Preparing for your hip replacement operation at the Elective Orthopaedic Centre, Kent and Canterbury (K&C) Hospital
A patient's guide
A joint replacement operation is done to improve your quality of life. It will hopefully allow you to do some of the things you want to in life, that have become difficult with your joint arthritis.
This booklet has been written by the teams who will look after you during your hospital stay. It aims to help you understand your surgery, and how you can best prepare and recover afterwards.
What is covered in this booklet?
This booklet will guide you through the various stages of your operation.
Welcome to the Elective Orthopaedic Centre
How can I prepare for my operation?
What happens on the day of my operation?
When can I go home after my operation?
What exercises should I do before and after my surgery?
Welcome to the Elective Orthopaedic Centre

The Elective Orthopaedic Centre or EOC, is based at the Kent and Canterbury Hospital. This centre has been completely renovated and opened in August 2021.
This centre offers treatment to people across the south east of England.
The unit is an elective care centre, which means that we only treat patients who have planned surgery. This means that the chance of your operation being cancelled is low, compared to having it in one of our busy general hospitals. Emergency surgeries at these hospitals can often cause planned care to be cancelled.
For more information about the hospital, please visit our website.

In October 2023, the EOC was awarded GIRFT Accreditation.
Accessible Information Standard (AIS)
We have a hearing loop system at the Elective Orthopaedic Centre reception and on the ward.
Please tell staff of any communication needs you have. Please let us know:
If you have any accessibility needs; this includes wanting someone to come with you to your appointment.
If you need an interpreter.
If you need this information in another format (such as Braille, audio, large print or Easy Read).
Infection control
We only treat patients who have followed all appropriate infection control guidelines. The risk of catching an infection whilst in one of our hospitals is extremely low.
High sugar levels in your blood and tissues allow bacteria to grow. This helps infections develop more quickly, so it is important that you make sure that your sugar levels are stable before your surgery.
Staffing
The doctors working in the EOC will be the same consultants as those who would treat you in your local hospital. They are supported by a team of nursing staff and allied health professionals (such as physiotherapists).
Pathway for recovery
Recovering from your joint replacement surgery has changed a lot over the years. We know the sooner we get you up and walking after your surgery, the better your outcomes will be. To help you do this, we have developed a pathway, using the expertise of hospitals across the UK. This should allow you to get back on your feet sooner, and return home to do the things you enjoy.
Returning home, the day after your operation
As a result of expert surgery and anaesthetics, and a highly skilled team of doctors, nurses and allied health professionals, many of you will not need to stay in hospital for more than one night. This is normal in many orthopaedic centres across the country. Since the Elective Orthopaedic Centre opened in August 2021, it has been successfully offering the patients of Kent this excellent standard of care, with very positive results and patient feedback.
We will only discharge you once you are recovered, and are able to safely return home.
Managing and understanding the process
It is important for you to have realistic expectations of having joint replacement surgery. You should have a clear understanding of what to expect at each stage. You must prepare appropriately for your surgery, and work with the clinical teams you meet during your care.
It is important to remember that the work you put in will determine how well you recover.
How do I prepare for my operation?
Why is preparing ahead of my operation important?
The weeks leading up to your operation are as important as the operation day itself. You will be aiming to leave hospital the day after surgery. Therefore, you should plan ahead before your surgery. Think about how things might be for you when you return home.
You must also come to all of your appointments before your surgery date.
Can I drive myself home following my operation?
No. You will not be able to drive yourself home after surgery. You should arrange for a family member or friend to collect you after your surgery. The hospital does not routinely provide transport for your return home.
What if I don’t have anyone that can collect me from hospital? What are my options?
Non-emergency patient transport to our sites is provided by G4S. This is for people whose health means they cannot get to or from their NHS appointment in any other way.
You can find out if you are eligible for patient transport by calling the freephone G4S bookings line on 0800 096 0211, 24 hours a day. You can find out more about the service, including the standard of care you can expect on the G4S website.
Patients (or carers) will be taken through a simple, confidential assessment process to check eligibility.
G4S staff have details of alternative services for patients who are not eligible, including volunteer driver schemes.
The eligibility criteria are set nationally. However, a considerable amount of work has been done in Kent and Medway to ensure that the criteria are applied in a completely fair and consistent way.
