Mastoid obliteration
Information for patients from the Otology Department
You have been referred for mastoid cavity obliteration surgery. The aim of this surgery will be to eliminate your troublesome mastoid cavity.
This leaflet will explain:
the aims, benefits, risks, and alternatives to mastoid obliteration surgery
what happens during the operation, and
how you will feel afterwards.
If you have any questions after reading this leaflet, please speak to your surgeon.
What can cause a troublesome mastoid cavity?
The most common reason is ear infections that keep recurring (or coming back).
How does the ear work?
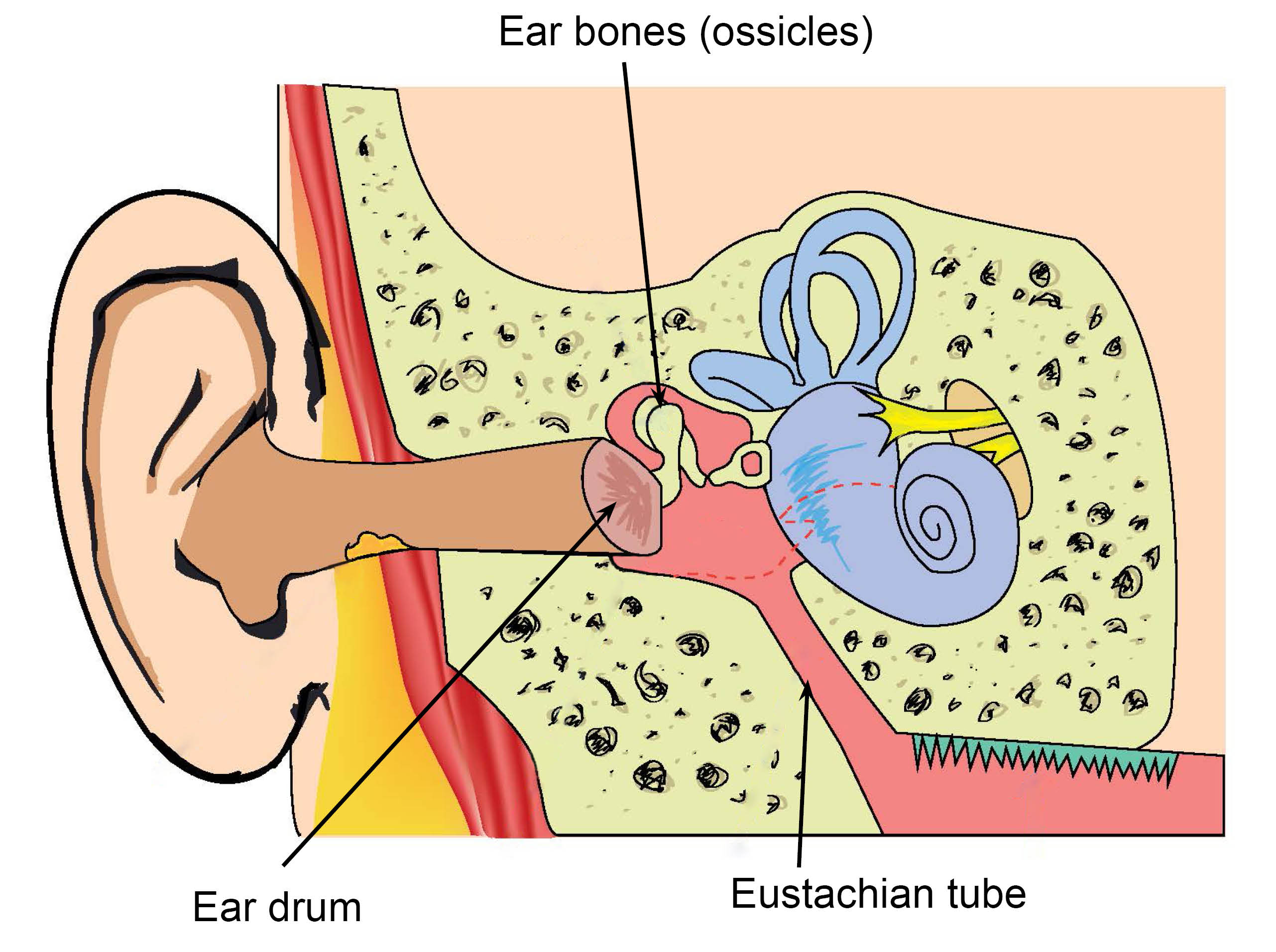
The ear consists of the outer, middle, and inner ear.
Sound travels through the outer ear and reaches the eardrum, causing it to vibrate.
