Mallet finger or thumb injury
Information for patients from the East Kent Hand Service
This leaflet provides general information about mallet finger injuries to the fingers and thumb. It is not a substitute for your doctor’s advice. This leaflet explains the following.
What a mallet injury is.
How is it diagnosed and what the symptoms are.
What the treatment is for mallet injury.
How to look after your splint.
What the risks and possible complications are.
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please speak your hand therapist.
What is a mallet injury?
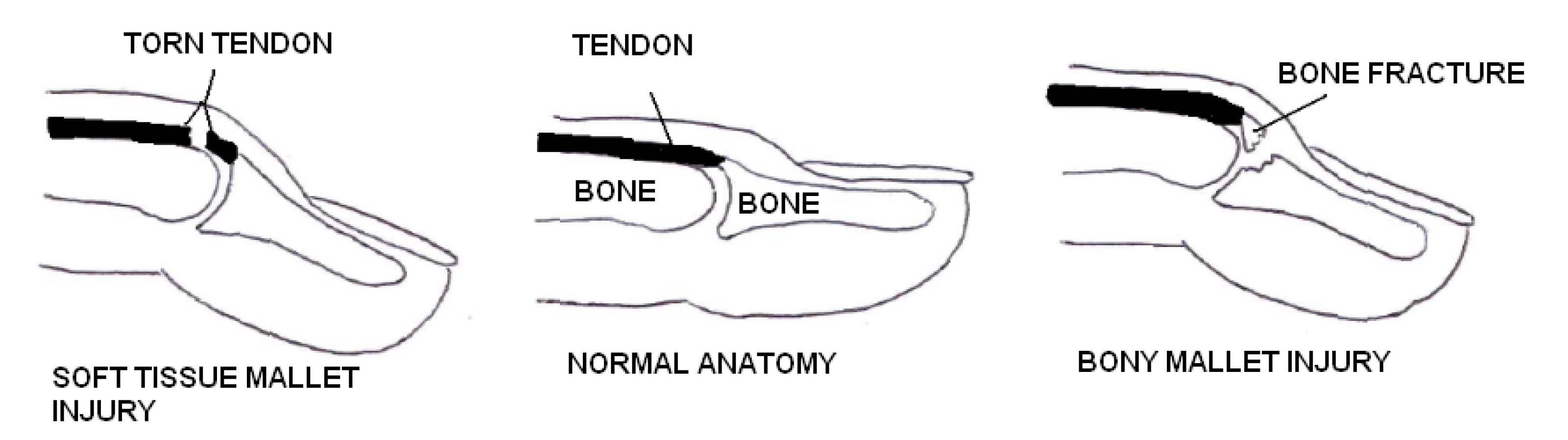
Mallet injury is an injury to the end joint of your finger or thumb. If you have a mallet injury, you are not able to straighten the tip by itself. Although you may still be able to push the joint straight with your other hand. Your finger is always in a bent position. This happens when either:
the tendon that straightens the tip is torn or pulled away from the bone, or
a fracture occurs to the bone where the tendon attaches (see diagrams below).
How is it diagnosed?
Usually a mallet injury is diagnosed by looking at and feeling your finger. Occasionally, an x-ray is taken to see if the bone has been damaged.
What are the symptoms?
Symptoms include:
pain
swelling over the end joint of your finger
the end of your finger lies in a bent position, or
you are not able to hold your finger straight at the end joint.
How is mallet injury treated?
A splint is used to treat most mallet injuries. The splint holds the tip of your finger straight.
A bony mallet injury is where there is a fracture. A splint is worn for 6 weeks.
A soft tissue injury is where the tendon has been pulled off the bone. A splint is worn for 8 weeks.
Your doctor, nurse, or hand therapist will tell you which type of injury you have.
Whilst wearing the splint it is important to continue using your hand normally. Do not let your other finger joints become stiff.
You must wear your splint at all times, both during the day and at night. Only remove your splint for cleaning.
