Idiopathic intracranial hypertension (IIH)
Information for patients from the Neurology Department
This leaflet is for patients already diagnosed with, and also those being investigated for IIH. The leaflet will explain the following.
What idiopathic intracranial hypertension (IIH) is.
What causes the condition, and what the symptoms are.
How we diagnose the condition.
The best ways of managing the condition.
What health professionals may be involved in your care.
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
What is idiopathic intracranial hypertension (IIH)? How common is it?
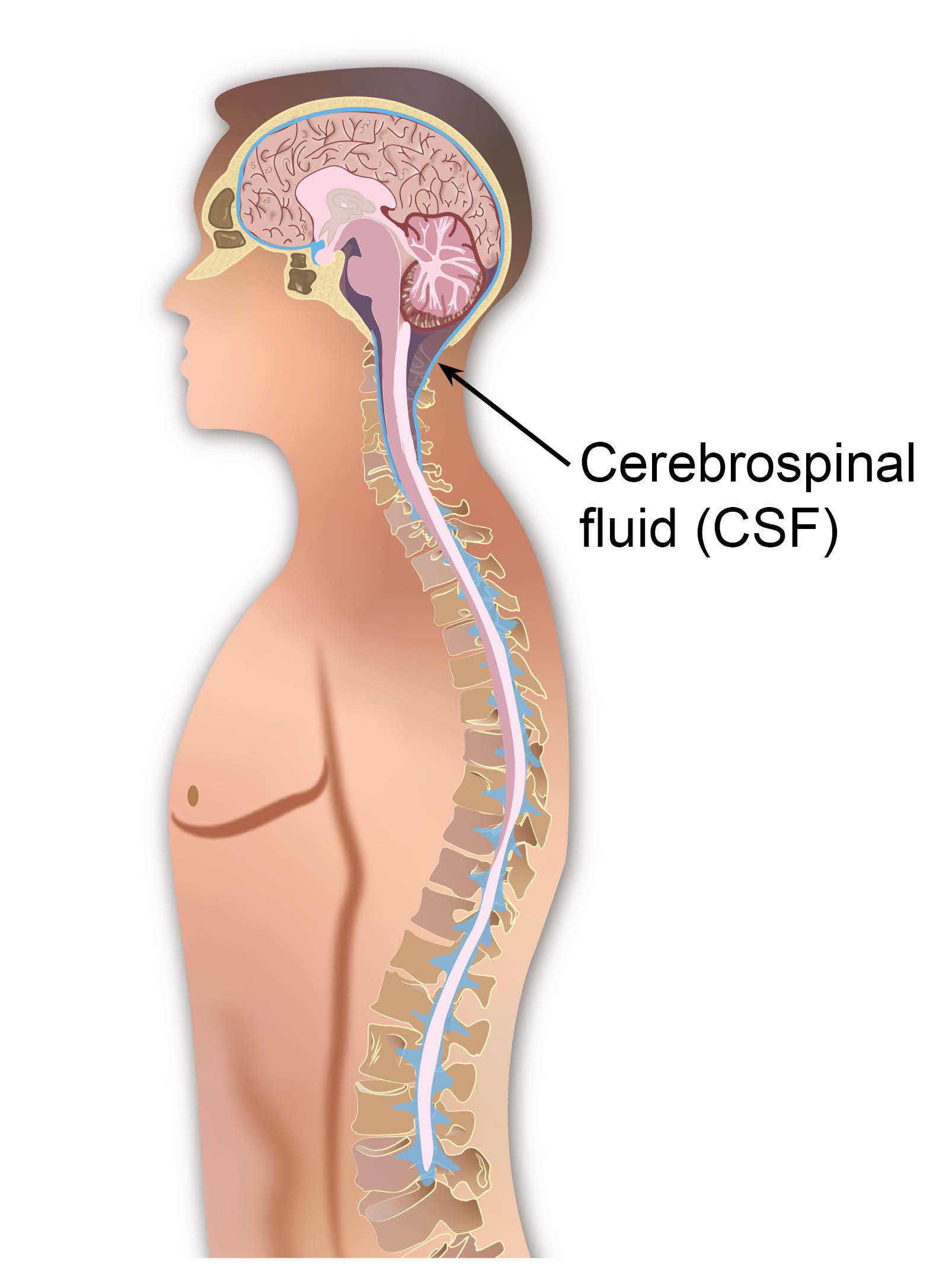
IIH is a neurological condition. It is caused by an increase in pressure in the fluid that surrounds the brain. This fluid is called cerebrospinal fluid (CSF). CSF bathes the brain, some of your nerves, and your spinal cord.