Will I need help at home after my operation?
You have probably been living with joint pain for some time before your operation, and will already have ways of adapting to certain situations at home. However, when you are recovering from your operation you may also need some extra help with general tasks, such as cooking, shopping, and cleaning. You need to make sure you organise this help before your operation date.
To make sure that your return home is successful and timely, you may wish to consider having someone at home to support you for the first few days.
Will I need care agency support after my operation?
Very few people need professional care support at home after their surgery. If your personal choice is to have this help, you must arrange this privately. The NHS can only provide professional care based on specifically assessed need after your surgery. We cannot arrange convalescent care.
What do I need to prepare at home before I come into hospital for my operation?
Preparing your home before surgery, is really helpful for when you get discharged. For example:
Freeze some simple-to-cook meals or have some ‘ready meals’ available.
Move any regularly used items that are heavy or out of reach, so you can get to them more easily. For example, move the saucepans you use most often up from any low shelves or cupboards.
Avoid trip hazards by removing any loose rugs or obstacles from the floor. This can be furniture or things that you could easily trip over.
Make arrangements for someone to care for any pets, including walking dogs after your surgery.
You may want to buy a long handled grabber, a long handled shoe horn, and a sock aid. These items will help you carry out your daily tasks following surgery.
Why is it important to keep as fit and healthy as possible before my operation?
The fitter you are before your operation, the less likely you are to have complications during and after your surgery. For more information, please visit the One You Kent web site.
You should make some lifestyle changes, such as:
Cutting down how much alcohol you drink.
Stopping smoking.
Moving around as much as possible and exercising.
Losing weight, if you need to.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
Why do I need to do the physiotherapy exercises?
The exercises in this booklet should be completed before and after your surgery. Doing these exercises before your operation will strengthen your muscles, and will help you to recover more quickly after surgery.
What should I do if I have other health problems?
If you have long-term health conditions you should aim to control these as well as possible before your operation. This will help prevent any complications and avoid your operation being postponed. It would be really helpful for you to check your own blood pressure if you are able to, or get it checked at your GP surgery. If it is above 160 / 90 you are likely to need medication, and the sooner this is started the sooner we will be able to go ahead with your surgery.
If are diabetic, and your HbA1c has not been checked for six months or was over 69mmol / mol the last time it was checked, please arrange to have this checked again and work with your diabetic adviser to improve it. It is very unlikely that you will have surgery if your diabetes is not well controlled and your HbA1c is above this value.
What will happen before the day of my operation?
What happens at my pre-assessment appointment?
Before your operation, you will have a pre-assessment appointment. This is important, as it helps the hospital plan your care.
You will be asked by the hospital to give information about your general health and current medications at this appointment. You may need to give this information via:
computer or mobile app
telephone
video; or
a face-to-face appointment.
At this appointment we will discuss your operation, and help you prepare. For example, we can give you instructions about medications and fasting times (when you need to stop eating and drink before your operation).
At this appointment we will also complete a VTE Risk Assessment. VTE (venous thromboembolism) is a condition that occurs when a blood clot forms in a vein. For more information on preventing blood clots, please see Information for patients having an operation / procedure as an inpatient. This booklet is given at your pre-assessment appointment.
What details will be checked at this appointment?
At your pre-assessment appointment, we will check various medical details, such as:
your general health
your blood pressure
your blood count (to see if you are anaemic)
your kidney function; and
how well you are controlling your diabetes (if needed).
Can I continue taking my normal medication?
We will review any medication you are taking at this appointment. It is fine to continue taking most medicines, and to take them on the day of your surgery. However, there are certain medications you may need to stop taking for a few days before your operation, such as:
blood thinning / anti-clotting medication, or
some blood pressure medications.
We will give you clear instructions if this is needed, and tell you when you should start these medications again after your surgery.
Why have I been given a decolonisation kit?
Getting an infection is one of the main reasons that a surgery is cancelled or postponed. To avoid this, you will be given a decolonisation kit at your pre-assessment appointment. This will keep your skin clean and infection-free. Please use this for two days before your surgery and on the morning of your surgery. Bring the kit into hospital, so you can continue using it after your surgery.
You will be given the following decolonisation kit.

Skin suppression protocol
Octenisan antimicrobial wash lotion (body and hair).
