Inhibitors
Information for patients and carers from the Haemophilia Centre
What is an inhibitor?
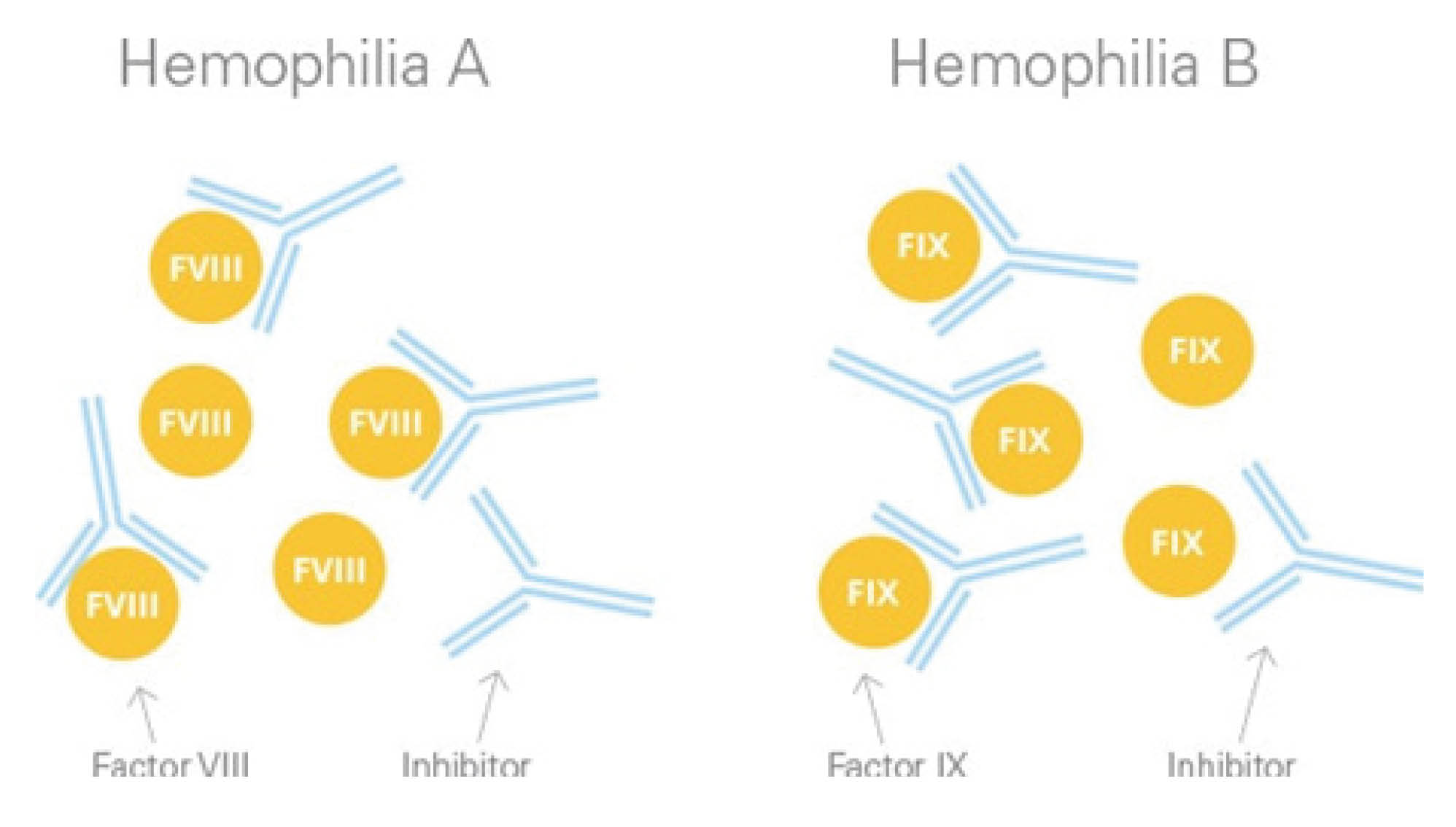
An inhibitor is a type of antibody (or protein) in the blood that prevents factor replacement treatment from working. Antibodies are made by our own immune system to destroy something in our body it thinks should not be there.