The vibration is then transmitted through three tiny bones, called the ossicles. These bones are in the middle ear.
The vibration then enters the inner ear. This is a snail-shaped bony structure filled with fluid.
The nerve cells in the inner ear are stimulated to produce signals. These signals are then carried to the brain, where the brain interprets them as sound.
What is the mastoid bone?
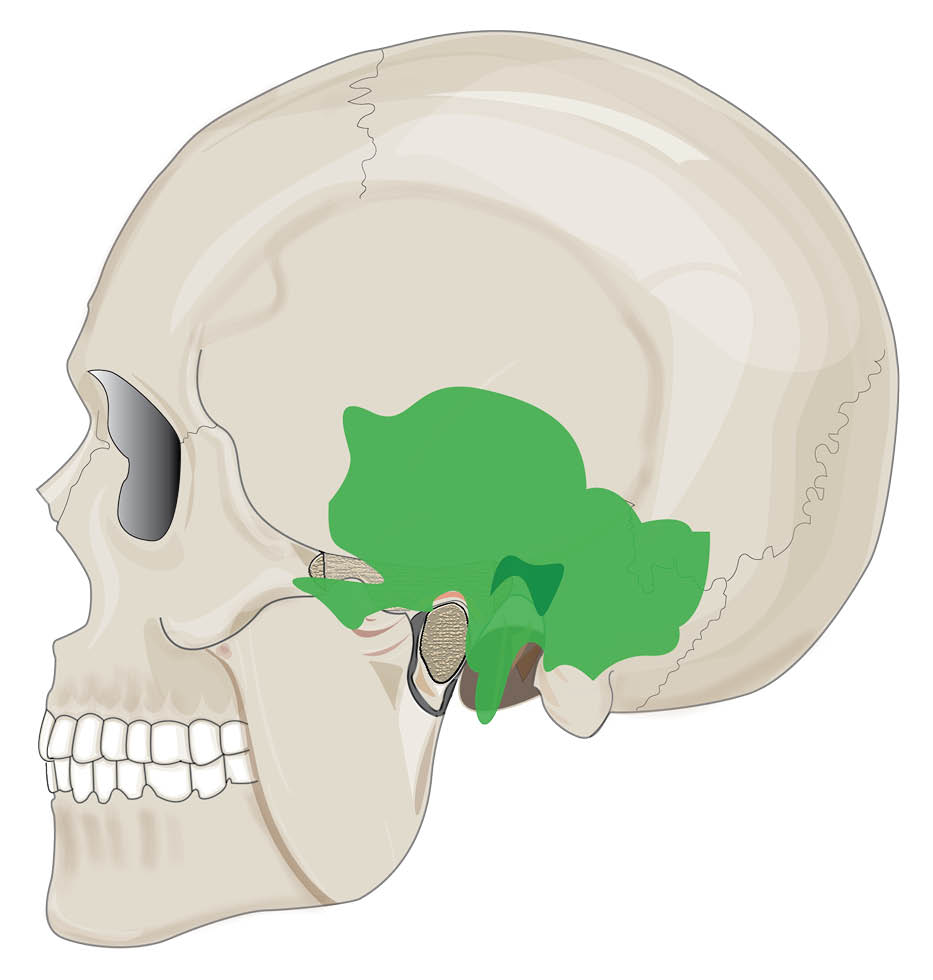
The mastoid bone is the bony prominence that can be felt just behind the ear. It contains many air spaces. The largest is the antrum, and this connects with air space in the middle ear.
Ear diseases in the middle ear can extend into the mastoid bone.
Why have I been referred for mastoid cavity obliteration?