Octenisan nasal gel.
Octenisan instructions
Use for five days total, starting two days before your operation and on the morning of your operation.
Body: use lotion once a day
Hair: use lotion on day 1 and 2 before your operation
Nose: apply nasal gel twice a day
Please bring the decolonisation kit with you when you come in for your surgery, as you will need to continue using it for two days after your operation.
Why do I need to come to the Joint School group session?
The Joint School consists of a presentation outlining your hospital stay, from admission to discharge. This presentation will be given by members of the nursing and therapy team. You will need to complete a questionnaire and bring it to your session. The questionnaire will be reviewed by one of the therapists, and they will arrange for any equipment you may need, and help plan your recovery.
We encourage you to come to the session with a relative or friend, so they can learn how to help you prepare for your operation and for when you return home afterwards.
Please use these sessions to ask any questions that you have.
The equipment is provided by NRS Healthcare.
What happens on the day of my operation?
You will be given a time to arrive at the hospital, which will be on your appointment letter.
Please do not wear nail varnish, false nails, or make-up.
You must have a bath or shower at home before coming to the hospital, using your decolonisation kit.
Can I eat and drink before my operation?
You must follow the fasting instructions below. It is important that you follow the fasting instructions correctly, or your operation may be cancelled on the day. You must not have any food or milky drinks within six hours of your surgery.
We encourage you to continue to drink plain still water up to the time of your operation.
Fasting instructions if you are having surgery in the morning:
Do not eat food after 2:30am. Please do not drink milk or fruit juice with pulp after 2:30am.
You may drink non-alcoholic clear fluids, such as water or black tea / coffee until 6.30am. This does not include fizzy drinks.
Fasting instructions if you are having surgery in the afternoon:
Do not eat food after 7:30am. Please do not drink milk or fruit juice with pulp after 7:30am.
You may drink non-alcoholic clear fluids, such as water or black tea / coffee until 11.30am. This does not include fizzy drinks.
What should I bring to the hospital?
All your current medication, in its original packaging.
Wear loose, comfortable day clothes to get dressed back into after your operation. Your leg may be swollen after your surgery, so make sure your clothes are an appropriate size.

Flat, study footwear with a back.
Toiletries and personal care items.
A change of clothes and nightwear.
Any glasses, hearing aids, or walking aids that you might have.
Phone and charger. Plus headphones, if you would like to listen to music on your own device during your stay.
Bring something to read / keep you occupied in case you have to wait. WiFi coverage varies, but is free. The hospital WiFi password is hospital.
The contact details of the person who will be picking you up.
Any letters you have had from the hospital, giving your arrival instructions for the day of your surgery.
Do not bring in a large number of items. Patients should not bring large sums of money or valuables into hospital. Please note that East Kent Hospitals accepts no responsibility for the loss or damage to personal property, unless the property had been handed to Trust staff for safe-keeping.
What happens when I arrive at the hospital?

When you arrive, you will be greeted by a member of the reception team. They will book you in and confirm some details with you. You will then be seen by one of the nursing team, who will ask some more questions.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page.
Staff will mark an arrow with a pen on the leg that is going to be operated upon.
Meeting your anaesthetist
Before your operation, you will meet your anaesthetist. They will explain the type of anaesthetic that is going to be used. Please ask them any questions you may have about the anaesthetic.
Getting ready for your operation
When it is time for your operation, you will be asked to change into a theatre gown. You will also be asked to put an anti-embolism stocking on your non-operated leg, this is to help prevent a blood clot. You can find more information in the Trust's Preventing a blood clot whilst you are in hospital leaflet.
You will then be taken to the Anaesthetic Room by one of the team, where you will be greeted by your anaesthetist. You will also meet the operating department practitioner, who works with the anaesthetist to look after you.
Routine checks
Some routine checks will be carried out to confirm your identity and to check if you have any allergies. We will also confirm your operation with you, and the side on which you are having your operation.

Attaching monitoring equipment and a drip
One of the team will attach some standard equipment to you. These will monitor your heart, blood pressure, and oxygen levels during your operation.
Your anaesthetist will give you medicine through a drip in the back of one of your hands. These include antibiotics, anti-sickness medicines, and fluids.