While cleaning it is important not to let your finger bend. If you do, it may slow down your healing and affect how well your treatment works.
What happens if my finger or thumb is not treated?
If your injury is not corrected, the tendon will not heal. You will not be able to straighten the tip of that finger or thumb again.
Are there alternative treatments?
Some patients may need surgery to treat their condition. If you need surgery this will be discussed with your clinician.
How do I look after my splint?
Your splint will either be a ready-made splint or one made for you by a hand therapist.
During your rehabilitation, you will need to remove and reapply your splint from time to time, to clean and dry your finger. When removing your splint, remove the tape and splint without leaving the tip of your finger unsupported. This is best done with your finger resting flat on a table.
Pre-taping your finger

Applying a ready-made splint

Applying a fabricated dorsal splint
A hand therapist may make and fit an individual splint. This is fitted to you in clinic.
-1747837106.jpg)
Place the splint over your pre-taped finger. Make sure the end of your finger is level with the end of the splint. Using one piece of tape, secure the splint onto your finger as shown.
-1728397126.jpg)
.jpg)
After 6 to 8 weeks gradually stop using the splint. Wear it at night and at risk times for another month. Risk times include lifting heavy items or playing sports.
How should I care for my finger and splint?
At least once a day remove the tape from your splint, and remove the splint so you can wash your finger and splint. Remember the end joint of your finger must not bend.
Once dry, reapply your splint following the instructions above.
What problems can happen with splinting?
Swelling in your finger is likely to change regularly (both up and down). This can cause your splint to be either:
too loose and not supporting your finger, or
too tight and uncomfortable.
If this happens, your splint needs to be altered or changed by a clinician.
When you take the splint off for washing, check your finger for red areas where the splint may be rubbing.
The tape may also cause some irritation to your skin. If this happens, change the tape to micropore (paper style tape). Micropore is available at most chemists.
What should I do if my splint becomes loose or painful?
If your splint becomes loose or painful, contact the department who fitted your splint. You may need a different size or a re-mould of your custom made splint.
What are the risks and possible complications?
After the splint is removed, some patients can no longer fully straighten their finger-tip. There is a slight stiffness at the end joint of the finger.
Redness and tenderness of the skin on top of the end joint is common for 3 to 4 months after injury. This usually settles with time. If this becomes a problem, contact the department where your splint was fitted for advice.
Occasionally stiffness may happen in your fingers. This is usually short-term and only occasionally needs therapy.
Compared to non-smokers, smokers are more likely to have complications in tissue healing and infections after injuries or surgery. For free friendly support and medication to help you stop smoking, contact One You Kent.
One You Kent
Telephone: 0300 123 1220
Email
Further information
If you have any questions or problems, please contact the department that treated you.
Exercises after your splint has been removed
Six or 8 weeks after your injury, your therapist will check your healing bone or tendon. At this time, you will need to start exercising your finger or thumb, to increase movement.
You will need to take the splint off your finger to do the exercises shown below.
Please complete the following exercises 4 times a day. Complete each exercise 5 times.
