Maintaining a healthy bowel when on peritoneal dialysis (PD)
Information for patients from the Home Dialysis Team
This leaflet has been written for people on peritoneal dialysis (PD). It will give you information on how to keep a healthy bowel habit. This is important to help prevent complications.
Constipation is a common condition that affects people of all ages; it is especially common in people having PD. It is really important that you have a bowel motion at least once a day, to allow your peritoneal dialysis to work better.
Although you may have a “normal” bowel movement, this may not be emptying your bowels sufficiently to allow your peritoneal dialysis to work.
What will my PD team do?
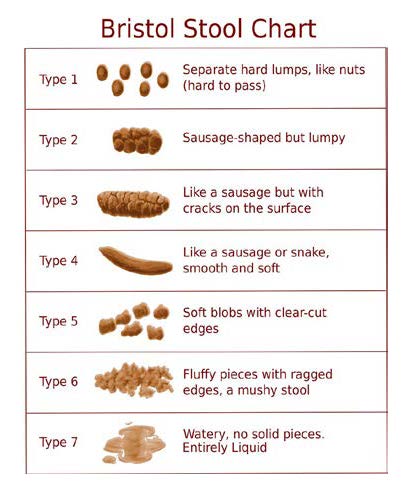
Your PD team will ask you lots of questions about your bowel habits. Do not feel embarrassed about discussing this with them, as it is important you get the right advice. They will use the Bristol Stool Chart to discuss the type of stool you are passing.
What are the symptoms of constipation?
You may have one or more of the following symptoms.
Difficulty in passing bowel motions, which may be abnormally large or small in size.
A feeling that you have not completely emptied your bowel.
Excess wind, bloating, or abdominal (stomach) cramps.
Opening your bowels less than three times a week.
Feeling sick or vomiting, and loss of appetite.
A horrible taste in your mouth.
Watery (overflow) diarrhoea (in severe constipation).
Although you may open your bowels daily, you might only be emptying the lower half of your bowel. The upper part of your bowel might still be full.
How does constipation affect my peritoneal dialysis?
When your bowel becomes full, it can squash or displace your PD catheter, making it difficult to drain the PD fluid out of your abdomen.
If you do not drain the fluid out of your abdomen, you may have lots of low drain alarms on your overnight machine (APD).
If you are on the Homechoice machine it will alarm “low drain volume”, and at the end of your treatment you will have a lost dwell (this is because it has taken longer to drain the fluid from your abdomen). The Homechoice machine does this automatically.
If you are on the Sleepsafe machine you may have an A08 alarm, and your % will be in the 70s or 80s rather than the 90s.
If you are on CAPD (continuous ambulatory peritoneal dialysis), you may find that you are taking a lot longer to drain the fluid out of your abdomen, and you need to stand and wriggle about.
Drain pain could also become more severe when constipated.
Why is constipation a problem?
Severe constipation can cause your PD catheter to move out of your pelvis, to the upper part of the left or right side of your abdomen. This is known as migration or mispositioning of the PD catheter. In severe cases of constipation, it may also cause PD peritonitis (an infection of your abdomen that needs treating with antibiotics).
What causes constipation?
Constipation can be caused by:
A restricted, low fibre diet or a very small diet (not eating enough).
A lack of exercise.
The side effects of some medication (such as phosphate binders, strong painkillers, and iron).
Medical problems (such as high calcium levels, diabetes mellitus, depression, or anxiety).
A restriction on how much fluid you can drink.
PD may also lead to constipation, by drying out your stool as extra fluid is removed during dialysis.
How may I avoid constipation?
Eat a high fibre diet. High fibre foods include wholegrain foods, such as wholemeal rice or pasta and cereals such as bran flakes, shredded wheat, and porridge oats. If you are increasing the amount of fibre you eat, it is important to do this gradually as a sudden increase may make you feel bloated, windy, and give you abdominal cramps.
Eat plenty of vegetables and fruits, as advised by your dietician (some fruit and vegetables have a high amount of potassium).
Exercise (as you are able) can also improve bowel movements. Something like a daily walk can help.
Do not ignore the urge to open your bowels; if you need to have a bowel movement, then do.
When you use the toilet try sitting in a squatting position and leaning forward, so that you are relaxed.
How do I keep a healthy bowel habit when on PD?
You should open your bowels at least once a day, sometimes we may suggest twice a day.
Laxatives
Most people on PD need to take laxatives. These help to soften your stool and move it along your bowel. Your PD nurse will make sure you are prescribed laxatives, and will change the dose if they are not working. You may need to take two or three different laxatives. They work better if taken regularly, rather than when you think you need them.Linseed or flaxseed
Taking linseed or flaxseed (golden or brown) in your diet may also help with constipation. These can be bought from any supermarket. Do not take linseed oil, as this does not work in the same way.
Start with one teaspoon twice a day, and gradually increase to one tablespoon twice a day (take each tablespoon with 150mls of cold water). You can also mix it with foods, such as yoghurt or porridge.
