Hysteroscopy
Information for patients from Women's Health
What is a hysteroscopy?
A hysteroscopy is a procedure for looking inside the uterus (womb). It is carried out using a hysteroscope. This is a small camera that is passed through the vagina and cervix, to see inside the uterus.
How will a hysteroscopy help?
A hysteroscopy is performed to help in the diagnosis of:
heavy or irregular periods
bleeding between periods
post menopausal bleeding, and
in some cases of repeated miscarriage.
If needed, a biopsy of the lining of the womb can be taken during a hysteroscopy. A hysteroscopy is also used in certain treatments of menstrual problems, such as the removal of polyps / fibroids and endometrial ablation.
Are there alternatives?
An ultrasound scan is usually carried out before a hysteroscopy. However, the view of the inside of the uterus is not as clear as it is with a hysteroscope.
Is the treatment safe?
A hysteroscopy is a minor procedure, and is relatively free of problems.
You can expect to have some vaginal bleeding for up to a week after your procedure. Use sanitary towels rather than tampons during this time, to prevent infection.
There is a low risk of infection. If you get an infection you may have increased vaginal bleeding and / or an offensive smelling discharge. If this happens you will need a course of antibiotics from your GP.
The uterus can be perforated (pierced) by the hysteroscope itself. If this happens, the perforation will heal on its own. You may be prescribed a course of antibiotics as a precaution, and very rarely you may have to stay in hospital overnight. A perforation is rare, and happens to less than one in every 1000 patients.
Where is the hysteroscopy performed? and, will I have an anaesthetic?
A hysteroscopy can be performed as:
an outpatient with or without local anaesthetic (you are awake but the area is numbed), or
as an inpatient in the Day Surgery Unit under general anaesthetic (you will be asleep).
What are the advantages to having the hysteroscopy as an outpatient?
There are no unwanted side effects of having a general anaesthetic. For more information on general anaesthetic, see the Royal College of Anaesthetists You and Your Anaesthetic leaflet.
You can speak with the hysteroscopist during and immediately after your procedure.
You will be able to go home soon after your procedure, with a plan for future treatment as needed.
Outpatient hysteroscopy is suitable for most patients, but you and your doctor will decide whether it is appropriate for you.
What should I do before I come into hospital?
If you are having your procedure as an outpatient, it is sensible but not essential to bring someone with you to your appointment, so that you do not have to drive yourself home.
If you feel nervous, speak to your GP before your procedure to discuss your concerns.
If you plan to have your hysteroscopy under a general anaesthetic, you may be asked to come to a Pre-assessment Clinic before the day of your hysteroscopy.
Please read your appointment letter for instructions on what to do before your operation, particularly about fasting (not eating or drinking) before your surgery.
What will happen when I arrive at the hospital?
You may have a blood test or be asked for a urine sample before your procedure.
The hysteroscopist (doctor or specially trained nurse who performs the procedure) will discuss with you the procedure and possible treatments available. These can include a biopsy, removal of polyps or fibroids, endometrial ablation and insertion of a hormonal coil (Mirena), if this is considered the best option at the time. It is unlikely all of these treatments will be needed.
The hysteroscopist will then ask you to sign a consent form. If you do not understand something on the consent form or have any last minute questions, please ask the hysteroscopist. This is the same whether you are having your hysteroscopy as an outpatient or under a general anaesthetic. Remember you can withdraw your consent for treatment at any time.
You will be asked to remove make-up, nail varnish, and jewellery.
What will happen during my procedure?
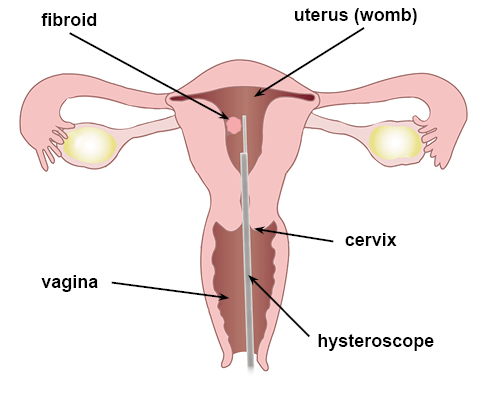
After lubrication (gel) is added, the hysteroscope will be inserted through your cervix (neck of the womb) and into your uterus. A speculum may be inserted in your vagina (as for a smear) to help with the procedure. It is sometimes necessary to use a local anaesthetic to numb the area; this will be either gel or an injection.
To get a good view of your womb, a small amount of liquid will be released through the hysteroscope to fill your womb. This allows the hysteroscopist to see the whole lining of your womb.
A biopsy (a little bit of tissue) from the lining of your womb may be taken. Occasionally small polyps / fibroids may be removed or cauterised under local anaesthetic. The hysteroscopist may advise you to have a Mirena coil inserted.
Will I have to stay in hospital?
Most people having an outpatient hysteroscopy will be in the clinic 20 to 30 minutes. No recovery time is needed and you are ready to go back to your usual commitments soon after your procedure. You may prefer to take the day off work, as you might feel a little uncomfortable afterwards.
Most general anaesthetic hysteroscopies are performed as a day case, and you can expect to be discharged home within a couple of hours. You should always have someone at home with you, and have access to a telephone on the night following your surgery. In certain cases, you may be advised to stay in hospital overnight.
How will I feel afterwards?
Most patients leave after their procedure saying it was not as bad as they expected.
During the procedure you may have some period type pain. Painkillers such as paracetamol or ibuprofen should help with this pain. We advise that you take these around one hour before your procedure.
You can expect to have some vaginal bleeding for up to a week after your procedure. Please contact your GP or the clinic if you are worried.
What should I do when I go home?
If you had a general anaesthetic
Try to rest for the first 24 hours.
Some women may feel emotional or ‘weepy’ during the first few days, this is normal.
Do not do any strenuous activity for at least 24 hours after your procedure.
Do not operate machinery or do anything needing fine co-ordination or judgement, for example using a cooker, for at least 24 hours.
Do not make important decisions or sign important documents for at least 24 hours.
You must not drive a car, or ride a motorbike or bicycle for 48 hours.
You may eat or drink as you wish; but your appetite may be poor to begin with.
Do not drink alcohol or take sleeping tablets for at least 24 hours.
Will I have to come back to hospital?
This will depend on your particular problem, but usually no. Biopsy results are usually sent to the patient by post four to six weeks after their procedure.
When can I return to work?
If you had a general anaesthetic you can usually return to work three to four days after your procedure. If you had a local anaesthetic then you may return the next day.
What if I have any questions or concerns?
You will be able to ask any questions at the end of your procedure, before you go home. You can always contact the clinic during office hours if needed. The clinic contact details will be on your appointment letter.
If the clinic is closed, please contact your GP or your nearest Emergency Department in an emergency.