Spinal anaesthetic (block)
Most patients will be given a spinal anaesthetic. This is very safe, and avoids the need for having a general anaesthetic, which may cause unpleasant side effects. Spinal anaesthetic also helps you to recover quickly, and helps with any pain you feel after your operation.
Local anaesthetic is placed around some of the nerves in your lower back. This numbs your pain nerves, so that you do not feel pain during your operation. Once the anaesthetic is working well, you will be taken into the operating theatre.
What happens in the operating theatre?
Once you are in the operating theatre, your whole leg will be painted with some cleaning fluid and covered with drapes. You will not be able to see the surgery. The spinal block will prevent you from feeling any of the operation.
Some people find listening to music through their headphones to be a good distraction. It helps them to relax; this will be offered to you. You may wish to bring your own music on your phone or portable music device, and your own headphones.
Some people prefer to have sedation, so they have a light sleep through their surgery. Your anaesthetist will discuss and agree with you a plan depending on your medical history, and your wishes.
After your operation, you may or may not recall hearing noises and conversations during the procedure. This is normal and will not be distressing. The anaesthetic staff will be with you throughout your operation to reassure you.
How long does the operation take?
The operation usually takes about 1½ hours.
What happens after my operation?
You will be transferred to the recovery area, where the nurses will monitor your blood pressure and pulse. Specialist nurses will care for you, making sure that you are comfortable and safe, before you are moved to the ward.
When your spinal anaesthetic has sufficiently worn off, our nursing and therapy teams will help you move out of bed. They will help you to stand and practise walking with suitable walking aids. It is important that you do this as early as possible. You need to be confident that your new joint will work. And moving around helps with:
your pain
allows you to get to the toilet; and
helps stop blood clots from forming.
The team will practise with you:
getting on and off the bed, a chair, and the toilet
give advice on how to dress and manage in the kitchen; and
how to safely go up and down the stairs.
When can I go home after my operation?
You must be able to do the following before you can go home
Your condition must have stabilised.
You must have had something to eat and drink.
You must have passed urine and opened your bowels.
You must be able to safely manage your pain with simple painkillers, such as ibuprofen and paracetamol.
You or your GP practice nurse must be able to look after your wound at home.
You must have been reviewed by a member of the Physiotherapy Team, and completed your assessment.
Remember, everyone's recovery time is different.
Do I need to arrange for support at home?
If you live alone, you may find it helpful to arrange for a friend or relative to stay with you for a few days after you return home. You should arrange this before you come in to have your surgery. This is not essential, as many people who live on their own manage well after their surgery.
