Laparoscopy and dye hydrotubation
Information for patients from Women's Health
You have been referred to the hospital for a laparoscopy and dye hydrotubation. This leaflet will explain the following.
Why you have been referred for this procedure.
What a laparoscopy and dye hydrotubation is.
What happens during the procedure.
Whether there are any alternatives.
What the risks are.
What you can expect afterwards.
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
Why have I been referred for a laparoscopy?
A laparoscopy is often used to diagnose why a patient is having fertility problems or pelvic pain. It helps your doctor see if you have an occlusion / blockage in your fallopian tubes. A blockage could be stopping you from getting pregnant.
What is a laparoscopy and dye hydrotubation?
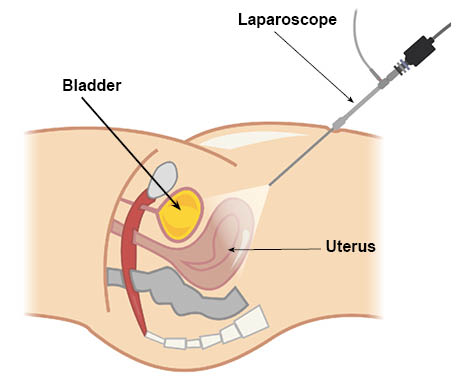
During a laparoscopy, a small telescope (a laparoscope) will pass through a small incision (cut) underneath the navel (belly button). This allows the surgeon to see the organs in the pelvis (uterus, ovaries, and fallopian tubes). To help see these organs, a small amount of carbon dioxide is passed through a fine needle into the abdominal cavity (tummy).
The laparoscope is passed through the little cut. The laparoscope is connected to a video camera and a television, so that the inside of the abdomen (particularly the uterus, fallopian tubes, and ovaries) can be seen on screen. One or two further small cuts are made on the abdomen. The surgeon can then insert narrow instruments to look at the fallopian tubes and ovaries.
If you are having tests to check if your fallopian tubes are open, blue dye is injected through a tube inserted through your vagina and into your cervix (neck of the womb), to see if it spills out at the ends of your fallopian tubes.
It is important that you do not get pregnant before your laparoscopy. Either avoid having sex or use condoms after your last period. If you have had unprotected sex since your last period, your procedure may be cancelled.
It is also important that this procedure is performed during the first half of your menstrual cycle. You will need to contact the waiting list co-ordinator, if your planned admission date does not fall in the first two weeks of your menstrual cycle.
How long will I be in hospital for?
If your surgery is uncomplicated you will be able to go home later that day or the following morning.
Do not drive after your surgery. Arrange for someone to take you home and stay with you overnight.
Will I have an anaesthetic?
Yes. You will have a general anaesthetic, which means you will be asleep during your procedure.
Are there alternatives?
An ultrasound scan may be performed before your laparoscopy.
An x-ray using dye injection procedure called a Hysterosalpingogram (HSG), can be performed to check whether the fallopian tubes are patent. However, this will only give limited information regarding your other pelvic organs.
What are the risks to having this procedure?
All surgical procedures carry risks.
Frequent risks
Failure to diagnose a disease causing your sub-fertility.
Bruising of your abdominal wall.
Infection in the cuts on your abdomen. You may also develop a urine infection.
Shoulder-tip pain. The gas used can cause irritation to the diaphragm. This pain is interpreted by the brain as pain in your shoulder. This is called ‘referred pain’, and is a common side effect of this operation. This pain usually stops after 48 hours.
Perforation of the womb happens in 1 in every 100 laparoscopies. This is where a hole is accidentally made through the wall of your womb. This usually heals itself.
Serious risks
The risk of a patient experiencing a serious complication from a laparoscopy is 2 in every 1000 patients.
Occasionally the operation cannot be completed successfully. This can be due to technical or physical difficulties. For example the telescope cannot get into the abdominal cavity. This means the procedure is stopped.
Damage to your bowel, bladder, ureters (the tubes linking the kidneys to the bladder), or blood vessels. This would need immediate repair by laparoscopy or laparotomy (open surgery is uncommon). However, up to 15 in every 100 bowel injuries might not be diagnosed at the time of the laparoscopy.
Haemorrhage (more bleeding than usual), during or after your procedure.
You may develop a hernia or blood clots after your surgery, but this is rare. If you develop a hernia, you will need to return to theatre.
3 to 8 women in every 100,000 die as a result of complications.
The chance of a complication increases if you:
Are overweight or underweight.
Have had previous surgery.
Have a pre-existing medical condition.
The serious complications increase if other procedures (such as diathermy to endometriosis) are performed.
What should I do before I come into hospital?
You will be asked to come to the hospital's Pre-Assessment Clinic. At this appointment a nurse will take a detailed medical history.
Blood tests may be performed before your operation.
You should check the instructions in your appointment letter. Particularly the advice about fasting (not eating or drinking) before your procedure.
