Hysterectomy
Information for patients from Women's Health
You have been referred to the hospital for a hysterectomy. This leaflet explains:
what a hysterectomy is
what the alternatives are
what risks are involved; and
what happens before, during, and after surgery.
We hope it will help to answer some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
What is a hysterectomy?
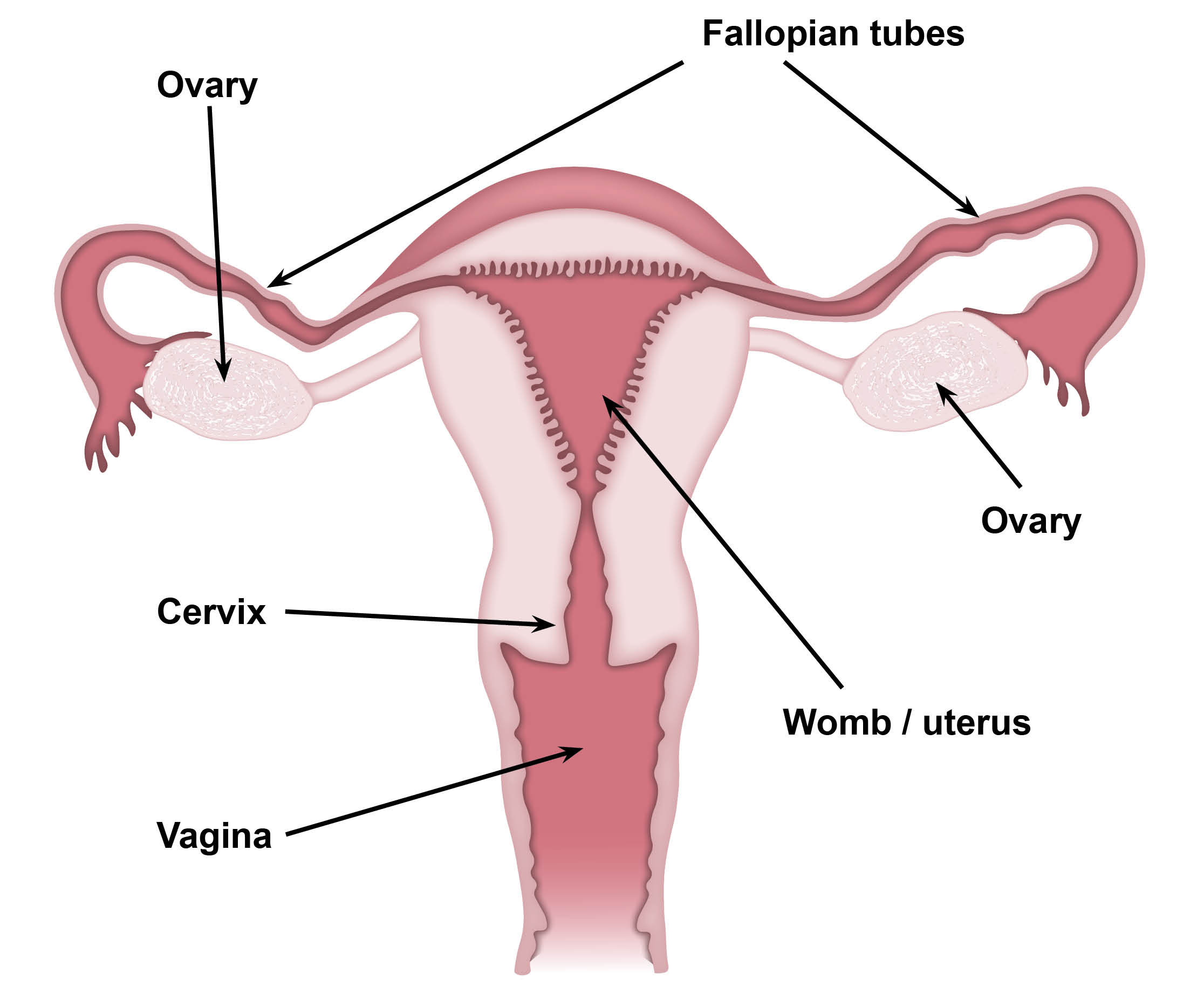
Hysterectomy means removal of the womb. However, there are different types of hysterectomy.
