Laparoscopy
Information for patients from Women's Health
This leaflet is not meant to replace the information discussed between you and your doctor, but can act as a starting point for such a discussion or as a useful reminder of the key points.
What is a laparoscopy?
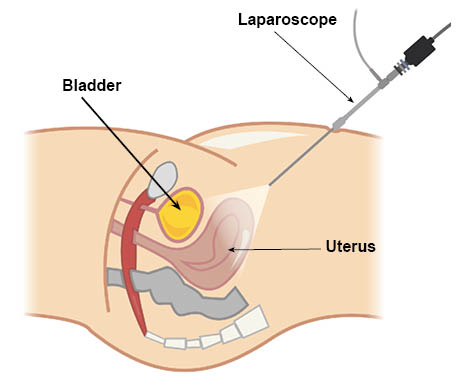
A laparoscopy is a procedure where a small telescope (a laparoscope) is passed through a small incision (cut) underneath the navel (belly button) in order to see the organs in the pelvis (uterus, ovaries, and fallopian tubes). In order to help see these organs, a small amount of carbon dioxide is put through a fine needle into the abdominal cavity (tummy).
How will a laparoscopy help?
Laparoscopy is most often performed as a diagnostic investigation (they will help find out what is wrong), particularly in the investigation of sub fertility or pelvic pain. It can also be done to check the situation if an abnormality has been found on an ultrasound scan.
Some therapeutic operations (treatments) can also be performed with the help of a laparoscope. These will include freeing scar tissue from around the fallopian tubes, treatment of some cases of endometriosis, and uncomplicated ovarian cysts and hysterectomies. Sterilisation is also commonly performed with the help of a laparoscope.
Are there alternatives?
An ultrasound scan may sometimes be performed before a laparoscopy, to help diagnose pelvic problems.
An x-ray, hysterosalpingogram (HSG), can be performed to check whether the fallopian tubes are open or not. However this only gives limited information with regard to the other pelvic organs and also exposes the ovaries to a small dose of radiation. So as a general rule, this investigation is reserved for a small group of women after laparoscopy.
What are the benefits of having a laparoscopy?
A diagnostic laparoscopy and a laparoscopy and dye test are used to look for the cause of bleeding problems or subfertility; they are diagnostic procedures and are not meant to help with symptoms. However, if additional procedures are undertaken (for example diathermy) your symptoms may improve.
Is the treatment safe?
All surgical procedures carry risks.
Occasionally there may be complications causing bleeding or damage to other organs (bladder or bowel). This may mean making a larger incision into the abdomen to repair damage (a laparotomy).
Other possible risks include urinary tract infection and abdominal bruising.
The gas inserted at the time of laparoscopy can cause irritation to the diaphragm (rib cage) and this pain is interpreted by the brain as pain in your shoulder. This phenomenon is called ‘referred pain’ and is a common side effect of the operation. This pain usually stops after 48 hours.
Like all operations, laparoscopy carries a risk of mortality (loss of life). In the case of laparoscopy this is extremely small.
What are the risks?
Serious risks
The overall risk of serious complications from a diagnostic laparoscopy is approximately one in 500 women (uncommon). This includes damage to the bowel, bladder, ureters, uterus, or major blood vessels which would need immediate repair by laparoscopy or laparotomy (open surgery is uncommon). However, in up to 15 in every 100 cases these bowel injuries might not be diagnosed during the laparoscopy.
Your doctor may not be able to enter your abdominal cavity and complete the procedure.
A hernia can develop at the site where the laparoscope enters your abdomen; this happens to less than one in 100 women.
You may have thromboembolic (blood clot) complications; this is rare or very rare.
Although very rare, three to eight in every 100,000 women undergoing a laparoscopy may die as a result of complications.
Frequent risks are usually mild and self-limiting. They may include bruising, shoulder-tip pain, wound gaping, and infection.
What should I do before I come into hospital?
You will be asked to come to the preassessment clinic where a detailed medical history is taken. Blood tests will be performed before your procedure.
Please refer to your appointment letter for any instructions as to what you need to do before you come to hospital, particularly the advice about fasting (eating and drinking) before your procedure.
What will happen when I arrive at the hospital?
On admission to hospital you will be greeted by a member of the ward team, who will discuss with you the care you will receive whilst you are in hospital. You will also be seen by your consultant and / or one of their team. You will be asked to remove make-up, nail varnish, and jewellery.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
Will I have an anaesthetic?
Yes. You will have a general anaesthetic (you will be asleep) for this procedure.