How do I look after my wound dressing?
Your wound is covered by a water-resistant dressing. However, you should not shower until your wound has been reviewed. This review will be with a healthcare professional two weeks after your operation, where your wound dressing will be removed. Please leave it in place until this appointment.
Please contact Invicta Ward with any concerns you have about your wound, on 01227 866392.
We will call you 30 days after your surgery to discuss your wound.
Should I keep active after my operation?
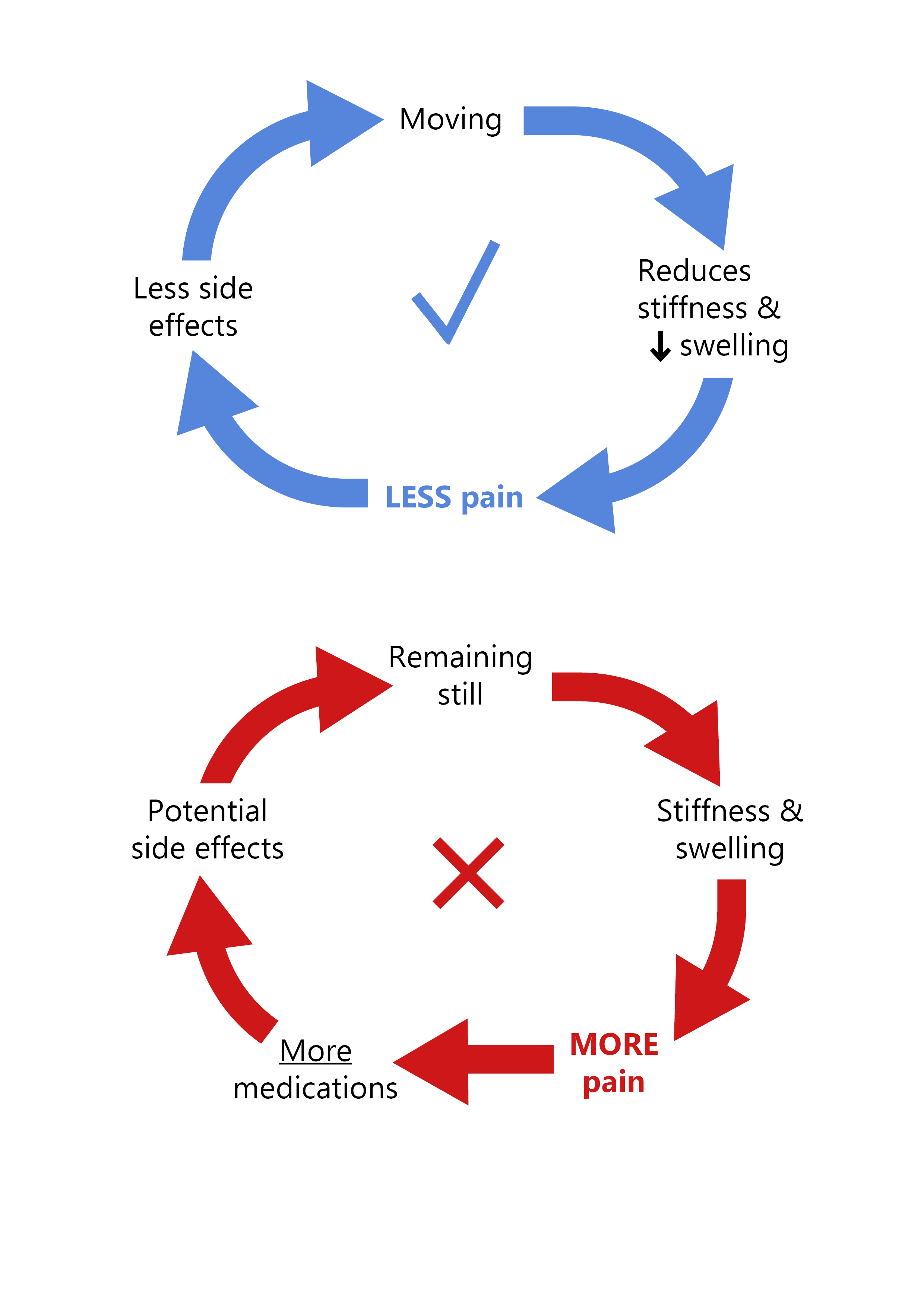
The sooner you can get up and walk after your operation, the better and faster your recovery will be. You will also have a lower risk of developing complications after your surgery. Keeping still after your operation tends to result in your leg swelling, which ends up making it even more painful to walk. This can cause more side effects, which need more pain relief.
Will I be in pain?
Joint replacement surgery is painful, just like any other surgery. The first few weeks can be a difficult time. However, it is important to stay active and do your movement exercises. We will give you strong pain relief medication. However, you should expect there to still be mild to moderate pain when you move. You will not be completely pain-free.
The pain relief you are given after your surgery should control your pain as well as possible. It starts from the day of your surgery, and continues after your discharge home. We will give you the same pain relief tablets whether you stay in hospital overnight, or return home on the same day as your operation.
In order for the pain relief to work, you must take your medicine as advised by your doctor or nurse.
What are the other medications I have been given?
You will also be given medication to help with some of the side effects, including nausea (feeling sick) and constipation (not able to pass stools). We strongly advise you to take this medication.
Other medications will be given to reduce the chance of certain complications, such as blood clots after your operation. You will be given clear information about the medicines you are sent home with, and when to take them.
What will happen when I get home?
My leg is swollen, should I be worried?
It is common to have some swelling in your leg below your hip replacement. Swelling will often get worse if you sit for long periods of time, so we encourage you to remain gently active and do your exercises.
To help reduce swelling in the lower half of your leg, you may need to rest on your bed for at least 20 minutes in the morning and / or afternoon. If you have increased swelling and pain, please contact Invicta Ward for advice.
Why have I got constipation?
You may have constipation due to the pain relief medication you are taking. We will give you some laxative medication as part of your pain relief package. Please make sure that you take these as prescribed, along with drinking two litres (or eight glasses) of water a day. Moving around will also help with constipation. If you struggle, please discuss this with your GP.
