Myosure
Information for patients from Women's Health
What is MyoSure?
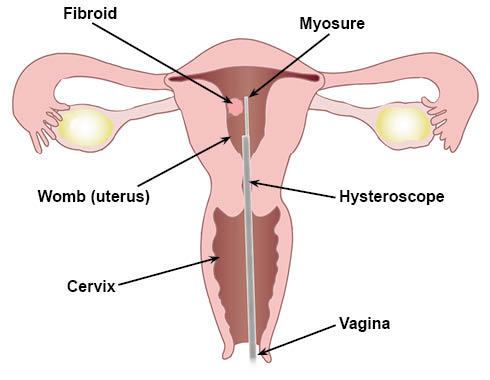
MyoSure is a small device placed inside a narrow telescope. The telescope has a camera and light source, and is called a hysteroscope.
The device is inserted into the womb through the vagina and cervix.
This allows the operator to remove polyps and fibroids within the womb.
Who undergoes a MyoSure procedure?
Myosure is recommended if a polyp or fibroid is found in a patient's womb during an ultrasound or hysteroscopy, and needs further investigation and / or management.
Please be aware that you cannot have this procedure if you are pregnant, or think that you might be. You may have a urine pregnancy test carried out on the day of your procedure.
What are polyps and fibroids?
Polyps are small, usually benign (non-cancerous) growths in the lining of the womb. They can cause heavy periods, bleeding between periods and after sex, and pain.
Fibroids are growths of muscle cells in the womb, which are usually non-cancerous. They can cause heavy, painful, irregular periods, and may also affect fertility.
How effective is this procedure?
This procedure reduces heavy bleeding caused by polyps or fibroids in nine out of every 10 patients (90%).
The fibroid / polyp will return within three years in three out of every 10 patients (30%). And in less than 10 in every 100 patients (10%) within 5 years.
How safe is this procedure?
A hysteroscopy is a very safe procedure.
Complications occur in less than one in every 100 patients (less than 1%).
What are the possible side effects and risks?
Pain or cramping is normal. You can take over-the-counter pain relief (such as paracetamol) to help with this.
Feeling sick, faint, or dizzy; this is normal and does not last long.
Vaginal spotting or bleeding after the procedure; this is normal. It lasts for a few days after your procedure. If needed, use sanitary towels not tampons; using tampons can cause an infection.
Infection of the bladder or womb. If over-the-counter pain relief does not help your pain or cramps, you may have developed an infection. If this happens, please contact your GP who may prescribe you a course of antibiotics.
Failure to gain entry into the womb or failure to remove the polyp or fibroid. If this happens, you may need to repeat the procedure at another time.
Creating a small hole in the wall of the womb. This happens in less than one in 1000 cases.
If this happens, you may need to stay in hospital overnight for observation.
Very rarely, you may need keyhole or open surgery, to check and repair any damage to tissues such as bowel, bladder, or blood vessels.
How do I prepare for my procedure?
Eat and drink as normal.
Take simple painkillers (such as paracetamol or ibuprofen) an hour before your procedure. This will help with any discomfort you may feel during your procedure.
What will happen during my procedure?
The team looking after you will introduce themselves. This team usually includes a clinician, nurse, and healthcare assistant.
The clinician will discuss your medical history with you. They will explain the steps of the procedure and the potential risks. Please use this time to ask any questions. Remember you have the right to withdraw your consent for treatment at any time.
The clinician will insert an instrument called a speculum into your vagina to keep it open. Speculums are also used during a cervical screening test (smear).
The clinician may recommend you have a local anaesthetic. This will numb your cervix and the surrounding area, so you feel no pain. You will be awake for the procedure.
The hysteroscope is inserted into your vagina. Saline (salt water) fluid will flow through the scope. This will widen / expand your vagina and cervix, so the scope can pass into your womb. It is normal to feel the water coming out.
The team will be able to see inside your womb. You may be able to see it on a screen next to you, if you wish to.
The MyoSure will then be used to gently remove the polyp or fibroid.
The procedure usually takes 10 to 20 minutes.
You may have some cramping (similar to period pain) during your procedure.
How will I feel after my procedure?
Recovery is usually quick, as no cuts or incisions are made to your skin. Most people are able to restart their normal activities after 15 minutes.
You will be able to go home as soon as you feel ready (usually within 15 minutes).
You will be able to drive yourself home.
You may feel mild discomfort for 24 to 48 hours after your procedure. This is usually helped by taking paracetamol or ibuprofen.
You may also have mild vaginal bleeding. Do not use tampons, have sex or a bath, or go swimming until the bleeding has stopped.
When will I get my results?
Any samples taken during your procedure will be sent to the laboratory for testing. The test results will be sent to you and your GP by post. This is usually within a few weeks of your procedure.
What if I have any concerns once I return home?
Please contact your GP as soon as possible, if you have any symptoms of infection. These include:
green or unpleasant smelling vaginal discharge;
feeling feverish (hot) or unwell;
problems with your bladder or bowel; and
abdominal pain, which does not improve.