-
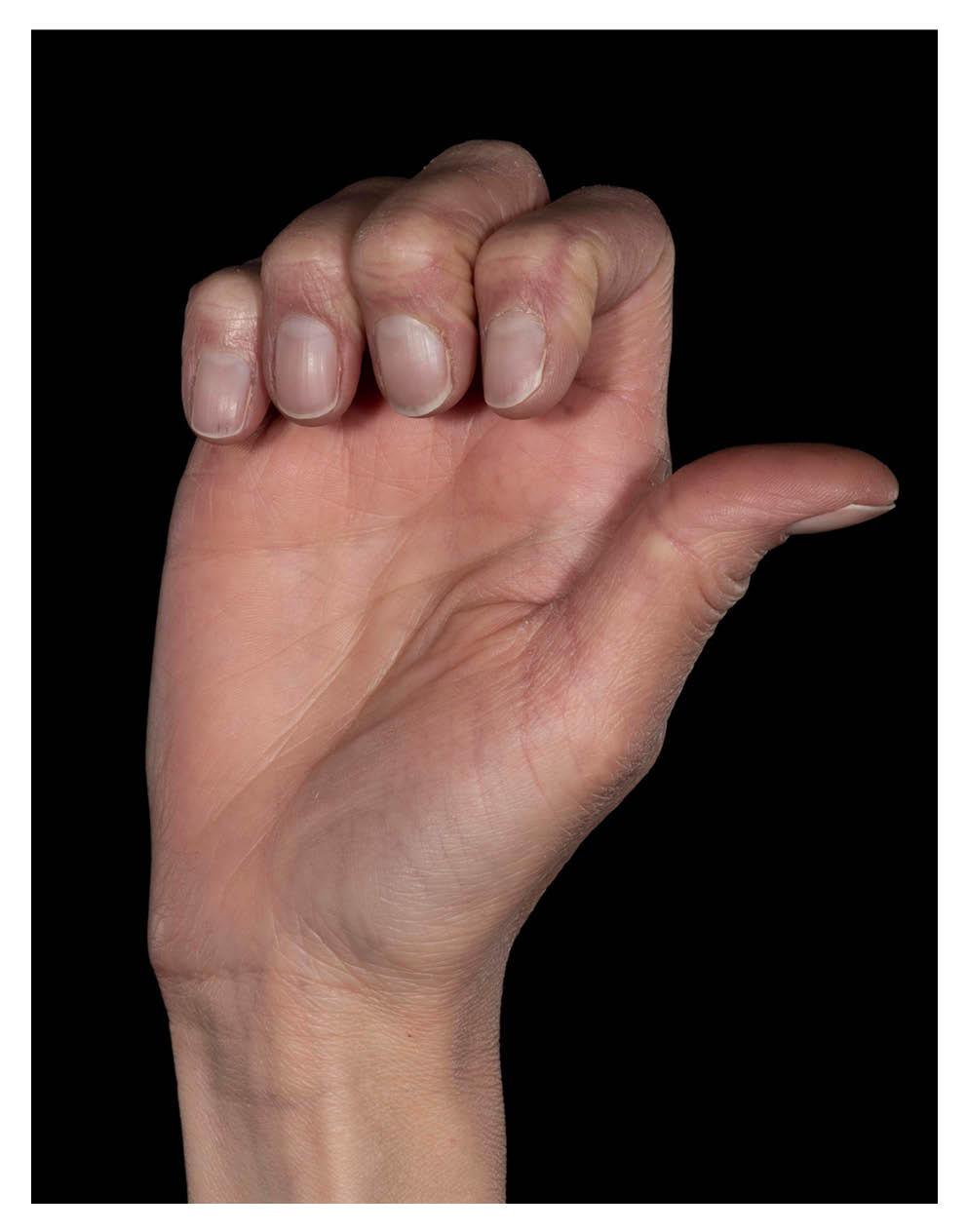 Exercise 1: Hook grip. Bend the top two joints of each finger, using your own muscle power.