When the pressure gets too high it can affect the nerves. The nerves supply your eyes and it can cause headaches.
IIH affects approximately 2 to 3 people in every 100,000.
The number of cases diagnosed each year is increasing.
What causes IIH?
The medical term ‘idiopathic’ means that the exact cause is not clear. However, certain things are known to increase your risk of developing the condition, including the following.
Weight gain is often the trigger in susceptible people. Especially those who are already overweight or obese.
Obesity (where your BMI is greater than 30) has been shown to be the biggest cause of IIH. Approximately 9 in every 10 patients diagnosed with IIH are obese.
IIH most commonly affects women in their 20s and 30s.
Taking certain medications can increase your chance of developing IIH. These include:
the combined oral contraceptive pill
tetracycline antibiotics
an overdose, or more than your recommended dosage of vitamin A; and
anabolic steroids.
Patients diagnosed with hormonal problems are more likely to develop IIH. Hormonal problems can include Cushing’s syndrome and hypothyroidism.
A blood clot in the veins draining CSF from the brain (venous sinus thrombosis) can mimic IIH. We will rule out this condition by arranging an MRI scan before we diagnose you.
What are the symptoms of IIH?
Common symptoms include the following.
Headaches are the most common symptom.
Double vision (also known as diplopia).
Temporary loss of vision in one or both eyes. Especially when doing activities that increase CSF pressure. Activities including bending over, straining, and coughing.
Blurred vision.
Whooshing noise in your ears, in time with your heartbeat (pulsatile tinnitus).
Rarer symptoms can include the following.
Aversion (dislike) to light, called photophobia.
Loss of peripheral vision, where you cannot see things you are not looking directly at.
Decreased depth perception, where you lose some ability to judge the distance between objects.
Nausea (feeling sick) and vomiting.
Fatigue (extreme tiredness).
Back pain.
Sometimes there are no symptoms, but your optician can pick up papilloedema (swelling of the optic disc) at a routine check-up.
How is IIH diagnosed?
If we think that you have IIH we will usually carry out the following tests. The tests help make a diagnosis and rule out other conditions that have similar symptoms.

A physical examination. This will involve using an ophthalmoscope to look in the back of your eyes. We will check for swelling around the optic nerves (known as papilloedema). If you have not already had one, you may have a more detailed assessment of your eye with an ophthalmologist.
A general examination of your body, to look for other causes of high pressure. We will record your height and weight, so we can calculate your body mass index (BMI). We will check your weight at your follow-up appointments.
We will use visual testing to check how clear your vision is.
CT and MRI brain scans will help rule out other causes of your symptoms, and help confirm your diagnosis.
A lumbar puncture is the only test which can physically confirm whether the CSF is under high pressure. For more information, ask a member of staff for a copy of the Trust’s Lumbar puncture (adult) leaflet.
What is the recommended treatment?
Before any treatment begins, your doctor will discuss each of the following options with you. If you have any questions about any of the following, please speak to your doctor. Weight loss along with one medication is what we usually recommend.
Weight loss
The most important and successful treatment for IIH is weight loss. Research has shown that weight loss in IIH leads to:
a reduction in pressure, and
reduces symptoms, such as headaches and visual changes.
The amount of weight you need to lose to stop symptoms is not yet known. Research suggests that a target of 15% weight loss can help to resolve papilloedema linked with IIH and preserve eyesight. Your doctor will discuss your target weight loss with you in clinic.
If you lose enough weight, your symptoms may improve and you will not need to take medication. However, if you put the weight on again IIH can return.
Even if your CSF pressure normalises with weight loss or medication, you may still have headaches. Your neurologist will manage these headaches differently.
Medication
Acetazolamide
The most commonly used medication in IIH is acetazolamide (Diamox). This is a water tablet that works by reducing the amount of CSF you produce.
Side effects include:
diarrhoea (poo is loose / runny and watery)
changes to your taste
fatigue (extreme tiredness)
nausea (feeling sick)
paraesthesia (pin and needles)
tinnitus (a ringing sound in your ears)
vomiting
depression, and
rarely kidney stones.
We will increase your dose slowly to reduce these side effects.
Avoid taking acetazolamide during pregnancy. Especially the first 12 weeks of pregnancy, as it may harm your baby. If you plan to become pregnant, tell your neurologist.