Adding linseed to your diet might increase the number of bowel movements you have each day. It may also cause side effects, such as bloating, flatulence (wind), abdominal pain / cramping, constipation, diarrhoea (where you pass looser or more frequent stools than is normal for you), and feeling sick.Optifibre
Optfibre is a food that is used for special medical purposes. It is a powder that can be added to drinks or food, and does not affect their flavour or texture. It is suitable for people with coeliac disease or an allergy to lactulose.
The dose needs to be increased slowly, starting with one scoop each day until you reach eight scoops per day. Please follow the instructions on the container.
Optifibre is available at many pharmacies, and no prescription is needed.Prescribed laxatives for people on peritoneal dialysis
Senna tablets
Senna contains sennosides, which work by making bowel muscles contract more often and with more force. This increased muscle action moves bowel contents to the rectum.
This medicine usually takes between eight to 12 hours to work.
The usual dose is one to two tablets at night. Your PD team may increase this dose to two tablets twice a day (morning and night), if needed. Do not increase your dose unless you have first spoken to a member of the PD team.
You may notice that your stool or urine is red or yellow in colour, and you may have abdominal cramp-like pains. This is normal, and will stop once the treatment has stopped.
Lactulose
Lactulose is a gentle laxative, that may take up to 48 hours to start working. It is a synthetic sugar that is broken down in the bowel, into products that pull water out of the body into the stool. This softens the stools to make them easier to pass.
If you have diabetes and are taking normal doses of lactulose for constipation, lactulose will have little or no effect on your blood glucose levels.
To start with, take 10mls twice a day. The amount you take can be changed depending on how well you respond to the treatment (up to 45mls each day).
You may have abdominal or cramp-like pain, diarrhoea, flatulence (wind), nausea (feeling sick), and vomiting.
Docusate sodium
Docusate sodium works by making the bowel muscles contract more often and with more force. This increased muscle action moves the bowel contents to the rectum. It also softens the stool and allows water to penetrate dry and hard stools. This softens the stool and makes it easier to pass.
You will need to take one 100mg capsule two or three times a day. If you are still having problems, your PD nurse or kidney doctor may suggest increasing your dose to 200mg in the morning, 100mg at lunchtime, and 200mg in the evening or bedtime.
You may have some abdominal cramps, feel sick, and have diarrhoea. This is normal but if they get worse, please contact your GP. Skin rashes and allergic reactions are rare, but please contact your GP if you have either.
Macrogol (LAXIDO®, MOVICOL®)
Macrogol helps to soften stools by absorbing water. This makes passing the stool more comfortable.
You need to take one sachet, one to three times every day. Mix the sachet with 125mls of water. It can be mixed with squash.
You may get some abdominal bloating, cramps, feel sick, and have flatulence (wind); this is normal.
Picolax (citric acid, magnesium oxide, and sodium picosulfate)
If you are still constipated after trying the routine treatments (such as lactulose and senna, or docusate sodium), or are having problems with your PD, your PD nurse may recommend a single treatment of Picolax. Picolax is a very powerful bowel cleansing agent.
Your PD nurse will give you the Picolax sachets with instructions. Picolax comes in a powder, and needs to be made up into a solution using 150mls of cold water. The mixture will become hot as the powder dissolves, allow it to cool before drinking (this takes around 30 minutes).
Take half to one full sachet, ideally in the morning. Your PD nurse may tell you to take a second dose six to eight hours after your first dose, but if this is after 4pm wait until the following day or you may be up all night using the toilet.
Stop taking your usual laxatives on the day you are taking Picolax and restart the following day.
You may feel sick or bloated, and have abdominal pain (this usually does not last long). Less common side effects include headache, dizziness, and dehydration. Please contact your PD nurse if you think you may be dehydrated.
What if I am still constipated despite these treatments?
If you are still constipated after trying the treatment options listed in this leaflet your PD nurse will talk to you about the next options, as we need to make sure your dialysis treatment is working well. If your PD still is not working well, you will need an abdominal x-ray to check the position of your PD catheter.
If you PD catheter is still not in the correct position or not working well after taking Picolax, you will probably need an operation to move it back into the correct position. If this is necessary, you will discuss this with the PD team before any decisions are made.
Further information
If you would like further information or advice on any of the information covered in this leaflet, please contact your PD nurses.
Home Dialysis (PD) (Monday to Friday, 8am to 4.30pm)
Telephone: 01227 864011 (no urgent messages can be left on the answerphone)Marlowe Ward (out of hours)
Telephone: 01227 783100 or 01227 866456
This leaflet has been produced by the East Kent Hospitals Home Dialysis Team, with help and advice from Dr N Shah Consultant Nephrologist, Mr M Holloway Renal Pharmacist, and Mr R Fleming Renal Dietitian all based on the Oxford Kidney Unit.