Exercise 1: Hook grip. Bend the top two joints of each finger, using your own muscle power. -
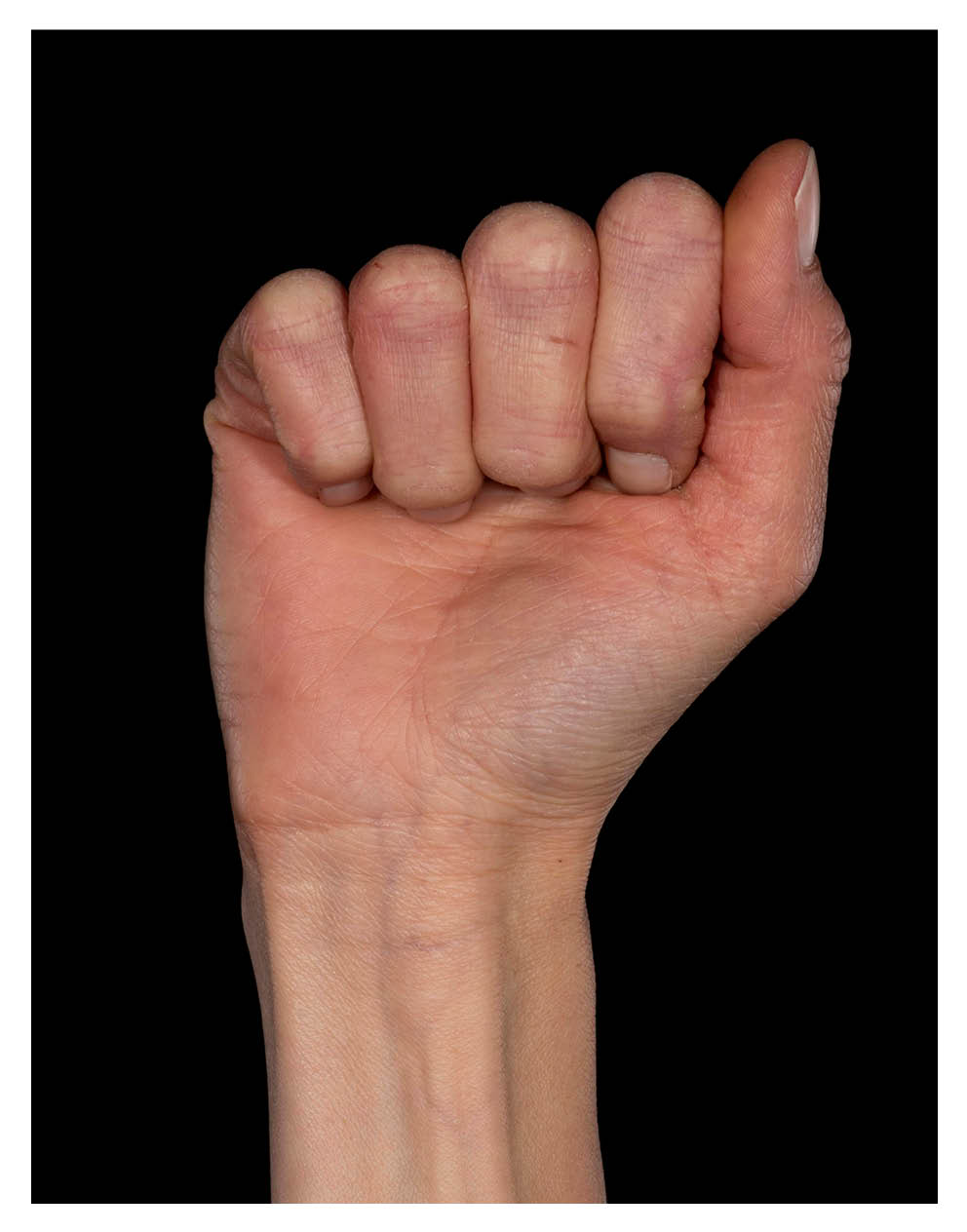 Exercise 2: Full fist. Bend all your finger joints, using your own muscle power.