How can I control my pain?
Pain is the biggest issue. It is something you should expect after your operation, but you must not stop doing your exercises. To help control your pain, please make sure that you follow the pain management programme you were discharged with.
I am having problems sleeping, is this normal?
Yes. It is common for people to have problems sleeping for the first few weeks after their operation. Please do not worry, as this usually improves with time.
You can sleep in any position, including lying on either side.
When should I contact the hospital?
If your leg becomes hard, swollen, hot and painful, especially in your calf area, this could be a sign that you have developed a blood clot. Please seek medical advice if you get these symptoms.
Infection is very rare. However, if your joint replacement or scar becomes hot, red and / or increasingly swollen, or you feel unwell, please do seek medical assistance.
If you have any of the above, please seek urgent medical advice / assistance from your GP or Invicta Ward. If out of hours, please call NHS 111.
What support will I have once I return home?
The ward team will let you know about any follow-up appointments you may have. Including a routine follow-up telephone call to check on you a few days after your discharge.
Remember, that even after you are discharged from hospital, you are not alone. There is always someone available for you can contact for advice. You will be given information before you go home about who to contact should you need any help.
If you would like more information before your operation or have any questions in the first seven days after you have been discharged home, please ring Invicta Ward on 01227 866392. One of the nursing staff will be able to advise you, or they will contact a member of your surgical team for you.
For therapy related queries, please contact us on either 01227 766877 extension: 722 5421 or email. There is an answer service, so please leave a message with your name, hospital number and a contact number, and we will call you back.
If you are unable to contact one of the Invicta Ward team, please ring your surgical consultant’s base hospital. Ask to speak to their secretary, who will be able to help you contact one of the team. Contact information can be found on your letter. If you do not have this, then please ask for this on the day of your surgery.
What exercises should I do before and after my surgery?
Completing the following exercises will:
help with your recovery
improve movement in your hip joint; and
develop the strength of your muscles around it.
These exercises should be completed before and after your surgery.
Complete your exercises 3 to 4 times a day, repeating each exercise up to 10 times.
To start with, the exercises may feel difficult due to pain and weakness, so it is important that you take your pain medication regularly. It is normal to feel a stretch around your operation site when exercising.
It is important to continue all the exercises once you have left hospital.
Foot exercise
Move your feet up and down from the ankles when you are sitting or lying down.
This exercise will help reduce swelling in your leg, which can take several months to settle down. It also reduces your risk of developing blood clots.
-
 Foot exercise; point your toes up
Foot exercise; point your toes up -
 Foot exercise; point your toes down
Foot exercise; point your toes down
Static quadricep exercise
Lie on your bed or on a flat surface, with your legs out straight and toes pointing to the ceiling.
Press the back of your knee on to the bed as firmly as possible to tense up your thigh muscle.
Hold for 5 seconds and then relax.
-
 Static quadricep exercise; point toes to the ceiling
Static quadricep exercise; point toes to the ceiling -
 Static quadricep exercise; press back of your knee to the bed
Static quadricep exercise; press back of your knee to the bed -
 Static quadricep exercise; relax your knee
Static quadricep exercise; relax your knee

Gluteal contraction exercise
Stay in the same position, and clench your bottom muscles together as firmly as possible.
Hold for 5 seconds and then relax.
You can also do this exercise while sitting.
Lying hip flexion exercise
Lie on your bed.
Bend the knee of your operated leg, keeping your knee pointing upwards. Do not let your knee point inwards.
Slowly straighten your leg, and return to the starting position.
-
 Lying hip flexion exercise; lie on bed
Lying hip flexion exercise; lie on bed -
 Lying hip flexion exercise; bend the knee of your operated leg, keeping your knee pointing upwards
Lying hip flexion exercise; bend the knee of your operated leg, keeping your knee pointing upwards -
 Lying hip flexion exercise; slowly lower your leg
Lying hip flexion exercise; slowly lower your leg
Lying hip abduction exercise
Lie on your bed, with your legs straight in front of you.
Move your operated leg out to the side, keeping your knee straight and toes pointed to the ceiling.
Slowly return to the starting point.
