Monitoring your baby’s heartbeat in labour
Information for women, birthing people, and their families
This leaflet explains what fetal monitoring is, and the methods available to you. It will give you information about how, and when, your baby’s heartbeat can be monitored in labour. This leaflet is not meant to replace the information discussed between you and your midwife or doctor. It can act as a starting point for such a discussion or as a useful reminder of the key points.
This leaflet is based upon the recommendations made by:
The National Institute for Health and Care Excellence (NICE), and
East Kent Hospitals Fetal Monitoring LMNS Guideline.
The Local Maternal and Neonatal System (LMNS) is a group of hospitals which develop and share joint guidance.
What is fetal monitoring? and, why is it offered?
Fetal monitoring is a way of assessing your baby’s wellbeing by monitoring their heartbeat. It does not predict birth outcomes but gives us a snapshot of how your baby is at that moment.
Labour is a natural process, and babies are well adapted to deal with life in the womb and the journey of labour. Contractions in labour temporarily cause a reduction in blood flow to the baby, which is normal. There can be an increase in the pressure in the umbilical cord, which most babies cope well with throughout labour and birth. If changes in their heartrate tell us your baby is no longer coping as we would expect; we may want to intervene. This could mean we recommend that your baby is born earlier.
What are the different types of fetal monitoring available?
Intermittent Auscultations (IA) of your baby’s heartbeat. This is performed regularly throughout labour using a Pinard stethoscope or hand-held Doppler.
Continuous Electronic Fetal Monitoring (CEFM) using a cardiotocograph (CTG) machine.
What is Intermittent Auscultation (IA) with a Pinard stethoscope or hand-held Doppler?
This type of monitoring is recommended in low risk / uncomplicated pregnancies.
On the day you go into labour, a midwife will re-assess yours and your baby’s wellbeing. If anything has changed or increases the risk to yourself or your baby, you may be recommended to use CEFM in labour.
With IA we listen to your baby heartbeat at regular intervals, immediately after a contraction. This is the most stressful time for baby. It is important to see baby’s response to the contractions.
This will tell us how your baby is ‘coping’ in labour. Some changes in your baby’s heart rate may mean we recommend closer observation via the CTG machine.

Pinard stethoscope
A Pinard stethoscope is a trumpet shaped stethoscope. It allows your midwife to listen to your baby’s heart rate through your abdomen (tummy). It is a non-electrical tool, so you will not be able to hear anything yourself. Only the midwife using the Pinard will be able to hear your baby’s heartbeat.

Hand-held Doppler
The Doppler is a handheld ultrasound device that is placed on your abdomen (tummy). Your midwife or doctor and you can hear your baby’s heartbeat through the device’s speaker. It is waterproof and can be used in the birthing pool.
What is Continuous Electronic Fetal Monitoring (CEFM)?
Continuous monitoring keeps track of your baby’s heart rate for the whole of your labour. This is done using a cardiotocograph (CTG) machine.

Elastic belts are used to hold the sensors against your abdomen. These detect your baby’s heartbeat and are connected to a monitor. The monitor records your baby’s heartbeat as a pattern on a strip of paper, as well as the frequency of your contractions. Your midwife or doctor will read and interpret the pattern on the strip of paper.
Continuous monitoring may limit how much you can move around during labour. However, the leads which connect you to the machine have some length and you will still be able to:
stand
kneel
sit, or
use a birth ball beside the monitor.
It may be possible to use wireless CTG monitoring, called telemetry. With this type of monitoring there are no leads connecting you to the machine (like wireless headphones). However, at the moment this service is very limited, as we do not have many machines. If you would like to use this form of monitoring, please speak to your midwife.
Why might we recommend CEFM in labour?
Your midwife or doctor may suggest the use of a CTG (continuous monitoring). The reasons for this will be discussed with you at the time. For example, your midwife or doctor may have noticed a change in your baby’s heart rate when using IA (intermittent monitoring). This may suggest that your baby might need to be monitored more closely to see how they are coping with labour.
