Laparoscopic sterilisation
Information for patients from Women's Health
You have been given this leaflet as you are considering having a laparoscopic sterilisation. This leaflet explains:
what laparoscopic sterilisation is
how it could help you
what the risks are; and
what will happen before and after your surgery.
We hope the leaflet will help to answer some of the questions you may have. If you have any further questions or concerns, please speak to your doctor.
What is laparoscopic sterilisation?
Laparoscopic sterilisation provides a permanent form of contraception by blocking the fallopian tubes, usually with metal clips. This prevents the egg from the ovaries travelling to the womb (uterus), and prevents the egg and sperm from meeting. This means there will be no fertilisation or resulting pregnancy.
It is a minor surgical procedure performed under a general anaesthetic.
What happens during a laparoscopic sterilisation?
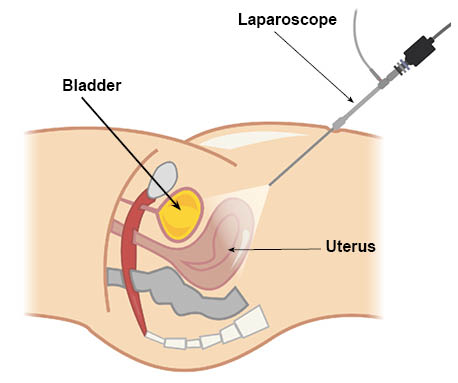
There are two methods used to complete a laparoscopic sterilisation. In both cases you will need an operation where a small telescope (laparoscope) is inserted through a cut in your navel (belly button). Gas is pumped into the abdominal cavity (tummy), so that your doctor can see the organs in your pelvis.
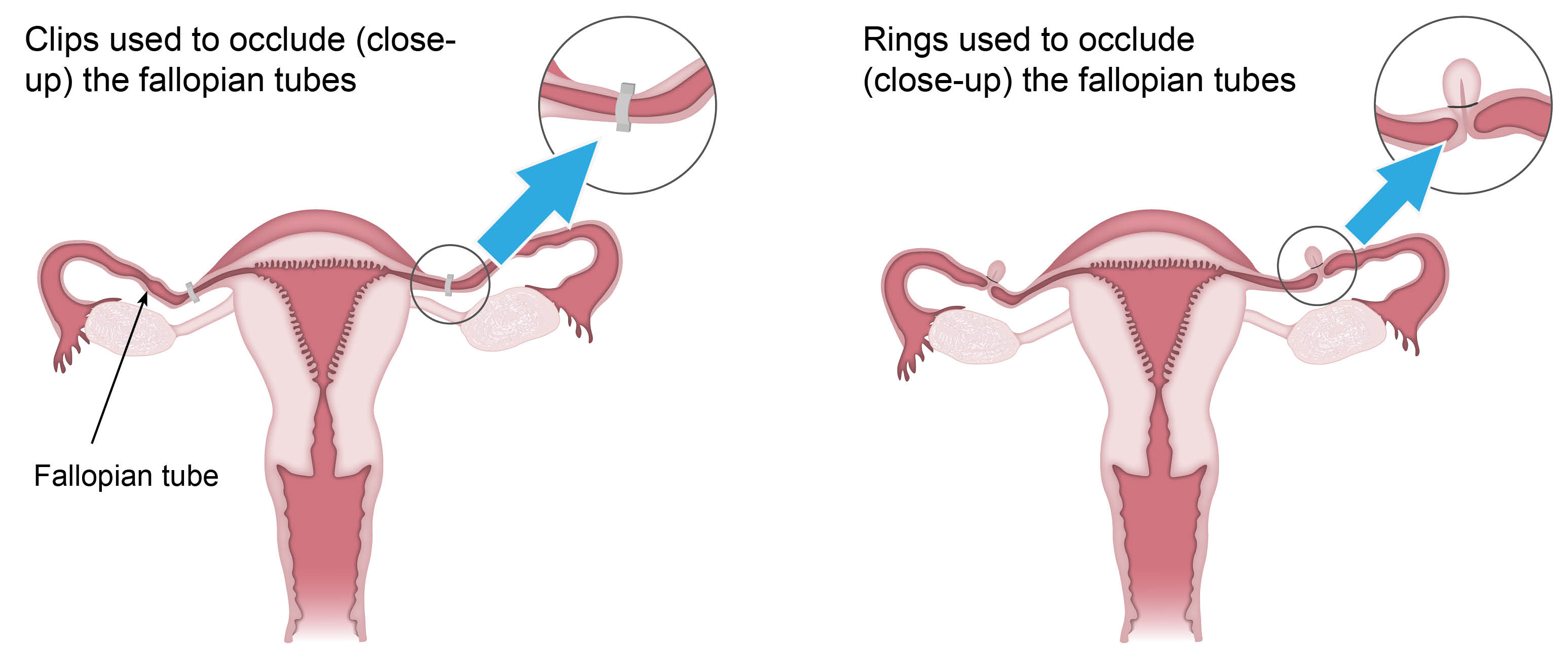
The first method is where one or two clips are added to each tube, to occlude (close up) both fallopian tubes. A ring may be used instead of a clip.
The second method removes the fallopian tubes completely. This is becoming the more common treatment. Research has shown that some ovarian cancers start in the fallopian tubes, and this method may decrease the risk of developing ovarian cancer later.
Are there alternatives?