Total abdominal hysterectomy
This is where the uterus and the neck of the womb (cervix) are removed through an incision (cut) in the lower abdomen.
Vaginal hysterectomy
This is the removal of the uterus and neck of the womb through the vagina, without the need for an abdominal incision.
Total abdominal hysterectomy with bilateral salpingo-oophorectomy
This is a total abdominal hysterectomy, but with both tubes and ovaries are removed as well. Sometimes, only one tube or ovary is removed (left or right salpingo-oophorectomy).
Subtotal hysterectomy (with / without salpingo-oophorectomy)
This involves the removal of the body of the uterus (with or without removal of tubes and ovaries) leaving the cervix or neck of the womb behind. This is done through a lower abdominal incision.
Laparoscopically assisted vaginal hysterectomy with or without bilateral salpingo-oophorectomy
During this operation the uterus is removed through the vagina. A laparoscope is used to stop blood loss from the blood vessels serving the uterus and / or ovaries.
Laparoscopic hysterectomy
This procedure can be carried out entirely by keyhole surgery. However, sometimes the surgeon may choose to remove through the vagina (known as laparoscopic assisted vaginal hysterectomy). For more information, see the Trust’s Laparoscopic hysterectomy leaflet.
How will it help and are there alternatives?
There are a number of reasons for performing a hysterectomy, and there are possible alternatives to all. You will have discussed these with your doctor in clinic, but some of the more common reasons for having a hysterectomy are listed below.
Fibroids are benign tumours in the muscle that coats the uterus. They can cause problems, including heavy periods or abdominal pain. Sometimes, a fibroid can press on the bladder and cause urinary symptoms.
Alternatives to hysterectomy include removal of the fibroids alone (myomectomy). If the fibroid protrudes into the uterine cavity, it may be possible to remove it through the vagina. Blocking the blood vessels to the uterus (uterine artery embolisation) is also available.
Pelvic organ prolapse is where organs like the womb or bladder move out of place and press on your vagina. Vaginal hysterectomy is one treatment for this.
Alternatives include vaginal repair procedures, which may be suitable in more minor cases of prolapse. Ring pessaries are sometimes used as a short-term treatment to control the symptoms of prolapse. However, if used in the long-term they can lead to ulceration of the vaginal skin and discharge. As a general rule, the ring pessary is reserved for older and more frail patients.
Endometriosis is a condition where the cells which normally lie in the uterine cavity (endometrium) come to lie outside the uterus. They may cause scarring and cysts to form. Hysterectomy with the removal of both tubes and ovaries may control symptoms. There are more conservative surgical and medical treatments available for this condition.
Hysterectomy will stop periods. However, there are less invasive treatments available, including:
drug therapy
progesterone containing coil (Mirena)
ablation therapy (Thermachoice Balloon / Novasure ablation); or
resection of the endometrium (the endometrium is the lining of the womb).
For certain gynaecological cancers such as cancer of the lining of the womb or ovary, there is little alternative other than surgery. Cancer of the cervix can be treated either by surgery or by radiotherapy, depending on the individual patient.
What are the benefits?
The main benefit to having a hysterectomy is to stop your periods (menstruation). Any symptoms you have that are not related to your womb will not change.
Is the treatment safe?
There are certain complications which are common to all surgery, including:
haemorrhage (bleeding)
wound or urinary infection; and
clots forming in the veins of the leg.
Clot formation can be serious if the clot becomes dislodged and travels to the lung.
You will have an antibiotic at the time of your surgery to minimise your risk of infection.
You will wear compression stockings to minimise your risk of clots forming in your legs.
Patients at higher risk of clotting will also have enoxaparin injections, which thin the blood.
What are the risks?
All operations carry a risk of death: for hysterectomy, this is 1 in every 4000 operations.
All operations carry a risk of complications, but the risk increases if:
you are overweight
have had previous surgery; and / or
have pre-existing medical conditions.
Frequent risks
Wound bruising and delayed wound healing.
Wound, urinary, or chest infection.
Having to pass urine (wee) more often than normal.
If you keep your ovaries, it could bring forward menopause. The evidence for this is not conclusive.
Excessive thickening of the skin incision after healing (keloid).
