Nephrectomy: physiotherapy advice for before and after your surgery
Information for patients having a nephrectomy, who have been referred to the POPS (Perioperative Care of the Older Person Undergoing Surgery) Team
This booklet will give you information on how you can best prepare for your nephrectomy, to make your journey as smooth as possible.
What are the different types of surgery I may have?
Open radical nephrectomy involves removing the whole kidney and its surrounding tissues, through an abdominal (stomach) or loin incision (cut).
Open partial nephrectomy involves removing only the part of the kidney containing the tumour, through an abdominal or loin incision.
Robotic-assisted partial nephrectomy involves removing part of the kidney containing the tumour, using a keyhole (laparoscopic) procedure with robotic help. This technique leaves a smaller wound, and recovery after surgery is often quicker.
Your surgeon will discuss these options with you, and decide with you what the best course of treatment for you is.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
Why is exercise before and after surgery important for my recovery?
Before your surgery, it is important to be as healthy and as fit as possible. Following the advice in this booklet will help you recover more quickly after your surgery.
Do you know what the minimum amount of exercise the average person should complete each week is?
The following advice is from the World Health Organisation (WHO). It outlines the recommended amount of exercise each adult should do each day.
Guidelines for adults (aged 18 to 64)
At least 30 minutes a day of moderate activity*, five days a week (or 150 minutes a week).
Guidelines for older people (aged 65+)
At least 30 minutes a day of moderate intensity activity, five days a week (or 150 minutes a week). Focus on aerobic activity, and muscle-strengthening and balance exercises.
* Moderate activity means that while carrying out the exercise your breathing and heart rate will increase, but you are still able to speak to someone. You should feel warm or be sweating slightly, but the pace of the exercise should be comfortable.
For more information, please visit the WHO web site.
Are you already doing the amount of exercise needed each week? If not, please follow the advice and exercises in this leaflet. Remember, the fitter you are before your surgery, the more quickly you will recover afterwards.
Before surgery: how can I safely increase how much exercise I do?
If you do not already take part in any physical activity, please use the following advice to get you started, along with the instructions you have been given by your POPS consultant and nurses at your clinic appointment.
Start with a few minutes of activity each day, such as a 5 to 10 minute walk.
Complete the exercise program below twice a week, and build-up to three times a week when you can.
Gradually increase to 30 minutes of moderate intensity activity (such as the exercise program below, swimming, dancing, or cycling) one or two days a week. Plus, a 10 minute walk every other day.
Your aim is to reach 30 minutes of exercise, five days a week. With at least two of these days including strengthening exercises (see exercises in this leaflet).
If you are active, but do less than the recommended levels:
Gradually increase the amount of exercise you do each day, until you reach the 30 minutes of moderate activity each day, five days a week.
How can I exercise safely, and when should I stop?
In order to keep yourself safe whilst exercising, it is important to consider the following points.
Do not exercise if you are feeling unwell.
Do not exercise where it is too hot or too cold.
Do not exercise straight after a large meal; wait for an hour before you exercise.
Always wear comfortable clothing and sensible footwear.
Make sure you have enough space to do your exercises safely.
You should stop exercising if:
you have any chest pain or tightness
you feel dizzy; or
you become very breathless.
After your first few exercise sessions it is normal to have some muscle soreness, but this should get better after a few days. However, if your joint or muscle pain continues you should contact your GP for advice.
Exercises to do before your surgery
Complete the following strength exercises 2 to 3 times each week, whilst increasing the amount of walking you are doing each week.
Sit to stand
Stand up and sit down from a chair, without using your hands as a support if possible.
Try to do this exercise as many times as you can in 30 seconds. Complete it slowly and controlled (do not rush).
Increase how many times you do the exercise as it becomes easier, and then complete for 1 minute.
Going up and down steps / stairs
Using the stairs is a great way to improve your fitness levels.
If you do not have stairs use a step.
Holding onto a bannister / railing or something sturdy and fixed that will not move, practice going up and down the bottom step as many times as you can in 1 minute.
Build up to 2 minutes when 1 minute feels easy, then aim for 3 minutes.
Bend the elbow, reach the ceiling
Stand or sit (whichever makes you feel more comfortable) holding a tin of beans or a weight that you are comfortable with.
Bend your elbow, bringing the weight up to your shoulder.
Hold for a second, then reach your arm / weight to the ceiling.
Bring your arms back down, and straighten your elbow, before repeating.
Complete 10 times, then rest.
Repeat the above twice.