Exercise 2: Full fist. Bend all your finger joints, using your own muscle power. -
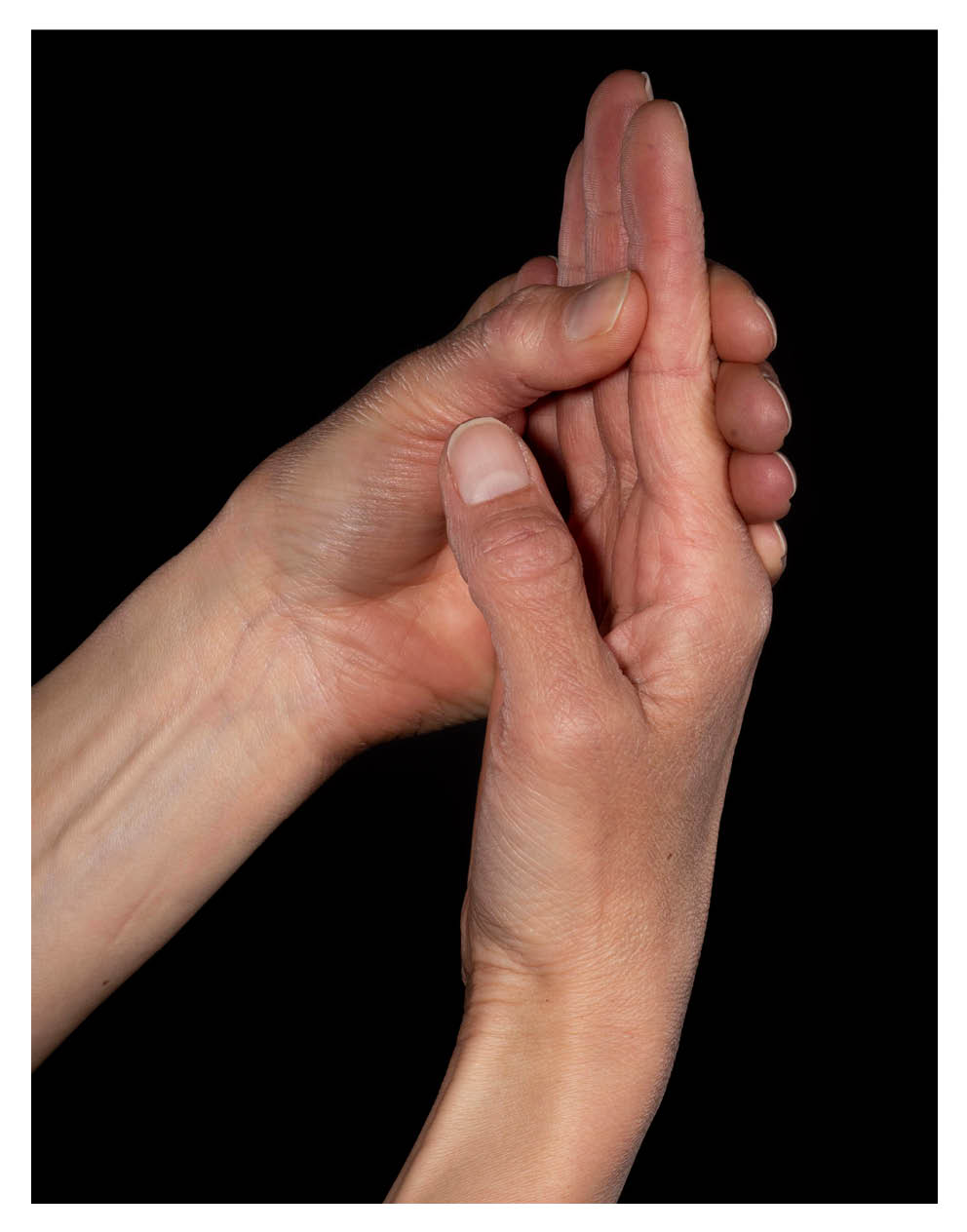 Exercise 3a. Block under the top joint of your finger. Do this by holding the middle joint with your other hand.
