Laparoscopic hysterectomy
Information for patients from Women's Health
You have been referred for a laparoscopic hysterectomy. This leaflet explains what a laparoscopic hysterectomy is, what the operation includes, and how you should look after yourself after your surgery.
This leaflet is not meant to replace the information discussed between you and your doctor, but can act as a starting point for such a discussion or as a useful reminder of the key points.
What is a laparoscopic hysterectomy?
There are three main types of hysterectomy.
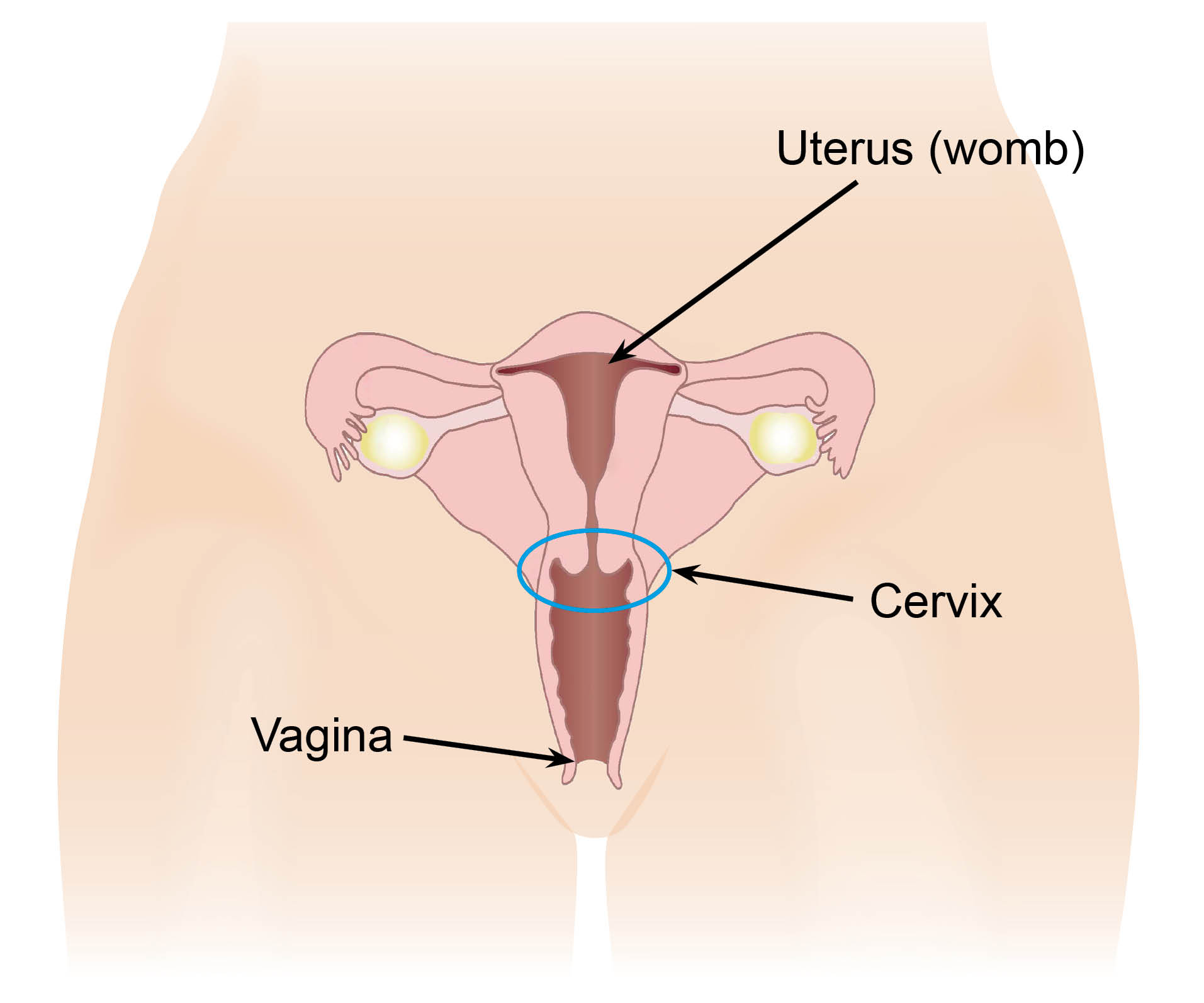
Total hysterectomy includes the removal of the uterus and the cervix (neck of the womb).