How will I feel after my procedure?
You may feel some pain in your shoulders and abdomen. You will be given pain relief after your procedure. Pain relief can be given in many different ways; in the form of tablets that can be swallowed, an injection, or sometimes in the form of suppositories which can be given via the rectum (the back passage).
You can expect to have two or three small cuts in your abdomen, one in your navel area and the other just above your pubic hair.
You may feel some nausea (sickness) after your anaesthetic, but this is rare.
How long will I be in hospital?
This will depend on the reasons for your operation, or your social circumstances. Many laparoscopies are performed as day cases, although some patients do need to stay in hospital overnight.
What can I expect after my laparoscopy?
Stitches and dressings
Your cuts will be closed with stitches. Most stitches dissolve by themselves in two to three weeks. Other stitches may need to be removed; this is usually done by the practice nurse at your GP surgery about five to seven days after your operation. You will be given information about this before you leave hospital.
To begin with your cuts will be covered with a dressing. You should be able to take this off about 24 hours after your operation and have a wash or shower (see the section on Washing and showering below).Vaginal bleeding
You may get a small amount of vaginal bleeding for 24 to 48 hours after your operation.Pain and discomfort
You can expect some pain and discomfort in your lower abdomen for the first few days after your operation. You may also have some pain in your shoulder. This is a common side effect of the operation. At your preassessment appointment you will be told to buy some over-the-counter painkillers (such as paracetamol) before your operation. Painkillers that contain codeine or dihydrocodeine can make you sleepy, slightly sick, and constipated. If you do need to take these medications, try to eat extra fruit and fibre to reduce your chances of becoming constipated.Starting to eat and drink
If you have had a short general anaesthetic, once you are awake you will be offered a drink of water or cup of tea and something light to eat before you go home.Washing and showering
You should be able to have a shower or bath and remove any dressing 24 hours after your operation. When you first take a shower or bath it is a good idea for someone to be at home with you, to help you if you feel faint or dizzy.
Do not worry about getting your scars wet, just make sure that you pat them dry with clean disposable tissues or let them dry in the air. Keeping scars clean and dry helps healing.
How can I reduce the risk of blood clots forming?
There is a small risk of blood clots forming in the veins of your legs and pelvis (deep vein thrombosis) after any operation. These clots can travel to your lungs (pulmonary embolism), which could be serious. You can reduce the risk of clots by:
moving around (being mobile) as much as you can, as early as you can after your operation; and
doing exercises when you are resting, for example pump each foot up and down briskly for 30 seconds by moving your ankle and moving each foot in a circular motion, or bending and straightening your legs for 30 seconds one leg at a time, three times for each leg.
You may also be given other measures to reduce the risk of a clot developing, particularly if you are overweight or have other health issues. These may include the following.
Daily heparin injections (a blood-thinning agent). You may need to continue having these injections daily when you go home; your doctor will advise you on the length of time you should have these for.
Wearing compression stockings, which should be worn day and night until your movement has improved and you can move around again.
What can help me recover?
A daily routine
Establish a daily routine and keep it up. For example, try to get up at your usual time, have a wash and get dressed, move about and so on. Sleeping in and staying in bed can make you feel depressed. Try to complete your routine and rest later if you need to.
Eat a healthy and balanced diet
Make sure that your body has all the nutrients it needs by eating a healthy balanced diet. A healthy diet is a high fibre diet (fruit, vegetables, wholegrain bread, and cereal) with up to two litres per day of fluid, mainly water.
Remember to eat at least five portions of fruit and vegetables each day. For more information on the importance of eating your 5-A-Day, please go to the NHS Live Well web site.Stop smoking
Stopping smoking will benefit your health in all sorts of ways, such as lessening the risk of a you getting a wound infection or chest problems after your anaesthetic. Even if it is just stop smoking while you recover, you will bring immediate benefits to your health. If you are unable to stop smoking before your operation, you may need to bring nicotine replacements for use during your hospital stay.You will not be able to smoke in hospital.
If you need support to stop smoking you can ask your GP for advice, or contact the Trust’s Stop Smoking Service either through the Trust website, or call 0300 12 31 22 0, or text QUIT to 87 023.A positive outlook
Your attitude towards how you are recovering is an important part of how your body heals and how you feel in yourself. You may want to use your recovery time as a chance to make some longer term positive lifestyle choices, such as:
- starting to exercise regularly if you are not doing so already and gradually building up the levels of exercise that you do; and
- eating a healthy diet. If you are overweight it is best to eat healthily without trying to lose weight for the first couple of weeks after your operation. After that, you may want to lose weight by combining a healthy diet with exercise.