Serious risks
Two in every 100 patients having an abdominal hysterectomy will have at least one of the following complications.
Haemorrhage needing a blood transfusion.
Return to theatre for more stitches to stop haemorrhage. The abdomen needs re-opening in half of these cases.
Damage to the bladder and / or ureter (the ureter carries urine from the kidney to the bladder). Also long-term problems with how your bladder works.
Venous thrombosis (a blood clot in the calf) or pulmonary embolism (a blood clot in the lung).
Pelvic abscess or infection.
Damage to the bowel.
Extra procedures you may need during your hysterectomy
Repair of damage to bladder, bowel, or major blood vessels. You may need a colostomy if your bowel is injured. A colostomy is an operation to divert one end of the colon (part of the bowel) through an opening in the tummy.
Removal of an ovary for unexpected disease. This will only be done if you have given your consent for this before your surgery.
When serious complications happen during an abdominal hysterectomy, further surgery to save life or prevent serious harm to future health will be carried out. Some complications, such as damage to a ureter, may need further surgery at a later date.
You will discuss all the risks and benefits of your surgery in clinic before your surgery. If you have any questions or concerns, please speak to your doctor or nurse.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
What will happen when I arrive at hospital?
Please refer to your appointment letter, for where to go when you arrive at the hospital.
On admission to hospital you will be greeted by a member of the ward team. This member of staff will discuss with you the care you will receive whilst you are in hospital. You will also be seen by your consultant or one of their team.
Please remove all make-up, nail varnish, and jewellery.
Will I have an anaesthetic?
You will have a general anaesthetic (you will be asleep) for this operation.
Sometimes a spinal anaesthetic is possible. A spinal anaesthetic is an injection that numbs a larger or deeper part of the body. You are awake or have some sedation, but are free from pain.
How will I feel afterwards?
After surgery you will feel pain in your lower abdomen. You will be given pain relief either by:
tablets that can be swallowed
an injection; and
sometimes as suppositories, which can be given via your rectum (back passage).
You may also have a small tube at the edge of your wound and a catheter inside your bladder. If present, these will usually be removed the day after your surgery. However, if you had a bladder repair at the same time as your hysterectomy, the catheter will remain in place for the next few days.
If you had a vaginal hysterectomy, you will be aware of a vaginal pack (rather like a large tampon). This is removed the day after your surgery.
All patients will have a drip in their arm / hand following surgery. Hydration and medication are given through this drip.
Three days after surgery it is normal to get a lot of abdominal wind. This usually settles after you have been for a poo.
How long will I be in hospital?
This will depend on the type of hysterectomy that you had. You can expect to be discharged from hospital:
1 to 2 days following vaginal hysterectomy alone
2 to 4 days after abdominal hysterectomy; and
between 1 and 3 days following hysterectomy with bladder neck repair.
Will I have to come back to hospital?
You may have a follow-up appointment in the Gynaecology Outpatients Department approximately 6 weeks after your discharge from hospital. However, this may not be needed in routine cases. You will be told if you need a follow-up appointment before you are discharged from hospital.
What should I do when I go home?
For the first 2 weeks at home, make sure that you have someone with you and do not do any work.
Do not stay in bed all this time. However, if may help to rest for a couple of hours in the middle of the day.
You may have vaginal discharge, which could last for up to 6 weeks following surgery. The discharge may be pinkish or slightly bloodstained at times. If this loss approaches a period-type loss or greater, contact the Gynaecology Assessment Unit or your GP for advice.
Gynaecology Assessment Unit, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 235009Gynaecology Assessment Unit, William Harvey Hospital, Ashford
Telephone: 01233 633331 extension 723-4257
Between 2 and 6 weeks after going home, slowly return to your normal routine. Do not do any heavy work or lifting for 6 weeks following your surgery.
You may drive again 4 to 6 weeks after returning home. Speak to your insurance company before driving again.
When can I return to work?
When you return to work will depend on the type of hysterectomy you had and your job. You can discuss this with your doctor or nurse at your outpatient appointment.
What do I do if I feel unwell at home?
If you have any questions or concerns, please phone the gynaecology wards listed below or contact your GP.
Birchington Ward, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234201Women’s Health Suite, William Harvey Hospital, Ashford
Telephone: 01233 651987