-
 Lying hip abduction exercise; lie of your bed, with your legs straight in front of you
Lying hip abduction exercise; lie of your bed, with your legs straight in front of you -
 Lying hip abduction exercise; move your operated leg out to the side, keeping your knee straight and toes pointed to the ceiling
Lying hip abduction exercise; move your operated leg out to the side, keeping your knee straight and toes pointed to the ceiling -
 Lying hip abduction exercise; slowly return your leg to the starting point
Lying hip abduction exercise; slowly return your leg to the starting point
Once you are walking comfortably you can start the following exercises while standing.
Hip abduction in standing exercise
Stand and hold onto a solid support.
Put your weight on your opposite leg and lift your operated leg sideways, keeping your knee straight and toes forward. Do this in a slow and controlled manner. Try and keep looking forward.
Slowly lower your leg.
-
 Hip abduction in standing exercise; stand and hold onto a solid support
Hip abduction in standing exercise; stand and hold onto a solid support -
 Hip abduction in standing exercise; put your weight on your opposite leg and lift your operated leg sideways, keeping your knee straight and toes forward
Hip abduction in standing exercise; put your weight on your opposite leg and lift your operated leg sideways, keeping your knee straight and toes forward -
 Hip abduction in standing exercise; slowly lower your leg
Hip abduction in standing exercise; slowly lower your leg
Hip flexion in standing exercise
Stand and hold onto a solid support.
Lift your operated leg, bending your hip and knee up toward your chest.
Slowly lower your leg.
-
 Hip flexion in standing exercise; stand and hold onto a solid support
Hip flexion in standing exercise; stand and hold onto a solid support -
 Hip flexion in standing exercise; lift your operated leg, bending your hip and knee up toward your chest
Hip flexion in standing exercise; lift your operated leg, bending your hip and knee up toward your chest -
 Hip flexion in standing exercise; slowly lower your leg
Hip flexion in standing exercise; slowly lower your leg
Hip extension in standing exercise
Stand and hold onto a solid support.
Lift your operated leg backwards, clenching your bottom muscles while keeping your knee straight. Do not lean forwards.
Slowly lower your leg.
-
 Hip extension in standing exercise; stand and hold onto a solid support
Hip extension in standing exercise; stand and hold onto a solid support -
 Hip extension in standing exercise; lift your operated leg backwards, clenching your bottom muscles while keeping your knee straight
Hip extension in standing exercise; lift your operated leg backwards, clenching your bottom muscles while keeping your knee straight -
 Hip extension in standing exercise; slowly lower your leg
Hip extension in standing exercise; slowly lower your leg
Once moving comfortably, you can repeat the standing exercises on your unoperated leg, by standing on your operated leg. You can also practice standing still on just your operated leg.
What other exercise should I do after my operation?
Following your operation, you will be referred to your local Physiotherapy Department to continue your rehabilitation. It is important to continue all the exercises once you have left hospital, until you have recovered from your surgery.
Should I walk?
Yes. Following your operation, you will be encouraged to get up and walk with an appropriate aid. It is important to walk on a regular basis, and to steadily increase the distance as you recover. You should be able to put your full weight on your operated leg. You will be given walking aids (usually crutches) before you leave the hospital.
As soon as possible after surgery, try and walk placing one foot past the other in a normal walking pattern. You can progress to using one crutch, or a stick held on the side opposite your operated leg, as soon as you feel safe and comfortable. If you are uncomfortable or limp when walking, continue to use your walking aid.
Walking is good for your new hip, but remember your hip is an artificial joint. Pace your activity, walk and exercise regularly, little and often.

The risk of dislocation is greatest in the first six weeks following surgery. To reduce the risk of dislocation whilst the tissues around your hip are healing, avoid forcing or overstretching your movement. Avoid bending your hip and knee across your body, towards the opposite shoulder as shown in the picture to the right.
Can I kneel?
Yes. To kneel, go down on your operated leg, taking your weight through your unoperated leg.
To come up from the kneeling position, take your unoperated leg forward. Take your weight through this leg and push up into a standing position.
Can I go up and down stairs?
Yes. Your therapist will practise with you how to safely use the stairs before you go home. To go up and down the stairs, use a banister rail if there is one.
Go up leading with the unoperated leg first, followed by the operated leg and then your crutch.