-
(1)
-
(2)
-
(3)
-
(4)
-
(4)
Lateral raise
Hold on to a tin of beans as a weight by your side (if the weight is too heavy, practice with no weight). Make sure your nails are facing forward.
Keep your elbows straight and bring your arms out to the side to shoulder height, slowly lower down.
Complete 10 times, then rest.
Repeat the above twice.
-
(1)
-
(2)
-
(2)
How does stopping smoking help my recovery after surgery?
Quitting smoking is the most important step you can take to help your recovery and improve your long-term health. After surgery, smoking increases your risk of getting a chest infection and can slow down healing. It is important to stop smoking before your surgery.
Our friendly NHS advisers offer free, non-judgemental support. You are up to four times more likely to quit with our help. We provide nicotine replacement therapy (NRT) free of charge, which doubles your chance of staying smoke free long-term. Ask your health professional to refer you, or phone our freephone number below to self-refer.
Support available
Kent and Canterbury Hospital is a smoke-free site, but NRT is available while in hospital and to take home on discharge, if appropriate.
Support is available on a one-to-one or group basis at various places across Kent. We also offer telephone and video appointments.
Whether you want to be a healthier weight, get active, quit smoking, cut down on alcohol, or just feel better about life, One You Kent offer free support to help YOU.
For more information or to self-refer call: 0300 123 1220
Email: kentchft.oneyoukent@nhs.net or visit our web site.
What do I need to bring with me to hospital?
After your surgery, staff will encourage you to get out of bed, get dressed in your own clothes, and get active while you are on the ward. Being in your own clothes will make you feel more comfortable to get up and walk around the ward. With this in mind, please bring the following items to hospital with you.

Loose fitting trousers or shorts
Loose fitting short sleeved t-shirts
Trainers / shoes
Underwear
Socks
Dressing gown
Supportive / comfortable slippers; ideally slippers that have backs to prevent them slipping off your feet
Your walking aid (such as a Zimmer frame or walking stick) (if applicable)
Your medication / inhalers / chest clearance appliances (if applicable)
A phone to contact your family
Glasses / hearing aid (if applicable); each ward has purple sensory boxes where you can keep glasses and hearing aids safe, accessible, and together.
What will happen during my hospital stay?
Hospital gowns
You will need to wear a hospital gown while in the Critical Care Unit / High Dependency Unit. During your time on these units you will be attached to machines, and wearing a hospital gown makes it easier to access these. When the machines are removed, you should start wearing your own clothes again.
Managing your pain
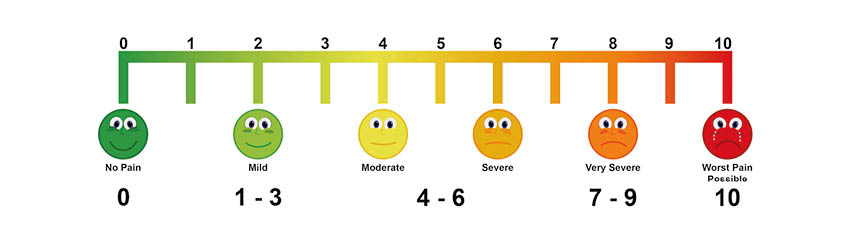
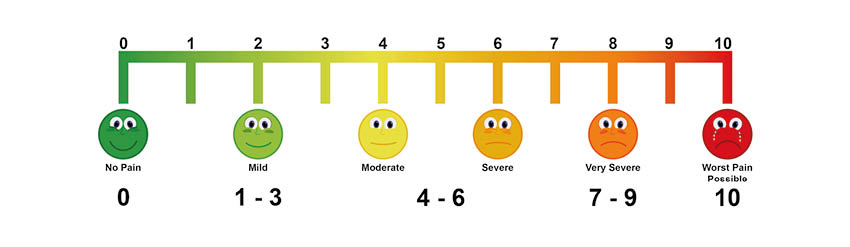
Controlling your pain after surgery is important. It will allow you to move, breathe, eat / drink, and sleep. Speak to your nurse if your pain reaches 4/10.
Why are breathing exercises important for my recovery?
A chest infection is a common complication after surgery.
Research has shown that breathing exercises and encouraging air to get to the bottom of your lungs as soon as you wake up after surgery, is important to prevent a chest infection.
Your doctor / physiotherapist will ask you to use an ‘incentive spirometer’ to help you take deep breaths.
Put the mouthpiece in your mouth and close your lips tightly around it. Slowly breathe out (exhale) completely.
Breathe in (inhale) slowly through your mouthpiece as deeply as you can. As you take the breath, you will see a ball rise inside.
