Humeral fracture
Information for patients from the Trauma and Orthopaedics (T&O) Department
Contents page
What will happen after I leave hospital?
Why have I been fitted with a brace?
How long will I be in the brace?
Can I take painkillers?
What can I do to help my recovery?
What is the best position for me to sleep in?
When can I return to my regular activities?
What if I have any questions or concerns?
Will I have follow-up appointments?
When will my physiotherapy begin?
General things you should and should not do while recovering
Physiotherapy exercises
Contact details
You have broken the shaft of your humerus, the middle of the main bone of your upper arm. Many of these fractures can be treated with a brace and will need physiotherapy two to three months after the fracture has happened.
To begin with you will feel a lot of discomfort, but the recovery is usually very good.
This leaflet will explain what will happen after you have left hospital. If after reading it you have further questions or concerns, please contact us using the numbers listed at the end of this leaflet.
-
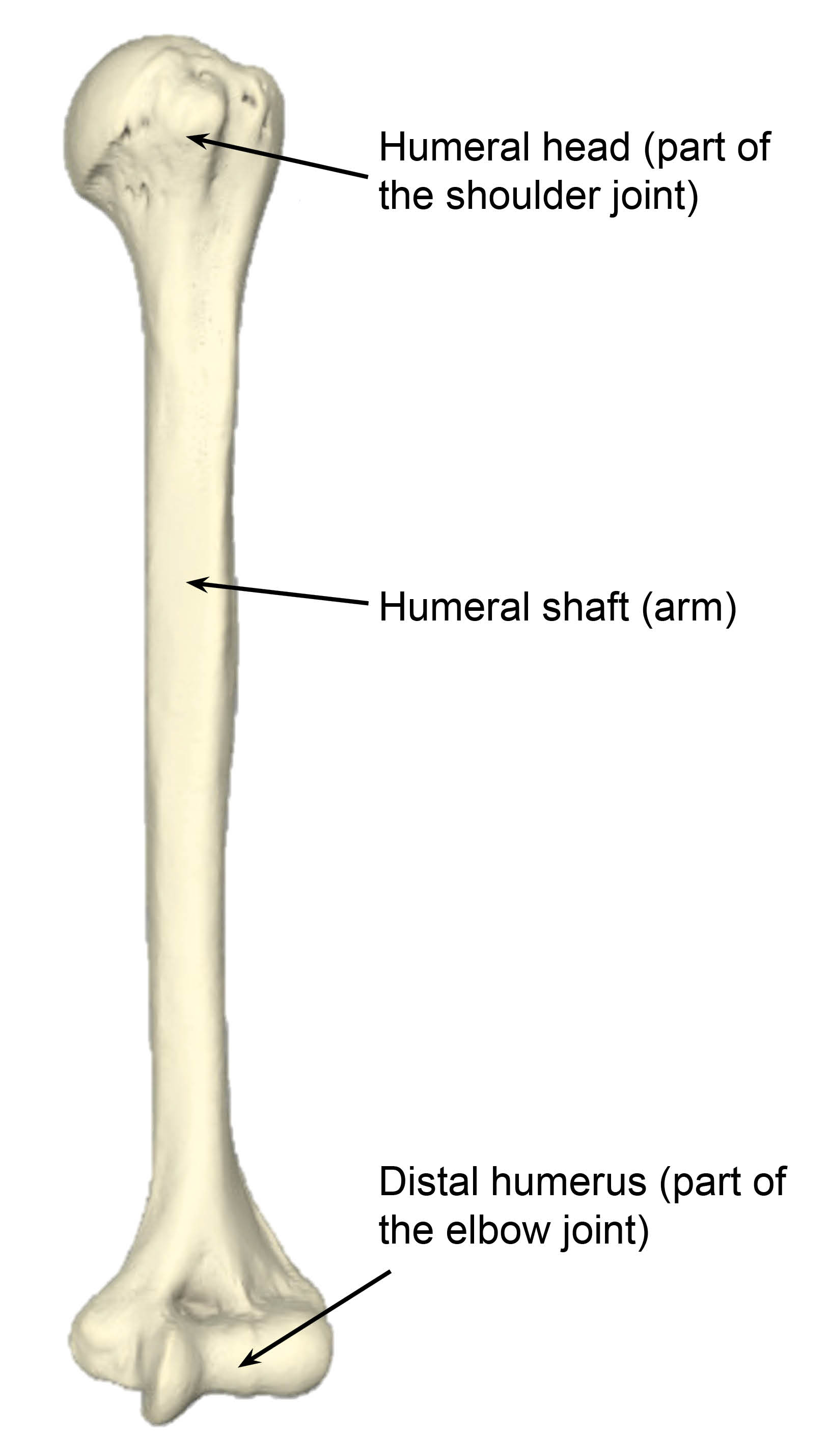 Humerus (upper arm) bone
Humerus (upper arm) bone -
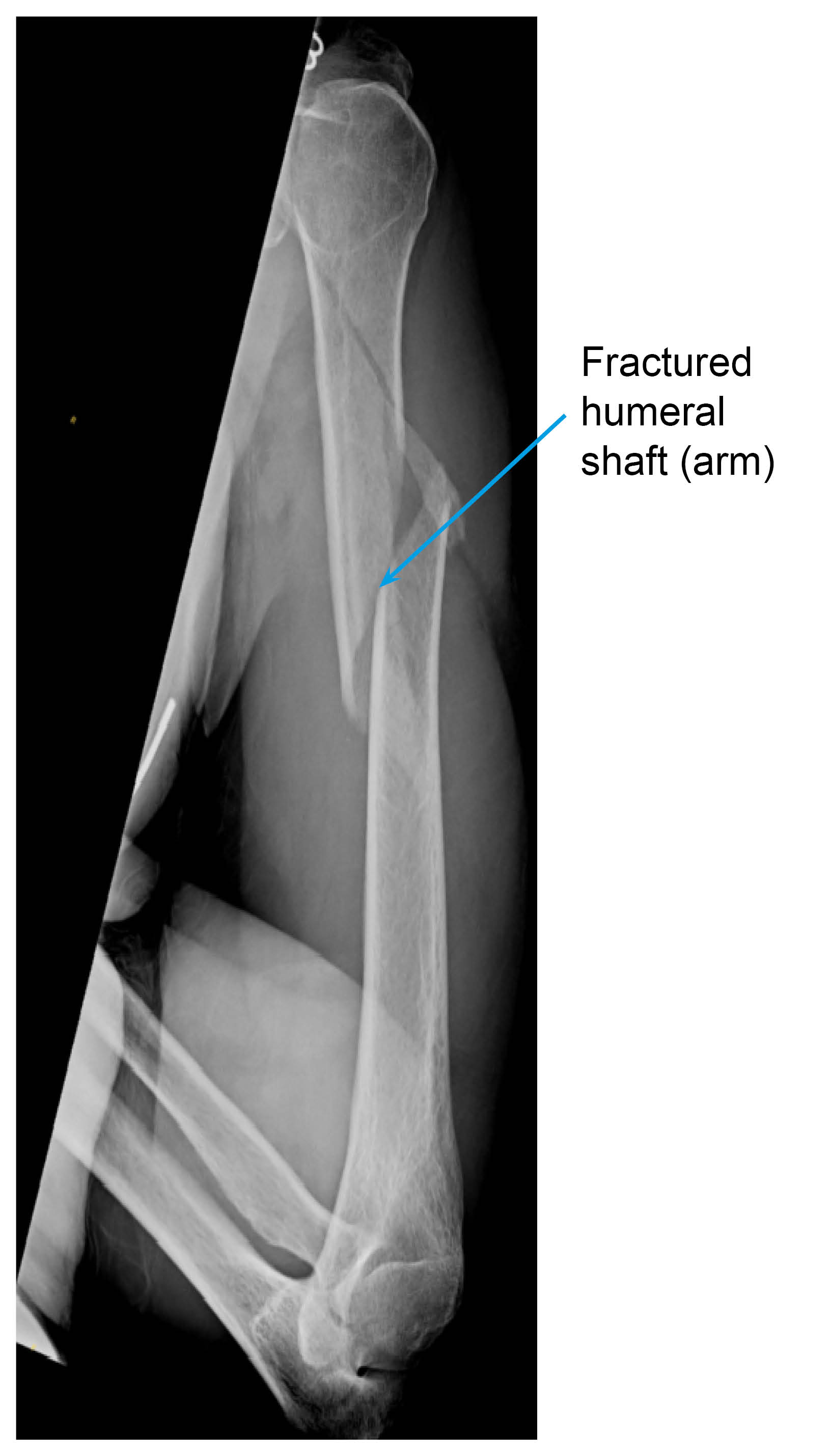 X-ray of a fractured humerus
X-ray of a fractured humerus
What will happen after I leave hospital?
A member of the orthopaedic team will look at the x-rays that were taken in hospital and provide you with a treatment plan within 72 hours. You will get a telephone call from the hospital (from a withheld number) to explain your treatment plan and to let you know if further imaging, such as x-rays, are needed.