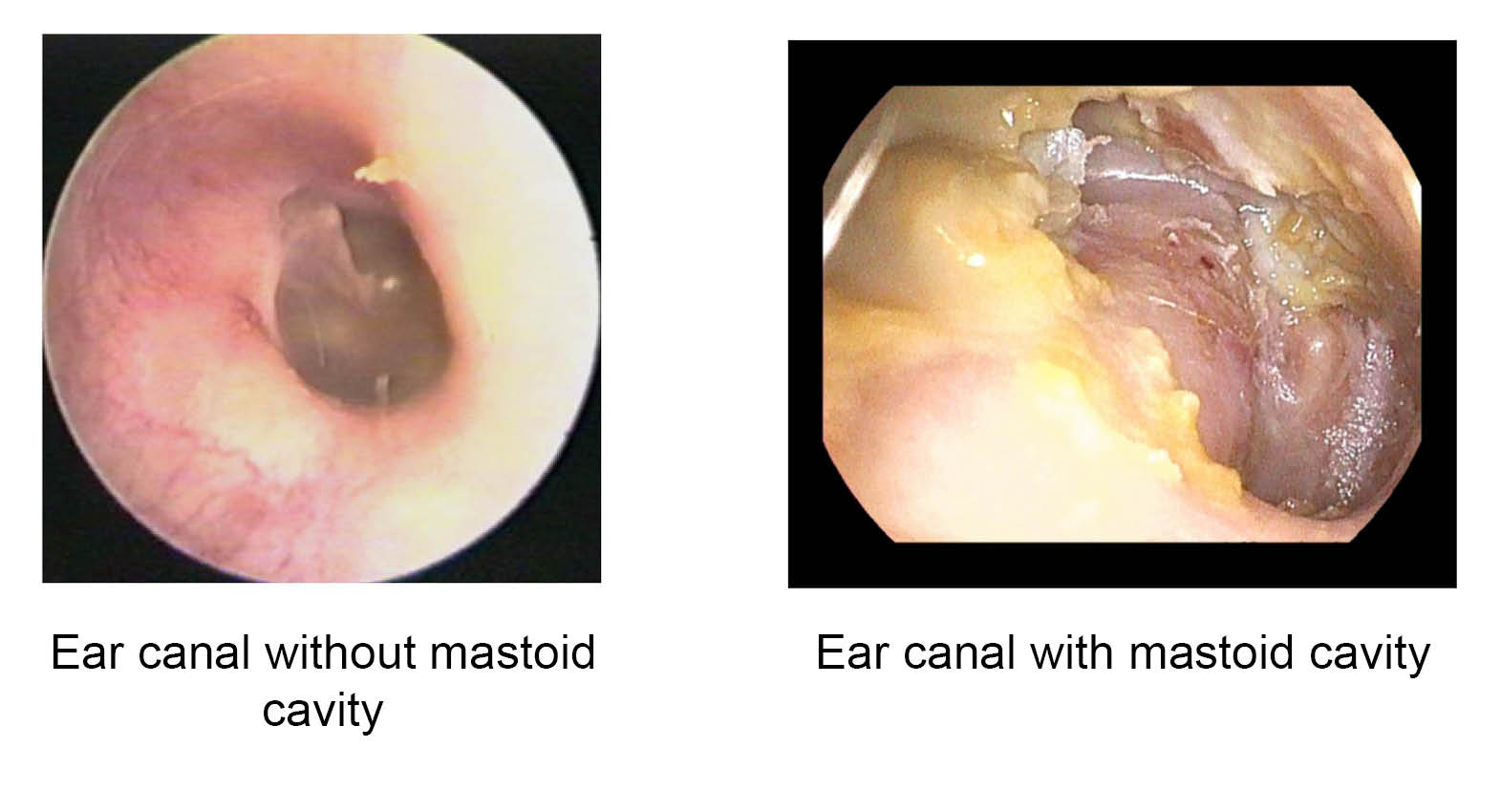
You have previously had surgery to remove one or more of the structures in your ear. This could be your ear drum, ossicles, or part of your mastoid bone. This has resulted in you having a mastoid cavity.
Your surgeon has recommended that you have mastoid obliteration surgery as:
your mastoid cavity is continually discharging, or
it is accumulating dead skin, and
it has not improved with regular cleaning and antibiotic drops.
This surgery aims to remove the disease from your ear. This could be removing the infected tissue or the dead skin, and then reconstructing your ear.
What are the intended benefits of mastoid cavity obliteration?
The main benefit of this procedure is to give you a dry, waterproof, and trouble-free ear.
It may be possible to improve your hearing in your affected ear as well. But this is only if the hearing mechanism of your inner ear is still working. It is not always possible to improve hearing, even when the hearing part of your inner ear still works.
How successful is this procedure?
About 85 in every 100 patients will have a dry, trouble-free ear after this operation.
We also hope to improve your hearing. The success rate of improving your hearing is in the region of 60 in 100 patients.
If surgery does not improve your hearing, a safe dry waterproof ear may allow you to wear a hearing aid. Your surgeon may recommend an alternative hearing solution after your ear has healed.
Who will perform my procedure?
An ear nose and throat (ENT) surgeon will perform your procedure.
What will happen before my procedure?
Most patients attend a Pre-assessment Clinic in the days or weeks before their surgery. At this clinic, you will be seen by a nurse.
They will ask you for details of your medical history.
You will have examinations and investigations. These include checking your blood pressure, pulse, and weight.
Please ask your nurse if you have any questions or concerns about your procedure.
The nurse will ask you what medication you are taking. This includes medication prescribed by your doctor or any over-the-counter medication you take. It helps us if you bring with you details of any medications or supplements you are taking.
