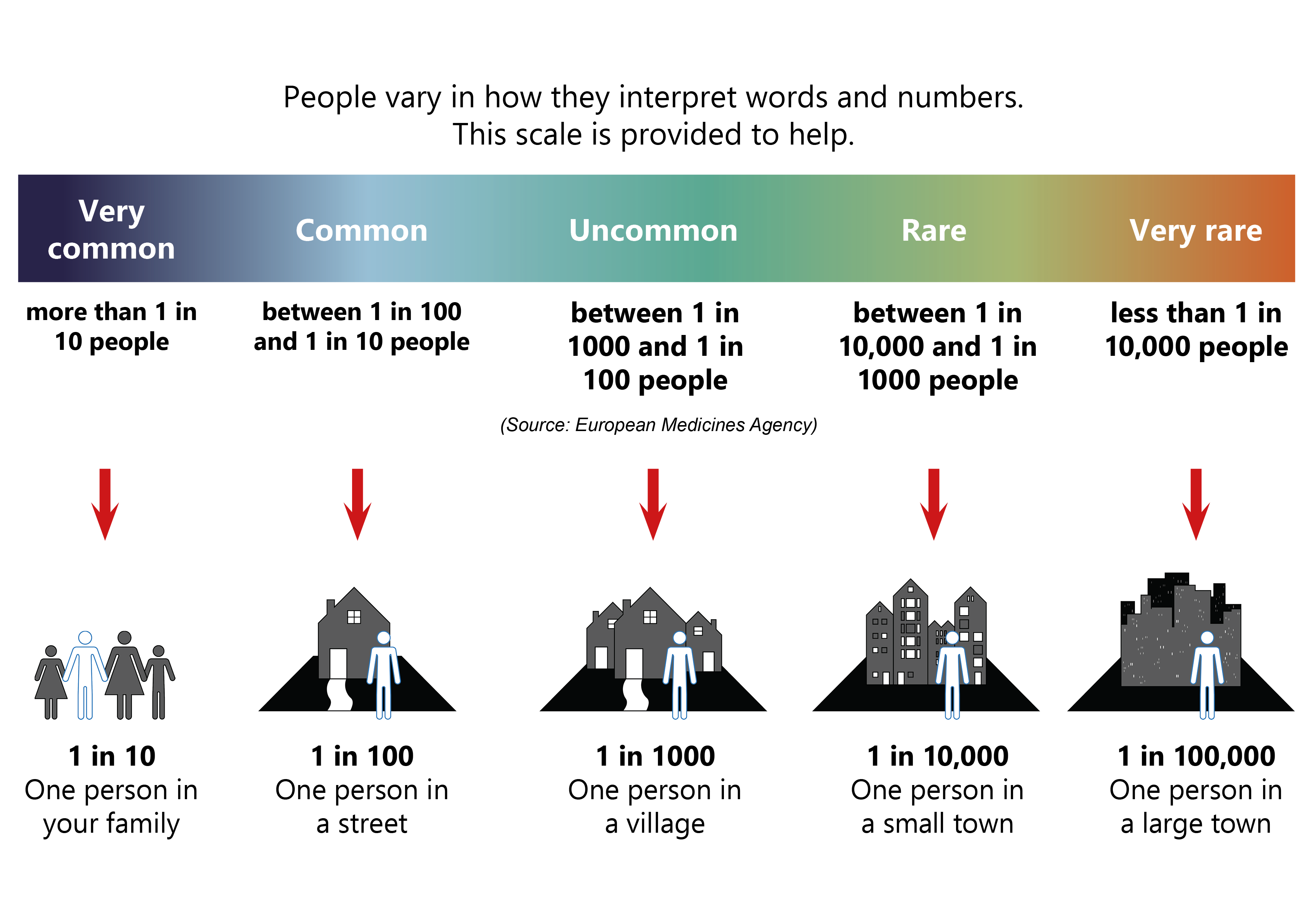
Serious problems are uncommon but risk cannot be removed completely. Modern drugs, equipment, and training have made nerve blocks safe procedures. All doctors and nurses take care to avoid the risks discussed in this section.
There is an uncommon risk (less than 1 in 1000) of damage to the covering of the lung. This can lead to some degree of collapse of the lung, called a pneumothorax. Air goes into the space between the chest wall and the lung, called the pleural space.
Treatment will depend on how big this is. It may cause no symptoms at all and just be noticed on a chest x-ray. However, if it is large and you become short of breath, you may need a chest drain to help manage the pneumothorax. A chest drain is a plastic tube that is inserted through the chest wall. It drains the air through a special vacuum drain until the lung damage has healed.
There is a rare risk of puncturing a blood vessel. This is minimised by viewing where the needle is going under direct vision and by checks used when the local anaesthetic is injected.
There is a very rare risk of having a fit or another life-threatening event. Your doctor and nurse will manage these promptly and tell you more about these very rare events.
Nerve damage is rare. There may be numbness or tingling in your chest that will not go away. For most patients (95 in every 100 (95%)), these symptoms will resolve within six weeks. After a year this increases to 99% of patients.
There is a rare risk of a reaction to the local anaesthetic. Before your nerve block, your doctor or nurse will ask if you have had any reactions in the past. You will be closely monitored for any signs of a reaction during and after the block. The doctor and nurse will manage any reaction promptly and appropriately.
If you have any questions or concerns about these risks, please speak to your doctor.
What about risks of having the catheter?
The catheter may move away from the nerve or become kinked. The local anaesthetic may then not reach the nerves and may no longer be effective. If you notice that the catheter has come away from your skin or your pain has worsened, please let the nurse looking after you know. They will ask for an anaesthetist or one of the Pain team to come and see you.
Any foreign body or break in the skin can be a source of infection. Precautions against infection are taken during insertion, and infection is uncommon. Should you develop an infection, it may need treatment with antibiotics.
If you notice that the skin around your catheter insertion site has become red, hot, swollen or painful, please let the nurse looking after you know. The nurse will arrange for an anaesthetist or one of the Pain team to come and see you.
You may have some mild bruising around the insertion site. This is common and will get better on its own.
Depending on where the peri-neural catheter is placed, there may be localised side-effects. These will be explained to you. These will resolve when the effects of the local anaesthetic wear off.
Please be aware of the following advice
Do not change the settings on the pumps yourself. This could be dangerous to you or the equipment.
Take care of the pre-programmed pump and catheter equipment. The nerve catheter may become dislodged.
Please try to keep the insertion site clean and dry, to reduce the risk of infection.
Do take care. If needed, ask for help before walking or getting out of bed.
Tell your nurse if:
You have pain in the area to be blocked.
You have difficulty breathing.
The pump alarms.
The nerve catheter becomes disconnected.
There is any leakage from the nerve catheter.
You notice redness or swelling around the catheter insertion site.
You think you may have side-effects from the local anaesthetic.
You feel dizzy, or have tingling in your lips, blurred vision, or feel unwell.
Contact details
If you have any questions or concerns, please speak to the team looking after you.