If you have not received a telephone call from us within 72 hours, please call the trauma coordinator (all contact numbers are listed at the end of this leaflet).
You will have your first appointment with the orthopaedic team one to two weeks after your fracture. At this appointment you will have new x-rays done, and a member of the team will check your skin and review your new x-rays.
Why have I been fitted with a brace?

You have been fitted with a brace to help with your pain and allow your fracture to heal in a good position.
You must wear the brace all the time, but it is important to stop your arm becoming stiff. In order to help prevent stiffness, as soon as you feel able to, we suggest you carry out the exercises listed later on in this leaflet. These exercises will also help reduce any swelling in your hand. You can also prevent this from happening by trying to keep your hand raised above your elbow.
You must try to keep the area under your arm as clean as possible, without removing the brace. You must not loosen the brace. If the brace becomes loose and you are unable to tighten it yourself, contact the Plaster Room at your local hospital (the contact details are listed at the end of this leaflet).
Contact the Plaster Room immediately if:
you feel that the brace is rubbing or digging into your skin, or the skin breaks down (your wound opens or your skin splits)
you have numbness or “pins and needles” in your fingers
your fingers become blue or white; or
you have severe pain.
How long will I be in the brace?
For a simple fracture you will be in the brace for six to eight weeks.
Can I take painkillers?
You should be taking regular painkillers when you leave the hospital, and this should be continued for at least two weeks. Do not wait for the pain to become really bad before taking the painkillers, as the pain is harder to control once this happens. Try and keep your pain to a bearable level of 2 to 3 out of 10 at all times (on a scale of 1 to 10, 1 being “no pain” and 10 being “the worse pain”).
Patients with a humerus fracture might be given some of the following painkillers, depending on their age, body weight, and individual circumstances, unless told otherwise by their doctor.
Take each painkiller as advised on your prescription.
Tablet paracetamol, 1g every four to six hours (no more than 4g per day).
Codeine Phosphate, 30 to 60mg every six to eight hours.
Tablet Tramadol, 50 to 100mg every eight hours.
Oramorph, 10 to 20mg every hour, as needed.
Anti-inflammatories may be prescribed; but you should try and take as few as possible immediately after your surgery.
Please note that Codeine, Oramorph, and Tramadol should not be taken together; you should only take one of the three.
If your pain continues and is not controlled with the medication you have been advised to take, then please contact your GP. You may also contact the East Kent Upper Limb Team if you need further help.
What can I do to help my recovery?
Smoking advice
It is important to stop smoking while you are recovering from this injury. Studies have shown that wound healing is significantly delayed by smoking / nicotine.
If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
How does eating a healthy diet help my recovery?
Healing of the humerus can take a long time and it is normal to get frustrated and anxious. But remember that while you are recovering, there are some things you can do to help your wound to heal. We suggest limiting the amount of alcohol you drink, stopping smoking, eating a healthy diet, drinking plenty of fluids (especially water), and staying active. If you need any extra support, do not hesitate to get in touch with us on the contact numbers listed at the end of this leaflet.
Some painkillers (especially those containing Codeine) can cause constipation. To avoid this, please follow a healthy well-balanced diet rich in fruit, vegetables (including green leafy vegetables), nuts, seeds, wholegrains, and legumes, which contain the necessary fibre, and drink plenty of water. More information is available on the NHS 5 A Day: what counts? web site.
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
What is the best position for me to sleep in?
We advise you to sleep in a reclined / sitting up position, to help with healing and alignment of your fractured humerus. You may be more comfortable sleeping propped up on several pillows in bed or in a reclining armchair, in the early days after your injury. If you need to sleep on your back, a pillow behind your arm can help you feel more comfortable.
When can I return to my regular activities?
It may take up to four months before you can return to simple daily activities. This may be longer if your work involves strenuous use of your upper limb.
What if I have any questions or concerns?
You can contact your GP, your local Plaster Room, or go to your nearest Urgent Treatment Centre if you experience any problems or have any questions.
Will I have follow-up appointments?
Yes. Arrangements will be made for you to have a Fracture Clinic appointment around seven to 10 days after your injury, to check that the brace is fitted correctly and that your skin has not reacted to it. At this appointment, decisions will be made as to whether you will need further imaging, such as x-rays, and follow-up appointments.
In some cases, an operation will be needed. If so, the orthopaedic surgeon will discuss this with you at your follow-up appointment.
When will my physiotherapy begin?
Physiotherapy usually starts six to 12 weeks after your injury, but this depends on whether the x-ray shows your fracture is healing or not. In the meantime, you should keep moving your arm, following the instructions listed below.