To start with, try to get one ball up and hold it at the top for 2 to 3 seconds, or as long as you can.
When this becomes easier, try to lift the second and third ball, holding the deep breath for as long as you can.
Repeat five times.
Repeat these steps every half hour that you are awake.
-
One ball lifted
-
Two balls lifted
-
Three balls lifted
What are ankle exercises?
Ankle pump exercises
Blood clots are another common complication of surgery and bed rest. Research shows that moving your ankles up and down while in bed, and getting up and moving around are important ways of preventing a blood clot from forming.
Every 30 minutes bend your ankles up and down.
Bend each ankle 10 times.
-
With your leg out in front, point your foot upwards
-
With your leg out in front, point your foot downwards
-
Return to starting position
Why is goal setting important for my recovery?
Below are the goals you must aim to achieve each day following your surgery. The entire ward team will help you to meet these goals.
When I wake up after surgery
Breathing: I will start my breathing exercises to prevent a chest infection (see Why are breathing exercises important for my recovery?).
Activities: I will start my ankle pumps to prevent clots (see Ankle pump exercises).
Pain control: I will tell my nurse if my pain reaches 4/10.
Nutrition: I will eat and drink, as advised by my surgeons.
Attachments: You will have many lines / tubes attached to you following your surgery; your team will help you manage these, and can explain what each does.
Day 1 after surgery
Breathing: I will continue deep breathing exercises every 30 minutes.
Activities: I will sit on my chair for as long as I can throughout the day; you will be helped to your chair by your physiotherapist / nurse. I will try to wash myself. If you have abdominal (stomach) pain / discomfort while doing these activities, the physiotherapist might suggest you use a walking aid to start with. They will make a decision based on how you are doing / feeling.
Pain control: I will tell my nurse if my pain reaches 4/10.
Nutrition: I will eat and drink, as advised by my surgeons.
Attachments: You will have many lines / tubes attached to you following your surgery; your team will help you manage these.
Going home: Patients who have had keyhole (laparoscopic) surgery may go home one to two days after their surgery.
Day 2 after surgery (begin to think about going home)
Breathing: I will continue deep breathing exercises every 30 minutes.
Activities: I will sit out of bed for as long as I can. I will continue to complete personal hygiene tasks for myself (such as washing myself). I might continue to use a walking aid to support myself when moving, this can help with any abdominal pain I may feel. I will reach my walking goal daily, as set by the team.
Pain control: I will tell my nurse if my pain reaches 4/10.
Nutrition: I will eat and drink, as advised by my surgeons.
Attachments: these may be removed today.
Day 3 onwards after surgery
Breathing: I will continue deep breathing exercises every 30 minutes. The more you walk and do things yourself, the less you will need to do the breathing exercises, as walking will help your lungs to expand.
Activities: I will work towards becoming independent on the ward, including walking to and from the toilet myself (if my physiotherapist has told me this is safe). I will think about what I need to do to get home safely, for example I will practice stairs with the physiotherapist if I need to use stairs at home.
Pain control: I will tell my nurse if my pain reaches 4/10.
Nutrition: I will eat and drink, as advised by my surgeons.
Going home: some patients will go home by day 2 to 4. Following these goals will help you be more ready for home.
How should I continue my recovery at home?
Recovery times vary from one patient to another. It can take several weeks or even a few months to feel like you are ‘back to normal’. This depends on how healthy and active you were before surgery.
The best way to recover after surgery is to slowly increase your level of physical activity over three months.
It is normal to feel tired for at least 4 to 6 weeks after your operation. You might need a short sleep in the afternoon for a few weeks, as you gradually increase your level of activity. It is good for you and your family to be aware of this.
Do not lift anything heavy (such as a child, full saucepan, or vacuum cleaner) until six weeks after your surgery.
What if I have any questions when I return home?
If you have questions about anything discussed in this leaflet, please contact one of the following.
Clinical Specialist Physiotherapist, POPS Team
Telephone: 07955 320901POPS Team
Telephone: 01227 783043Urology Suite, Kent and Canterbury Hospital
Telephone: 01227 864383
.JPG)
.JPG)
.JPG)
.JPG)
-1686913432.JPG)
.JPG)
.JPG)
-1686913392.JPG)
.JPG)
.JPG)
.JPG)
.JPG)
-1686916901.JPG)
-1686917060.JPG)
.JPG)
-1686917109.JPG)
.JPG)
.JPG)
.JPG)
.JPG)
.JPG)
-1686919362.JPG)