-
 Going up stairs with crutches; place your unoperated leg on the step above
Going up stairs with crutches; place your unoperated leg on the step above -
 Going up stairs with crutches; follow by your operated leg
Going up stairs with crutches; follow by your operated leg -
 Going up stairs with crutches; and then your crutch
Going up stairs with crutches; and then your crutch
Going down, put the crutch on the step below, then step down with your operated leg, followed by your unoperated leg.
-
 Going down stairs with crutches; put the crutch on the step below
Going down stairs with crutches; put the crutch on the step below -
 Going down stairs with crutches; follow with your operated leg
Going down stairs with crutches; follow with your operated leg -
 Going down stairs with crutches; then follow with your unoperated leg
Going down stairs with crutches; then follow with your unoperated leg
When should I rest?
It can take time to recover from a total hip replacement. To start with, you may need to rest on your bed for at least 20 minutes in the morning and / or afternoon. This will help reduce swelling in your leg.
-1700750896.jpg)
What position should I sleep in?
You can sleep in any position, including lying on either side. To start with, when you lie on your non-operated side it may be more comfortable with a pillow between your legs to support your operated hip. When getting into bed, position your bottom back towards the centre of your bed. Slide yourself around into bed, lifting your legs onto the bed.
How should I sit following surgery?
Sit in a comfortable supportive chair after your operation. Ideally in a chair with arms, to help you get up and down safely. To start with, avoid low soft seating after your operation.
How do I get dressed?
Put pants or trousers over your feet, hold the waistband and lower garment to your feet. Insert your operated leg first, followed by your other leg before pulling them up. To undress, do this in reverse.
When putting on shoes and socks, reach down on the inside of your operated leg (this avoids uncomfortable twisting of your hip). A long-handled reacher, shoehorn, or sock aid can make dressing easier. You can buy these from mobility shops, pharmacies, and online.
When can I have sex again?
To start with, it is normal for your sex life to change following a joint replacement. You can have sex again once you feel comfortable.
When can I drive again?
You can travel as a passenger in a car immediately after your operation.
You should sit in the front seat, with the seat well back and reclined. An extra cushion on the seat can be helpful.
Gently lower yourself down onto the edge of the car seat, keeping your operated leg straight and out in front of you.
Slide back into the seat. Lift both legs into the car, as your body turns to sit upright in the seat. You may find a plastic bag on the seat helps you to turn smoothly. Remove the bag once you are seated.
If possible, get into the car directly from the drive or road, rather than the kerb or pavement.
You can usually start driving six weeks after your operation, or when you can perform an emergency stop. Stop regularly on longer journeys, so you can get out of the car to change position and move around.
You should contact your insurance company before you start driving, as you may not be covered. Please speak to your insurance company for more information.
When can I return to work?
Most people are ready to return to work six to eight weeks after their operation, depending on your job.
When can I fly again?
Air travel should be avoided whenever possible for the first six weeks following surgery.
Depending on the sensitivity of the security scanner, your new hip may set off the alarm. This is not usually a problem, as airport security staff are familiar with such situations, but it is best to be prepared by letting them know before you go through the scanner.
When can I return to my normal exercise?
You can start most physical activities again as soon as you feel comfortable and confident.
You can swim once your wound has healed, swimming any stroke including breaststroke.
Exercise bikes and treadmills can be used from six weeks, returning to outdoor cycling once comfortable.
If you play golf, we suggest you start this again gradually after six weeks.
For activities such as tennis, badminton and cricket, we suggest you start these again after three months.
You can run short distances. Running longer distances risks wearing your new joint and reducing how long it lasts.
Contact sports (such as football or rugby) are not advised following this surgery.
Where should I return any equipment to, once I no longer need it?
Crutches should be returned to the hospital when you come for your follow-up outpatient appointment.
All other equipment, which is supplied by NRS Healthcare, please contact them to arrange collection on 01622 235300.
Contact details
Elective Orthopaedic Centre Pre-assessment, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783114Channel Day Surgery Pre-assessment, William Harvey Hospital, Ashford
Telephone: 01233 616263Arundel Unit Pre-assessment, William Harvey Hospital, Ashford
Telephone: 01233 616743Invicta Ward, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 866392Joint School, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 766877 extension: 722 5421
EmailNRS Healthcare
Telephone: 01622 235300