If you smoke, stopping before your surgery will help you to heal quicker afterwards. Compared to non-smokers, smokers are more likely to have complications with tissue healing and infections after surgery. For free friendly support and medication to help you stop smoking, contact One You Kent on telephone 03001 231 220.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. More information on consent is available on the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time
Will I have an anaesthetic?
Yes. You will have a general anaesthetic for this procedure (you will be asleep).
Will I have to stay in hospital overnight?
Most people who have this type of procedure can go home on the same day as their surgery. Sometimes we know before your surgery whether you will need to stay for longer than usual. Your doctor will discuss this with you before you decide to have the operation.
Is some of my hair removed before my procedure?
The healthcare team needs to see or reach the skin behind your ear for the operation. They may use an electric hair clipper to remove some of your hair on the day of surgery. The clippers will have a single-use disposable head. Please do not shave your hair yourself, as this can increase your risk of skin infection.
Shower and wash your hair either the night before or on the morning of your operation.
What happens during the operation?
The surgery may take up to five hours.
Once you are asleep, your surgeon will make an incision (cut) behind your ear. They will remove the infected tissues in your mastoid, and any dead skin, to reveal healthy bone. If your surgeon sees any leftover infection, they will clear the infected bone by drilling it away.
Synthetic bone substitute, or your own bone dust or chips is then used to fill the cavity. This is then covered with cartilage and local soft tissue flaps, to help create a healthy ear canal.
Your surgeon will often reconstruct your eardrum using cartilage. Whether they can do this will depend on what structures that are still available and healthy in your ear. Your surgeon will discuss this with you in your clinic appointments. However, it is often impossible to decide if this is an option until during the operation itself. If your surgeon thinks your hearing can be improved, they may replace your ossicle bones with a prosthetic (artificial) ossicle. This will be made of titanium. These prostheses are MRI compatible.
Your ear is then packed with ribbon gauze soaked with antiseptic paste, to keep the graft in place.
Your surgeon will use dissolvable stitches. They will place an adhesive dressing (steri strips) over the stitches to protect them. A cushioning bandage is then placed over the area and kept on overnight. Your surgeon will usually tell you to remove this at home.
Are there alternatives to this procedure?
No. This procedure is the only way to guarantee that you will not have further problems with your mastoid cavity. If you are unfit for this surgery, the only alternative is to have a specialist regularly clean your ear, and to use antibiotic ear drops or creams. At best, this could reduce the discharge.
Are there any risks with this surgery?
There are some risks that you must consider before giving consent to this treatment. You should speak to your surgeon about the chances of any complications in your case.
Scar
You will have a scar behind your ear after surgery. To start with, this will be a red / pink colour but it will fade to a white colour with time and become less noticeable. This scar may be uncomfortable for some time after your operation, often many months. You may have some numbness around the scar, which may or may not improve with time. Sometimes a scar may become larger than immediately after the operation. If this happens you may need another procedure at a later date.
Bleeding
You may have bloodstained discharge from your ear in the weeks following your operation. If the bleeding does not settle, please contact Rotary Ward and ask to speak to the ENT doctor on-call. The contact details are at the end of this leaflet.
Loss of hearing
In a small number of patients, hearing may be made worse due to damage to the inner ear. Hearing in the ear being operated on may be lost completely and permanently.
How should I care for my ear after surgery?
Keep your ear dry for the first few weeks after surgery. Plug it with a cotton wool ball coated with Vaseline when you are having a shower. Do not wash your hair until the ear packing is removed in clinic. Use dry shampoo instead.
Avoid straining / lifting anything heavy for the first two weeks after surgery.
Blow your nose gently.
Avoid air travel for two months.
If possible, avoid diving or flying when you have a cold.
Will I have a follow-up appointment?
You will receive an appointment to return to the clinic four weeks following your operation. This is mainly to remove the packing and check your ear.
We will see you again three months after your surgery. At this appointment, we will check your ear and perform an audiogram. We will discuss any further treatments you may need at this appointment as well.
You will need to come to the ENT Department for your follow-up, for at least five years after your operation. These appointments are usually every year. Your surgeon may also order an MRI scan to check your ear, usually one year after your operation. You may need more MRI scans at a later date.
What if I have any problems or concerns?
If you have any questions or concerns, please call either of the following.
the ENT team on-call at the William Harvey Hospital via the hospital switchboard
Telephone: 01233 633331Rotary Ward, William Harvey Hospital, Ashford
Telephone: 01233 616234.
Ask to speak to either the on-call ENT registrar or nurse practitioner for advice.