Subtotal hysterectomy includes the removal of the uterus leaving the cervix intact.
Hysterectomy plus a salpingo-oopherectomy includes the removal of the uterus and either one or both of the ovaries and fallopian tubes.
A laparoscopic hysterectomy can be carried out entirely by keyhole surgery. However sometimes the surgeon may choose to remove via the vagina (a laparoscopic assisted vaginal hysterectomy (LAVH)).
The type of hysterectomy carried out for you will depend on your personal circumstances and which option is most appropriate for you. You will be able to discuss the type of surgery planned for you with your consultant.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
Will I need a general anaesthetic?
You will usually need a general anaesthetic for your surgery (you will be asleep), however sometimes a spinal anaesthetic can be offered (which numbs the area but you will be awake). You will see an anaesthetist on the day of your surgery to decide which anaesthetic you will have. Please use this time to ask any questions you may have.
How long will I stay in hospital?
You will usually be admitted to hospital on the day of your surgery. If all is well, you will usually be sent home the next day.
How will I feel after my surgery?
You may feel the effects of the general anaesthetic for up to 24 hours after your operation. You may feel drowsy (sleepy), sick, or unable to make decisions during this time.
When you return from surgery you will have a catheter inserted into your bladder; this will usually be removed the next morning. If you have any difficulties passing urine after the catheter is removed, you may need to go home with the catheter for one week to rest your bladder. Arrangements will then be made for you to return to one of our Gynaecological Assessment Units for this to be removed.
If you go home with a catheter, a nurse will teach you how to care for it before you leave hospital. A district nurse referral will also be made, so if you have any problems at home you can contact them through your GP or ring the ward direct (the ward contact details are at the end of this leaflet).
You will have between two and four small incisions (cuts) on various parts of your abdomen (tummy) after your surgery. Each will be up to 1cm long and will most likely have dissolvable stitches in place which dissolve on their own. However, if you have non-dissolvable stitches these will need to be removed five to seven days after surgery; arrangements for this will be discussed with you before you leave hospital.
Dressings will be used to cover your incision sites, which can be removed 24 hours after your operation. Your wounds should heal well with minimal scarring.
If your cervix has been removed, there will be stitches at the top of your vagina. These do not need to be removed and will dissolve on their own; do not be alarmed if you notice part of a stitch discharging from your vagina. You will also have an internal scar at the top of your vagina if your cervix has been removed.
You may have a pack after surgery. This is a length of gauze inserted into your vagina which reduces the risk of bleeding. If you have a pack inserted it can cause a pressure feeling within your vagina and may make you feel like you need to open your bowels. A nurse will remove the pack the morning after your surgery, while you are on the ward. Removing the pack can cause slight discomfort.
Most women will have some vaginal bleeding for up to two weeks after their surgery. It is usually light bleeding similar to a period, and is red or brown in colour. Do not be alarmed if you do not lose blood in the first few days and then have sudden loss days later, this is normal. Sanitary pads should be used, as tampons increase the risk of developing an infection.
It is normal to feel pain and discomfort in your abdomen for a few days after your surgery. While in hospital you can ask your nurse for pain relief, as this will help you to get out of bed and move around. This will help speed up your recovery and help prevent blood clots forming in your legs and lungs.
When you are at home you are advised to take paracetamol and ibuprofen for pain, so please make sure that you have a supply of these at home before you come into hospital. If you need them, you will be given a supply of stronger painkillers such as codeine. Codeine can cause constipation, so make sure you eat a high fibre diet and ask for advice from your GP or ward staff if you become constipated.