The assessment tool midwives use at the beginning and throughout your labour may suggest continuous monitoring is used. If you have any questions, please speak with your midwife or doctor.
Examples of why your doctor or midwife may suggest CEFM
You have pre-existing or gestational diabetes and are taking medicine for this.
You have high blood pressure (hypertension) and are taking medicine for this.
You have been told you have Intrahepatic Cholestasis of Pregnancy (ICP). Previously known as Obstetric Cholestasis (OC). ICP is a liver condition, which can cause severe itching on the body. CEFM is only recommended if your blood tests are abnormal and induction of labour is recommended.
You have had a caesarean birth or surgery on your womb in the past.
You have had a stillbirth in the past.
You have had heavy vaginal bleeding during your pregnancy. This is called an APH or Antepartum Haemorrhage.
You are more than 28 weeks, but less than 37 weeks pregnant.
You are more than 42 weeks pregnant.
You are pregnant with twins.
You have been told that your baby is smaller than it should be. This is called fetal growth restriction.
You have been told that the dopplers taken during your baby’s ultrasound scan are ‘abnormal’.
You have been told there is too little amniotic fluid around your baby (called Oligohydramnios).
You have been told there is too much amniotic fluid around your baby (called Polyhydramnios).
You have prolonged rupture of membranes (PROM). PROM is where the fluid around your baby ‘broke’ more than 24 hours before the start of established labour.
You have had reduced fetal movements in the last 24 hours.
You need to have an epidural for pain relief.
You have meconium in the amniotic fluid around your baby. This is when your baby has had a poo in the ‘waters’.
You have a suspected infection.
If your baby has a baseline heart rate that is not appropriate. It could be too high, too low, or not stable.
This is not a complete list. If you have any questions about any of these examples, please speak with your midwife.
What is a fetal scalp electrode (FSE)?
If we are struggling to monitor your babies heartbeat in labour, a fetal scalp electrode (FSE) may be recommended. A FSE is a small, spiral shaped wire that is placed just beneath the baby's scalp. This gives a more accurate and continuous reading compared to the CTG during labour.