What can slow down my recovery?
It can take longer to recover from a laparoscopy if:
you had health problems before your operation; for example, women with diabetes may heal more slowly and be more likely to get an infection
you smoke - smokers are at increased risk of getting a chest or wound infection during their recovery, and smoking can delay your healing
you were overweight at the time of your operation it can take longer to recover from the effects of the anaesthetic and there is a higher risk of complications such as infection and thrombosis
there were any complications during your operation.
Recovering after an operation is a very personal experience. If you are following all the advice that you have been given but do not think that you are at the stage you should be, talk with your GP.
When can I return to work?
You can usually return to work three to five days after your operation.
Will I have to come back to hospital?
This will depend upon the particular problem troubling you, but usually no.
Getting back to normal
Around the house
While it is important to rest after your operation, you should start some of your normal daily activities as soon as you feel able. You will find you are able to do more as the days pass. If you feel pain, you should try doing a little less for another few days.
Remember to lift correctly by having your feet slightly apart, bending your knees, keeping your back straight, and bracing (tightening or strengthening) your pelvic floor and stomach muscles as you lift. Hold the object close to your body and lift by straightening your knees.
Exercise
The day after your operation you should be able to go for a short 10 to 15 minute walk in the morning and the afternoon, having a rest afterwards if you need to. You should be able to increase your activity levels quite quickly over the first week. There is no evidence that normal physical activity levels are in any way harmful, and a regular and gradual build-up of activity will help your recovery. Most women should be able to walk slowly and steadily for 30 to 60 minutes by the middle of the first week, and will be back to their previous activity levels by the second week.
Swimming is an ideal exercise and, if you have had no additional procedures while in hospital, you can start as soon as you feel comfortable. If you have had other procedures with your laparoscopy, you may need to avoid contact sports and power sports for a few more weeks. This will depend on your levels of fitness before surgery; please discuss this with your doctor.Having sex
It is safe to have sex when you feel ready. If your vagina feels dry, especially if you have had both ovaries removed, try using a lubricant. You can buy this from your local pharmacy.
Travel plans
If you are considering travelling during your recovery, it is helpful to think about whether your:
- travel insurance covers any medical treatment if you have a problem after your operation; and- whether your travel plans are in line with the levels of activity recommended in this leaflet.
If you have concerns about your travel plans including overseas travel, it is important to discuss these with your consultant or GP before you travel.Driving
You should not drive for 24 hours after a general anaesthetic. Each insurance company will have their own conditions for when you are insured to start driving again. Check your policy.
Before you drive you should be:
- free from the sedative effects of any painkillers
- able to sit in the car comfortably and work the controls
- able to wear the seatbelt comfortably
- able to make an emergency stop; and
- able to comfortably look over your shoulder to manoeuvre.
It is a good idea to practise without the keys in the ignition. See whether you can do the movements you would need for an emergency stop and a three-point turn without causing yourself any discomfort or pain. When you are ready to start driving again, build up gradually, starting with a short journey.
When should I ask for medical advice after a laparoscopy?
You should contact Day Surgery or the Women’s Health Suite (see numbers below), your GP, or NHS 111 if you have any of the following symptoms.
Burning and stinging when you pass urine or you pass urine frequently. This may be due to a urine infection and you will be treated with a course of antibiotics.
Red and painful skin around your scars. This may be due to a wound infection and you will be treated with a course of antibiotics.
Increasing abdominal pain. If you also have a temperature (fever), have lost your appetite, and are vomiting, this may be due to damage to your bowel or bladder, in which case you will need to be admitted to hospital again.
A painful, red, swollen, hot leg or difficulty bearing weight on your legs; this may be due to a deep vein thrombosis (DVT). If you have shortness of breath, chest pain, or cough-up blood, it could be a sign that a blood clot has travelled to the lungs (pulmonary embolism). If you have these symptoms, you should ask for medical help immediately.
You should expect a gradual improvement in your symptoms over time. If this is not the case, you should ask for medical advice.
Contact details
Day Surgery, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783114 (open 7:30am to 7pm)Gynaecology Assessment Unit, Queen Elizabeth the Queen Mother Hospital, Margate
Telephone: 01843 235009 (open 24 hours a day)Women’s Health Suite, William Harvey Hospital, Ashford
Telephone: 01233 65 19 87 (open 24 hours a day)