A well-known side effect following this surgery is pain in your shoulder, which is caused by trapped air. Walking around and drinking peppermint water can help your discomfort. Tell your nurse if you have trapped wind.
Food and drink will be offered to you as soon as you return to the ward. You may have an intravenous (IV) drip in your arm, this will be removed once you are able to eat and drink again on your own.
You may have a shower or a quick bath the day after your surgery. Dressings need to be removed and left off of your wounds. It is safe for wounds to get wet, but avoid using soap directly on your wounds until they have healed. Following your shower, pat your wound areas dry with a clean towel and keep them clean to prevent infection. Do not reapply the dressing, leave your wound open to the air.
The first few days after your surgery, you may feel more tired than usual, as your body uses a lot of energy to heal itself. Taking a nap during the day can help with this. You may also notice that you feel more emotional, this can be a side effect of what is a stressful unsettling time and is completely normal.
After surgery there is a risk of developing a blood clot or deep vein thrombosis (DVT) to your calf area or pulmonary embolus (PE) in your lungs. To stop this happening you will be prescribed a blood thinning injection called Clexane; which you will need to be injected with each day. You will be shown how to do this yourself, or if you have a friend or relative they can do this for you; if neither is an option please discuss this with your nurse to allow them to make other arrangements.
You will also be given a pair of compression stockings to wear during and following surgery. These will need to be worn day and night until you are able to move around as normal. If you are considered to be at a higher risk of blood clots you may also have a pair of inflatable boots put on your legs to wear while in hospital, these help reduce the risk of clotting.
You can reduce your risks of clots by:
moving around as soon as you are able to, following your operation
carrying out leg exercises every hour when sitting down, such as:
moving each foot in a circular motion for 30 seconds each
pumping each foot up and down for 30 seconds by moving your ankle; and
bending and straightening your legs one at a time, three times on each leg.
For further information, please ask a member of staff for copies of the Trust leaflets Preventing a blood clot whilst you are in hospital, Deep Vein Thrombosis, and / or Pulmonary embolus.
Do I have to take hormone replacement therapy (HRT) following my surgery?
If you have had both of your ovaries removed your consultant may consider it necessary for you to take HRT. This will be discussed with you and you will have a chance to ask any questions before you and your consultant decide whether you need to take it or not.
For more information, please ask a member of staff for a copy of the Trust’s Hormone Replacement Therapy (HRT) leaflet.
Will I still need regular smear tests?
It may be suggested that you will need to continue to have regular smear tests once you have had your hysterectomy. Your consultant will advise you after your surgery whether this will be necessary.
What will happen before the day of my operation?
We recommend that you begin your surgical journey in the best health possible, this includes stopping smoking, losing weight, reducing the amount of alcohol you drink, and increasing your daily exercise.
It is important that all existing medical conditions are well controlled before your operation.
Before you have surgery your health will be checked during a preassessment appointment, and a plan of care for your stay and discharge will be discussed with you. At this appointment please ask any questions you may have about your surgery and care plan, so you are prepared for what lies ahead. Remember you can withdraw your consent for treatment at any time.
Your care plan aims to make your stay in hospital short and allow you to recover better at home. Patients that follow the plan are less likely to have complications after surgery and be readmitted to hospital.
Before surgery you may need to have your bowel completely emptied, which is known as bowel prep. You may be asked to do this at home or in hospital. Bowel prep involves taking two prescribed sachets of powder mixed with a litre of water twice, on the day before your surgery. This will make your bowel open very frequently until there are no more stools left. You will only be allowed to drink clear fluids during this time, however you may also be asked to drink specially made carbohydrate drinks to make sure you keep well hydrated.
What can I do to help myself recover after surgery?
It will take time for your body to recover following a hysterectomy. Everybody heals and recovers differently, but there are some steps you can follow to help with your recovery.