There are alternative methods of contraception. These will be discussed with you during your outpatient appointment. Some of these methods work well and have the advantage of being reversible.
There are important points to think about before you agree to sterilisation.
The first is that sterilisation has to be regarded as permanent and irreversible. The NHS does not try to reverse sterilisation. It is very important that you are absolutely sure of your decision before choosing this procedure.
Like other methods of contraception, sterilisation can fail. In around one in 200 cases the fallopian tube will re-join. If this happens, you will be at higher risk of having an ectopic pregnancy, which can be a serious condition. An ectopic pregnancy is a pregnancy outside the womb. Therefore, if you ever miss a period following sterilisation, you should complete a urine pregnancy test immediately. If the result is positive, contact your GP. They may arrange for you to have an ultrasound.
Vasectomy is male sterilisation. It is safer and carries a lower failure rate of one in 2,000.
The Mirena IUS (Intra Uterine System) contraceptive coil carries a failure rate of one in 1000. It is a simple and easy treatment. More information is available in the Mirena Coil leaflet.
If you have any questions about the points raised in this section, please speak to your doctor.
Is this treatment safe?
All surgery has risks.
Occasionally, a clip can come free of the fallopian tube. This does not mean that the sterilisation has failed, as there will still be a gap in the fallopian tube where the clip was.
Common risks include bruising of the abdominal wall and shoulder-tip pain.
Serious risks that can happen during surgery
Failure to get the telescope into your abdominal cavity (one in 50 laparoscopies). We will stop your procedure if this happens.
Not able to add the clips to your fallopian tubes. This could be because your doctor's view is hidden by adhesions. We will stop your procedure if this happens.
A hole (perforation) is accidentally made through the wall of the womb during surgery (one in 100 laparoscopies). This usually heals itself.
If damage is done to your bowel, bladder, or blood vessels (one in 1000 laparoscopies) you will need major repair surgery. This is done through a large abdominal incision (laparotomy) and often a blood transfusion. You will need treatment in hospital for several days afterwards.
One woman in 10,000 having a laparoscopy dies as a result of complications.
The chance of a complication increases for patients who:
are overweight
have had previous surgery; and
have pre-existing medical conditions.
Risks following sterilisation
If the procedure is completed using clips, it has a one in 200 lifetime risk of failing, for example you will become pregnant.
If you do get pregnant, it is more likely that you will have an ectopic pregnancy (a pregnancy in the fallopian tube). This can be a life-threatening complication. For more information on ectopic pregnancy, see Are there alternatives? above.
In itself, the procedure is unlikely to change your periods. However, your periods may change if you stop other forms of contraception, such as the pill.
The procedure has to be regarded as irreversible. The NHS does not try to reverse sterilisation.
What should I do before I come into hospital?
You will be asked to come to a Pre-assessment Clinic. You will have blood tests before your surgery.
Please read your appointment letter for instructions. This letter will tell you the fasting times before your operation. Fasting is when you stop eating and drinking before your surgery.
What will happen when I arrive at the hospital?
On admission you will be greeted by a member of the unit team. They will discuss with you the care you will receive whilst you are in hospital. They will ask you to remove make-up, nail varnish, and jewellery.
You will also see your doctor or one of their team. Please use this time to ask any questions, before you sign a consent form.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
Will I have an anaesthetic?
You will have a general anaesthetic for this operation (you will be asleep during the procedure).
How will I feel afterwards?
You can expect to have three small cuts in your abdomen (tummy):
one in your navel (belly button) region
one above your pubic hair; and
a small cut, usually in your right lower abdomen.
You may feel some pain in your abdomen and shoulders. A nurse will give you pain relief after your operation. Pain relief can be given in different ways, including:
tablets, which you can swallow
an injection; or
sometimes as a suppository, which can be given via your rectum (back passage).
Some patients feel emotional or ‘weepy’ for the first few days following their surgery. This is normal.
You may develop a urinary tract infection or sore throat.
Sterilisation after 30 years of age does not make your periods heavier or irregular.
How long will I be in hospital?
This will depend on the reasons for your operation, or your social circumstances. Many patients who have a laparoscopic sterilisation go home the same day. Although some patients do need an overnight stay in hospital.
Will I have a follow-up appointment?
Follow-up appointments are usually with your GP. You will only come back to the hospital if your GP thinks it is necessary.
What should I do when I get home?
You may feel tired. Try to rest for the first 24 hours.
You can eat or drink as you wish, but your appetite may be poor to begin with.
Continue with your normal method of contraception (such as the pill) until your next period starts.
For patients who had a general anaesthetic
For at least 24 hours do not:
do any strenuous activities.
operate machinery or do anything needing fine coordination or judgement, including using a cooker.
make important decisions or sign important documents.
drink alcohol or take sleeping tablets.
You must not drive a car, or ride a motorbike or bicycle for 48 hours.
When can I return to work?
This will depend on what job you do. Usually you can return to work within three to five days following your operation. If you are unsure, please speak to your GP.
What do I do if I feel unwell at home?
If you feel unwell at home or have any concerns, please call one of the following.
Canterbury Day Surgery Centre, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783114 (7:30am to 8pm)
Telephone: 07887 687645 (8pm to 7:30am)Day Surgery, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234499 (7:30am to 8pm)
Telephone: 07887 651162 (8pm to 7:30am)Channel Day Surgery, William Harvey Hospital, Ashford
Telephone: 01233 616263 (24 hours a day, 7 days a week)