Exercise 3a. Block under the top joint of your finger. Do this by holding the middle joint with your other hand. -
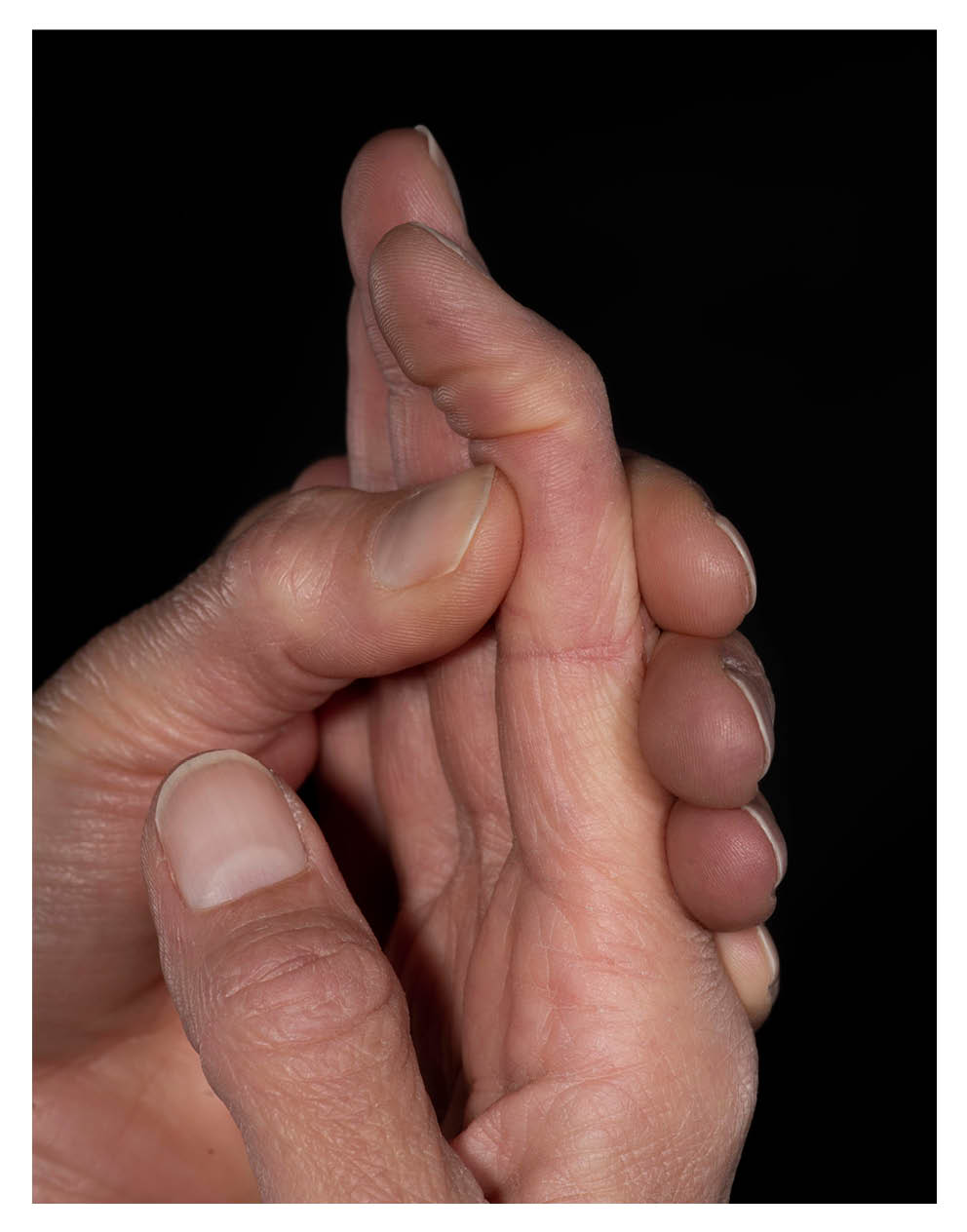 Exercise 3b. Using your own muscle power, bend the tip of your finger. Hold for 2 seconds and then fully straighten the tip. Hold the middle joint firmly during this exercise, to keep it as straight as possible.
Exercise 3b. Using your own muscle power, bend the tip of your finger. Hold for 2 seconds and then fully straighten the tip. Hold the middle joint firmly during this exercise, to keep it as straight as possible.
Do not force your finger to bend.
Do not use your other hand to push it down.
Continue to wear your splint for a further 2 weeks at night in bed and ‘at risk’ times during the day, unless told otherwise by your clinician.
It can take a few months to regain good movement again in your finger tip. It is important to be patient with your recovery.
If you have any problems regaining the movement in your finger tip, please tell your clinician.
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email