What will happen when I arrive at the hospital for my procedure?
When you arrive at hospital you will be greeted by a member of the ward team. They will discuss with you the care you will receive whilst you are in hospital. You will also be seen by your consultant or one of their team.
You will be asked to remove all make-up, nail varnish, and jewellery.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of:
medical treatment
test; or
examination.
Consent is usually given when you sign the consent form before your treatment. We may ask you to give your consent verbally (spoken rather than written consent).
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. Please speak to staff if:
staff have not given you this information; or
they have but you still have questions.
You must be capable of giving consent. This means you understand the information given to you, and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
What happens after my surgery?
You will wake up in the recovery room, and be taken back to the ward on your bed.
You may have an oxygen mask to help you breathe. This will stay in place until the anaesthetic wears off and you are more awake.
You may have a fluid drip in your arm, until you are able to drink enough fluids on your own.
You can eat and drink as soon as you feel able to.
You can get up and move around the ward, as soon as you feel comfortable.
One of the doctors involved in your operation will come and see you in the ward. They will explain what was found.
You may have some vaginal bleeding. This should not be heavy and should only last a couple of days. Use sanitary towels rather than tampons whilst this bleeding lasts. This will help you avoid the risk of infection.
There may be some blue dye around your genital area; this will wash off.
You will be given a discharge letter. Take this letter to your GP surgery as soon as possible.
How will I feel afterwards?
You may feel some discomfort both in your abdomen and shoulders.
You will be given pain relief after your operation. Pain relief is given in many different ways;
tablets that can be swallowed
an injection; or
sometimes suppositories which can be given via the rectum (the back passage).
Please follow the instructions that come with your painkillers.
Tell us if you feel sick after your anaesthetic. We can give you medication to help with this.
You may find that your genital area has some of the blue dye still present; this will wash off.
Some people may feel emotional or ‘weepy’ during the first few days; this is normal.
You should feel better every day after surgery. However, please contact the hospital urgently if you feel:
increasingly unwell,
have a high fever; or
your pain keeps getting worse.
The hospital contact details are at the end of this leaflet.
Will I have a follow-up appointment?
If you need a review appointment, your doctor will discuss this with you when they visit you on the ward after your surgery. At this review appointment with the Infertility Clinic, we will discuss your results and whether any further tests or treatments are needed.
You will be given a discharge letter to take home. An electronic copy of this letter will be sent to your GP as well.
How do I care for my wounds at home?
You will have two small cuts in your abdomen. One in the navel area and the other just above your pubic hair.
Keep your wounds covered for 24 hours. After 24 hours you can remove the dressing.
You will be given instructions about your stitches. Stitches usually dissolve by themselves. You will be told if you do not have dissolvable stitches, as you will need to make an appointment with your GP practice nurse to have them removed after 3 to 5 days.
Contact your GP if you notice your wounds becoming red, swollen, tender, bleeding, or producing pus or discharge.
Can I drive myself home after my surgery?
No. The effects of the anaesthetic can remain in your body for up to 24 hours. Make sure a responsible adult takes you home, and stays with you overnight in case you feel unwell.
What should I do when I go home?
Do not have a bath / shower the same day as your operation.
You may feel tired, and will probably ache for 48 hours. Try to rest for a few days after your operation.
If you have had a general anaesthetic
Do not undertake strenuous activity for 48 hours.
Do not operate machinery or do anything needing fine coordination or judgement for at least 24 hours, for example using a cooker.
Do not make important decisions or sign important documents.
Do not drive a car, or ride a motorbike or bicycle for 48 hours.
You may eat or drink as you wish; however, your appetite may be poor to begin with.
Do not drink alcohol or take sleeping tablets for at least 24 hours.
When can I return to work?
Do not to return to work until you feel well enough. Depending on your job, this is usually after 3 to 5 days. If you are unsure, please speak to your doctor after your surgery.
What do I do if I feel unwell at home?
If you feel unwell, phone the hospital where you had your surgery.
Canterbury Day Surgery Centre, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783114 (7am to 8pm)Day Surgery, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234499 (Monday to Friday 7am to 9pm)
Telephone: 07887 651162 (Monday to Friday 9pm to 7am) (Bank Holidays and weekends, 24 hours a day)Channel Day Surgery, William Harvey Hospital, Ashford
Telephone: 01233 616263 (24 hours a day, 7 days a week)
Why have has the hospital postponed my appointment?
There is always a risk that your operation may be cancelled at short notice. This is due to either emergency patients who need urgent surgery or other reasons which are beyond our control. We realise that this can cause distress and inconvenience, but if your surgery is postponed, you will be offered a new date as soon as possible.
I need to cancel my appointment, what should I do?
If you cannot keep your appointment, or have been given one that is unsuitable, please change it by phoning the number on your appointment letter. Your call will give someone else the chance to be seen and will help us keep waiting times to a minimum.
References
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email