Your midwife or doctor will insert the electrode through your cervix during a vaginal examination. They will carefully attach the electrode to your baby's head. The electrode is then connected to the CTG machine, which tracks your baby's heartbeat.
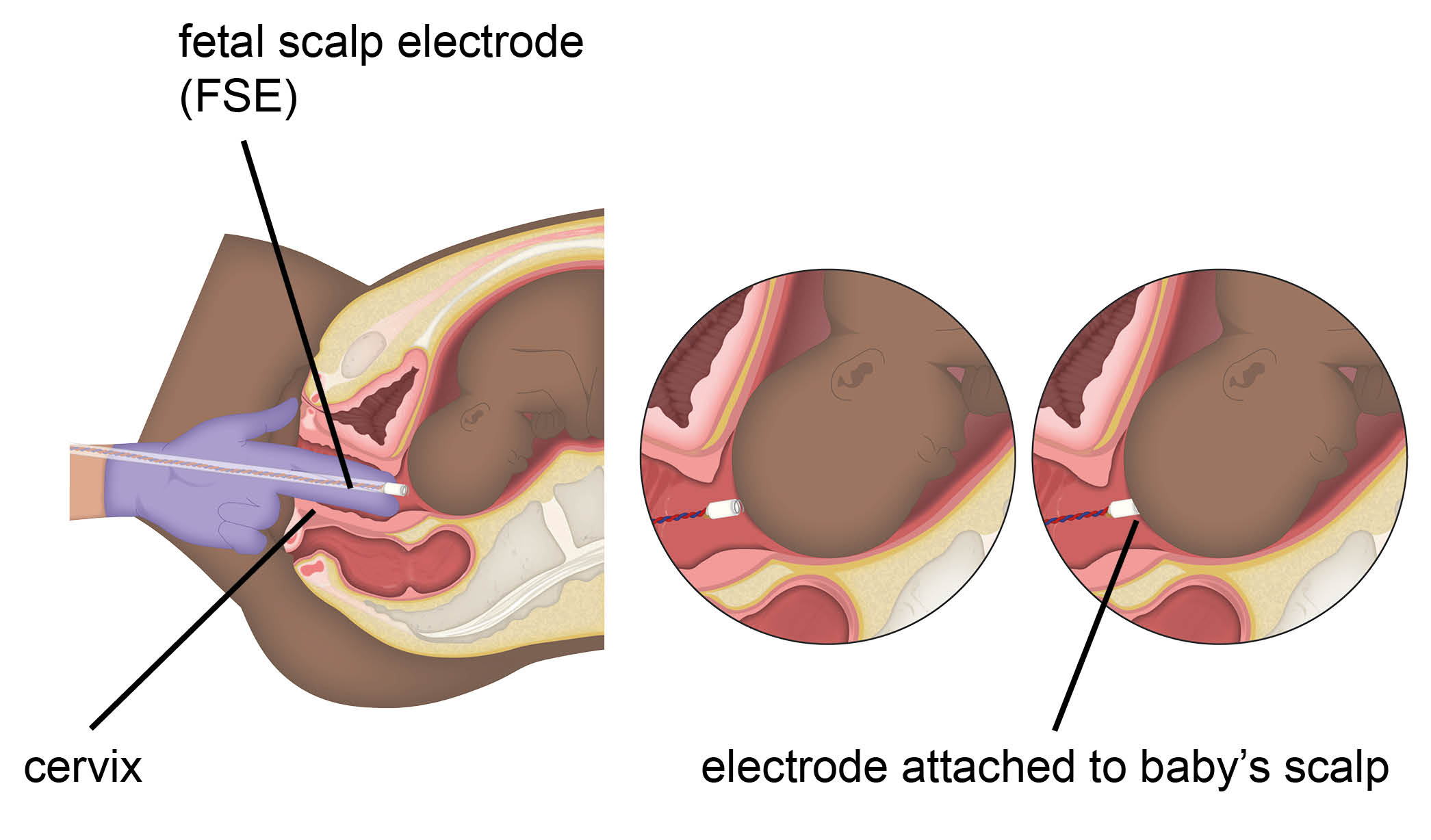
The procedure is generally safe. It does carry some risks, such as:
slight bruising to the baby’s scalp, or
irritation to the baby's scalp.
The waters around your baby need to have 'broken' before an FSE can be used. If they have not 'broken' a midwife or doctor will need to do this. This is called an ARM or artificial rupture of membranes.
The need for more accurate monitoring has to be balanced against the more invasive nature of this type of monitoring. If they think it is necessary, your midwife or doctor will discuss this option with you.
Do I have a choice in how my baby is monitored?
You always have a choice, and the final choice is yours. If you have any questions, speak with your midwife or doctor. They will explain why they think a specific method of monitoring your baby's heartbeat is best for you and your baby.
What happens if I chose to not have any monitoring?
Not monitoring your baby in labour is not nationally recommended, and goes against NICE guidance. Monitoring allows midwives and doctors to act if there are concerns with how your baby is coping. However, this is your choice, and if this is something you are considering please speak with your midwife. They can refer you on the relevant professionals to discuss the risks, and develop a care plan which may be outside of guidance.
Further information
Please speak to your midwife or doctor if you have any concerns about monitoring your baby’s heartbeat. Or, for further information about care in labour, please go to the following web site.
Who can I contact if I have any worries or concerns?
If you have any worries or concerns, please contact your community midwife. Alternatively, you can call Maternity Triage on 01227 206737. Maternity Triage are available for urgent help and advice 24 hours a day. In any cases of emergency contact 999.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email