It is important that you rest for the first few days once you are home. The term ‘rest’ does not mean do nothing at all, you need to move around the house and do gentle leg and ankle exercises. Avoid crossing your legs for periods of time.
Your pelvic floor muscles keep your pelvic organs (including your bladder, small bowel, uterus, vagina, and rectum) in their correct position, to stop incontinence. You must exercise your pelvic floor muscles once you have had surgery, even if you have had stitches.
Pelvic floor exercises are done by squeezing the muscles inside your vagina or trying to stop yourself passing wind. You must breathe normally during these exercises, and you can do short or long pelvic exercises.
Short exercises are when you squeeze the pelvic floor muscles for one second and then relax them.
Long exercises are when you squeeze your pelvic floor muscles for several seconds and then release and relax them.
Begin by holding the long squeezes for as long as possible and gently increase them until you are able to hold for 10 seconds. For effective pelvic floor exercises you should do 10 long squeezes followed by 10 short squeezes three times a day.
Straining to open your bowels can also weaken your pelvic muscles and should be avoided.
For more information, please read the Pelvic floor muscle exercises (for women) leaflet.
It is important that you try and keep to your usual daily routine. Get up and have breakfast, shower, and get dressed. Avoid lying in bed as this can cause complications, such as blood clots, and may make you feel depressed.
Make sure your body has all the nutrients it needs for a speedy recovery by eating a healthy balanced diet. Eat a high fibre diet with at least five portions of fruit and vegetables a day along with two litres of fluid, such as a glass of water or squash.
More information on the importance of eating your 5-A-Day, is available from the NHS web site.
Keep your bowels moving. It may take some time for your usual bowel habits to return to normal following your surgery. To begin with you will be given a stool softener or laxative to help you go to the toilet without straining. If passing stools becomes a problem, you should contact your GP for advice.
Stopping smoking will have a big positive impact on your health and wellbeing in general, but it will also reduce your risk of developing a wound infection and chest related issues after anaesthetic. If you need support to stop smoking please contact One You Kent on 03001 231 220, or email.
You may need support from your family and friends whilst you are recovering. This could be support with housework or shopping, or emotional support, where you can talk to them about how you are feeling. If you live alone try and plan ahead by asking a relative or friend if they could stay with you for the first few days. If you have no network of support, please speak to your nurse before you leave hospital.
Having a positive attitude towards your recovery will have benefits for how your body heals and how you feel. Making a change to your exercise and eating a healthy diet could become a positive long-term change to improve your general health. If you are feeling low in mood try and talk things through with someone to make yourself feel more positive.
What will slow down my recovery?
Existing conditions. If you have any health problems before your surgery (such as diabetes) this can slow down your healing and increase your risk of an infection.
Smoking will increase your risk of a chest or wound infection, and slow down healing.
Being overweight can make your recovery from the anaesthetic slower. It also puts you at higher risk of infections and thrombosis.
Some patients will take longer to recover than others, so try not to worry if your recovery seems to be taking a while. If you have any concerns about your recovery, please speak to your GP.
When should I ask for medical advice?
There are health professionals you can speak to if you are worried about anything.
From 9am to 5pm you can contact one of our Gynaecological Assessment Units (GAUs). Out of these hours you can contact one of the wards listed at the end of this leaflet. You can speak with your GP or call NHS 111 out of hours as well.
If you have any of the following signs and symptoms, you should speak to a health professional.
Any signs of a urine infection, such as frequency, burning, stinging, or a bad smell. The most likely treatment for this would be a course of antibiotics.
Vaginal bleeding that is very heavy or smells bad, plus having a fever or generally feeling unwell. This could mean that you have a collection of blood or pus or a haematoma. This can be treated with antibiotics, and you will need blood tests to decide if you take the antibiotics orally or intravenously. If the collection is large and not responding to antibiotics it may need to be drained under ultrasound.
Redness or pain around the incision sites in your abdomen. If any of your incision sites are hot to the touch, or have redness or hardness surrounding them, this can be the sign of a wound infection. This is usually treated with antibiotics. You will need to have a wound swab to decide which antibiotics you will need.