General things you should and should not do while recovering
Do not
Rest your arm / elbow on anything, if possible. This will push your bone ends together and / or bend your bone where is it fractured.
Put your injured arm through any sleeves. Dress with the injured arm under your clothing, close to your body. This will be less painful and will also help to support your arm.
Keep your brace dry. Avoid getting it wet.
You should not have a bath or shower as:
You may struggle to get into and out of a bath safely.
Your balance will be affected, and you may fall in the shower or getting out of the bath.
How do I wash while wearing the brace?
To wash under your injured arm, lean slightly to the side and forward. This will allow you to reach your underarm.
Use a face cloth, soap, and water.
Make sure the area is dried thoroughly afterwards.
Do not try to raise your arm.
A fractured humerus can move around. You may feel or hear the bone moving; this is not unusual but by allowing your arm to relax from the shoulder and hang loose you may reduce or even prevent this from happening.
Physiotherapy exercises while wearing a brace
It is important to stop other joints in your arm getting stiff, and to help with swelling in your arm and hand by doing the following exercises. The exercises should only be completed as your pain allows. They should not make your pain worse.
Do each of these exercises three to five times each day.
Week 1: from the day of your injury to your first Fracture Clinic appointment
Wear the brace and sling all of the time, even in bed at night.
You may remove the sling part to wash yourself and for your exercises.
Do not remove the brace.

Hand exercises
Open and close your fist 20 times.

Wrist exercises (1)
Move your wrist up and down 10 to 15 times.
.jpg)
Wrist exercises (2)
Turn your palm up and down 10 to 15 times.

Elbow exercises
Support your injured arm with your other hand.
Bend and straighten your elbow 10 to 15 times.
Week 1: after your Fracture Clinic appointment with your doctor
You can take your hand out of the sling to do these exercise but keep the brace on at all other times, until told otherwise by your surgeon. Continue with the exercises above and add in the following.
.jpg)
Pendular exercises
Lean forwards, supporting yourself with your other arm.
Move your arm forwards and backwards gently, similar to a pendulum.
Do this 20 times.
Three weeks after your Fracture Clinic appointment
Take your hand out of the sling to do these exercise but keep the brace on until told otherwise by your surgeon. Continue with the previous exercises and add in the following.
.jpg)
Pendular exercises
Lean forwards, supporting yourself with your other arm.
Swing your arm forwards and backwards gently, similar to a pendulum.
Do this 20 times.
Six weeks after your Fracture Clinic appointment, or as guided by your doctor at your Fracture Clinic appointment
If your progress is satisfactory, you will have a physiotherapy appointment and you will be shown further exercises to help maximise your range of movement, strength, and function.
Contact details
Consultants and their secretaries
The teams listed below work at Kent and Canterbury Hospital as well.
| Hospital site | Consultant | Secretary | Contact number |
|---|---|---|---|
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Mr Sathya Murthy | Tracy Blackman | 01843 235068 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Mr Georgios Arealis | Donna Cannon | 01843 235083 |
| William Harvey Hospital, Ashford | Mr Paolo Consigliere | Heather Littlejohn | 01233 616280 |
| William Harvey Hospital, Ashford | Mr Jai Relwani | Dione Allen | 01233 616737 |
| William Harvey Hospital, Ashford | Surgical Care Practitioner | Alphonsa Augustine | 07929 375381 |
Physiotherapists
| Hospital site | Physiotherapist | Contact number |
|---|---|---|
| Buckland Hospital, Dover | Abi Lipinski | 01304 222659 |
| Kent and Canterbury Hospital, Canterbury | Sarah Gillet (inpatient) | 01227 866365 |
| Kent and Canterbury Hospital, Canterbury | Darren Base | 01227 783065 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Caroline Phillipott (inpatient) | 01843 234575 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Martin Creasey | 01843 235096 |
| Royal Victoria Hospital, Folkestone | Ailsa Sutherland | 01303 854410 |
| William Harvey Hospital, Ashford | Cindy Gabett (inpatient) | 01233 633331 |
| William Harvey Hospital, Ashford | Chris Watts | 01233 616085 |
Surgical Preassessment Units
| Hospital site | Contact number |
|---|---|
| Kent and Canterbury Hospital, Canterbury | 01227 783114 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | 01843 235115 |
| William Harvey Hospital, Ashford | 01233 616743 |
Fracture Clinics
| Hospital site | Contact number |
|---|---|
| Kent and Canterbury Hospital, Canterbury | 01227 783075 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | 01843 235056 |
| William Harvey Hospital, Ashford | 01233 616849 |