Topiramate
Another less commonly used tablet is topiramate, which acts in a similar way to acetazolamide.
There is a new government rule for prescribing topiramate in women with child bearing potential. The rule limits the use of this medicine, unless you are on a definitive pregnancy prevention. For more information, please go to the UK government web site.
Pins and needles, reduced appetite, and low mood are the most common side effects. You may also feel drowsy and have reduced concentration. Some people can have a stomach upset. Topiramate can reduce the effectiveness of hormonal contraceptives (including the pill).
Avoid taking topiramate during pregnancy. There is an increased risk of major congenital malformations, such as cleft palate, during the first 12 weeks of pregnancy. If you plan to become pregnant, tell your neurologist.
Painkilling medications
Wherever possible do not take regular painkillers (such as paracetamol or ibuprofen). These can cause another type of headache called medication overuse headache. If you do need to take these painkillers, try to only take them for 10 days or less each month. Avoid strong opioid medications, such as tramadol and morphine.
Lumbar puncture
In the past, we have used repeated lumbar punctures therapeutically to try and control IIH. However, recent evidence no longer supports this. It shows the rate of production of CSF leads to the CSF pressure returning to its previous level within a few hours of having a lumbar puncture. The current recommendation is that lumbar puncture should only be routinely used to diagnose IIH.
In rare cases, we may perform a therapeutic lumbar puncture as a holding measure. However, only for patients with serious visual loss, who are awaiting surgery within the next few days.
Surgery
If you have severe IIH with visual problems and the above treatments have not worked, we may consider surgery to protect your vision. The most common procedures are those which divert (redirect) and drain the CSF, these are called ‘shunts’ and include the following.
Subcutaneous lumbar drain is a temporary measure. We place a plastic tube in your lower back, using local anaesthetic. The anaesthetic numbs the area, and you are awake for the procedure. This drain is sometimes used whilst planning a permanent shunt procedure.
Lumbo-peritoneal (LP) shunt is a permanent plastic tube inserted into:
the spinal subarachnoid space at one end, and
into a cavity in the abdomen called the peritoneum at the other end.
Ventriculoperitoneal (VP) shunt is a tube placed from the CSF containing chamber in the brain, called the lateral ventricle. The shunt goes down through the neck into the peritoneal cavity in the abdomen.
Optic nerve sheath fenestration is an alternative procedure. It is used to reduce the swelling of the optic nerves, whilst you lose weight. A small window is cut into the optic nerve sheath. The optic nerve sheath is a layer of fibrous tissue surrounding the optic nerve. This procedure carries the risk of blindness, so is only used in those who are severely affected by visual loss in IIH.
Shunt surgery can provide successful long-term relief from IIH symptoms. However, the procedures listed above do have risks, including:
malfunction (the shunt does not work)
infection, and
kinking, blockages, and over-draining of the shunts.
Shunt repair surgery is often needed.
What health professionals may be involved in my care?
Acute physicians are the doctors working in the Emergency Department and Acute Medical Units. They will often be the first people you come in to contact with in the hospital.
Neurologists are doctors who specialise in the care of the nervous system. They will be the specialist who takes ownership of your care, once you have been seen in clinic.
Ophthalmologists are doctors who specialise in the care of your eyes. Neurology will refer you to an ophthalmologist for regular visual field assessments. These assessments will monitor your vision for any impairment.
Dietitians are health professionals who specialise in dietary advice and help with weight loss.
Neurosurgeons are doctors who specialise in surgery of the nervous system.
What are the risks of IIH?
Visual loss is the most worrying risk. If left untreated IIH can lead to permanent loss of vision. If there is any concern that your vision has got worse, please contact your GP for urgent medical advice.
Does IIH get worse during pregnancy?
The effects of pregnancy on IIH vary from one person to another. Some have had improvement in their IIH symptoms when they are pregnant, and worsening of symptoms after childbirth.
Will I have regular follow-up appointments?
This will depend on how bad your condition is. Your doctor will discuss this with you at your clinic appointment.
What if I have any questions or concerns?
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
Further information
References
[Web sites last accessed 19th November 2025]
We have used the term ‘women’ in this leaflet. When we use this term we also mean people with female reproductive organs who do not identify as a woman. East Kent Hospitals is committed to supporting people of all gender identities. Please tell your midwife or doctor how you would like them to address you, so we can be sure to get this right.
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email