In haemophilia, if an inhibitor develops, the immune system thinks Factor VIII should not be there. Therefore the clotting factor treatment does not work, because as soon as we give treatment the immune system destroys it. This makes bleeding episodes more difficult to treat.
How common are inhibitors?
For children with severe haemophilia A, about three in 10 will develop inhibitors. Inhibitors in severe haemophilia B however, are much rarer.
Most inhibitors are low level and can be easily treated with continued Factor VIII or Factor IX. Known risk factors in the development of inhibitors include:
a family history of inhibitors
ethnic background
the number of days treated with clotting factor; and
the type of mutation causing your haemophilia.
How do you know if my child has an inhibitor?
Part of our routine care will be to check for the presence of an inhibitor. Usually this is done when your child is being given their treatment. A small amount of blood will be taken when we put in the needle to give the factor treatment. This is done more often when your child first starts needing treatment, because we know the risk of developing an inhibitor is much higher between the 5th and 50th treatment that is given.
After that, we check for an inhibitor before each appointment and at other times if we are concerned.
What will happen if my child does develop an inhibitor?
There are two issues to deal with when an inhibitor is detected.
Treatment of acute bleeding episodes
Because the inhibitor stops the Factor VIII from working, different products are used for haemophilia patients with inhibitors. These products aim to bypass the inhibitor and allow the blood to clot. The two products used most commonly are FEIBA and Recombinant Factor VIIa. Both these treatments are given intravenously through a needle in the skin or through a portacath, similar to the way we give standard clotting Factors VIII and IX (see separate information sheet Implantable port (portacath or port) for more information). The Haemophilia Centre doctors and nurses will advise you on the best treatment in your child’s case.
To eradicate (get rid of) the inhibitor
In the long-term, it is better if we can “get rid” of the inhibitor and allow treatment with Factor VIII or Factor IX to continue as before. This process is called immune tolerance and aims to reset the immune system to recognise the clotting factor, as part of the normal body. This involves giving larger doses of Factor VIII regularly in order to make the immune system tolerant of the clotting factor.
There are also a number of newer therapies for patients with inhibitors that appear very promising. The Haemophilia Centre staff will keep you updated on these.
Are all inhibitors the same?
No, inhibitors are not all the same. We measure the level of the inhibitor that is in your blood; this is known as a titre.
There are two types of inhibitor: low titre inhibitor and high titre inhibitor. We measure the inhibitor in what is called Bethesda Units: a low titre inhibitor (low strength) measures less than five Bethesda Units, whilst a high titre inhibitor (high strength) measures higher than five Units.
Once we find an inhibitor, the way it responds to ongoing treatment with Factor VIII or IX determines whether it is:
a low responding inhibitor, that remains at low levels despite continuing factor treatment; or
a high responding inhibitor, where the inhibitor level rises in response to continuing factor therapy.
This information helps us decide the most appropriate way to treat the inhibitor and any bleeding episodes.
Is there anything we need to look out for?
It is important to contact the Haemophilia Centre for advice if you have any concerns.
In particular, bleeding episodes need to be treated quickly. The Haemophilia Centre should be contacted if you have any concerns about bleeding.
It can be a very stressful time for you and your family, so it is vital to contact staff here in the Haemophilia Centre for support and for any more information you may need.
Contacting the Haemophilia Centre
Non urgent and routine enquiries (we will aim to get back to you by the end of the following working day).
Telephone: 01227 783157
EmailEmergency number to be used for urgent clinical issues.
Telephone: 01227 783166 (Monday to Friday excluding Bank Holidays, 8.30am to 5pm)
Telephone: 01227 783190 (out of hours) and ask for the consultant on-call for haemophilia.