Increasing abdominal pain, including loss of appetite, vomiting, or a fever. This could be a sign of a problem with your bladder or bowels.
Pain, swelling, or hot calf area could be a sign of DVT (a blood clot in the leg), or shortness of breath or chest pain could be a sign of a PE (a blood clot in the lungs). If you have any of these symptoms go to your nearest Emergency Department immediately.
When can I begin my normal activities again?
It is important that you rest and take things easy after your surgery. However, once home you need to begin to get back into a routine and start your usual activities. As the days and weeks pass you will be able to increase the amount you do, but if you feel a pain when you carry out an activity stop for a few days and then try again.
In the first few weeks you could sit to do ironing or prepare dinner, and lift nothing heavier than a litre of water.
For the first four weeks you should avoid lifting anything heavy, including small children, or doing jobs such as hoovering as this can affect how your wound heals. When you do begin lifting things again remember to do so correctly - feet apart, bending your knees and keeping your back straight, tightening your stomach muscles as you lift.
Exercise
Gentle walking is recommended during your recovery. As soon as you get home you should begin taking slow walks, gradually building up the pace and length of your walk. Most women will be able to complete a 30 to 60 minute walk after the first three weeks following surgery.
You can return to exercise (such as swimming) after about two to three weeks.
If you build up gradually you should be able to return to your usual activity level within six weeks.
Contact sports should be avoided for the first six weeks following surgery.
You will not be able to start driving again until you:
have stopped taking any medication which makes you feel sleepy.
can sit comfortably in a car and are able to use all the controls correctly (including doing an emergency stop).
can wear a seat belt without it hurting or feeling uncomfortable.
are able to look around to manoeuvre the car safely.
Check with your insurance company that you are covered to drive after your surgery. It will take approximately two to four weeks following your surgery for you to be able to begin driving again. Before you set out on a journey sit in your car with the engine off and try the movements you will need to use when driving, and see if you can complete them with ease and comfort.
If you are planning to travel during your recovery period it is important to think about the following points.
The length of the journey. If your travel time is four hours or more and you cannot take regular stops to walk about, you could be at increased risk of developing a DVT.
Will the journey cause you discomfort? For example will you be squashed in a car and not able to change position?
If travelling abroad, will your travel insurance cover you if you have had surgery? Will you have access to any medical treatment you might need following any complications with your surgery?
Do the activities you have planned for your trip exceed the time limits discussed above?
If you have any queries about the safety of travelling following your surgery, please ask your GP or consultant for advice.
We recommend that you do not have sex until four to six weeks after your surgery. After this time you should have healed enough. If you feel any discomfort you can wait until it is more comfortable for you. If you have had your ovaries removed during surgery you could have vaginal dryness, which can be helped by using a lubricant which you can buy over-the-counter at your local chemist.
Following your surgery you may feel more tired than usual, so your return to work will depend on how you feel and what you do for a job. Some women will feel fine to return after three weeks but most women will return within four to six weeks.
Returning to work can help your recovery by getting back to your usual routine and spending time with others. It may be possible to return to work to do shorter days or light duties, and then gradually return to your usual working hours. Please discuss this possibility with your employer.
It is your decision when you feel the time is right for you to return to work, do not let anyone make this decision for you. You will be given a sick note when you are discharged from hospital, and if you feel you need longer you can discuss this with your GP.
Contact details
If you have any questions or concerns about your surgery or recovery, please contact one of the following.
Birchington Ward, Queen Elizabeth the Queen Mother Hospital, Margate
Telephone: 01843 234201Gynaecological Assessment Unit, Queen Elizabeth the Queen Mother Hospital, Margate
Telephone: 01843 235009Women’s Health Suite, William Harvey Hospital, Ashford
Telephone: 01233 616107Gynaecological Assessment Unit, William Harvey Hospital, Ashford
Telephone: 01233 651987