Hip fracture
Information for patients and relatives from the Trauma and Orthopaedics (T&O) Team
This booklet is for you. It will help you to understand:
your injury
what will happen during the operation
your rehabilitation, and
what will happen when you leave the hospital.
Your choices are important and healthcare professionals will support these wherever possible. The whole team aims to help you walk again and leave the hospital. They will provide you with an appropriate level of help.
A hip fracture is a very common injury, over 70,000 people in the UK sustain a hip fracture each year. Hip fractures typically occur in frailer older people, with various other medical problems. But, they can also occur in patients who are otherwise healthy and independent.
Please use this information to start important discussions. You may wish to have them with your family, supporters, and staff. Talks will be about your health – how much help you will need, staying active, and preventing more falls. You will also discuss if you want CPR in the unlikely event you are found without a pulse.
Please be aware that a hip fracture is a major injury. Most people recover well. But, about half of patients with hip fractures:
are not able to move around as they did before their fracture, and
may struggle to walk even with a walking aid, and will need help with daily activities.
Across the UK, 1 in 10 patients (10%) die after a hip fracture without leaving the hospital. This can be due to complications such as stroke, blood clots, heart failure, or other medical issues. While we understand this may be frightening to hear, we will do our best to make sure you receive the best care possible.
If you cannot make decisions while you are in hospital, your healthcare team may talk to your family or carers, unless you asked them not to. You may wish to nominate a family member or carer to make decisions for you, if for some reason they are unable to whilst in hospital. Healthcare workers must follow the Department of Health's advice on consent. They should also adhere to the Mental Capacity Act's code of practice. For more information about the Act and consent, please go to the NHS Managing legal affairs for someone with dementia web page.
Staff members are happy to help. If you have any concerns, please do not hesitate to contact us and ask questions.
Who will be involved in my care?
A multi-disciplinary team (MDT) is a group of health care professionals who will look after you. Each one specializes in a different area of care. The team meet each morning to discuss each patient on the ward.
These are some of the healthcare professionals you will meet
Orthopaedic surgeons are doctors who specialise in treating bone, joint, and muscle disorders. They will visit you when you come into hospital. They will carry out your operation, and will also see you after your surgery. They will check that your wound is healing and that your bones are stable.
Ortho-geriatric doctors help older patients with hip or femur fractures. They focus on complex medical issues during hospital stays. They assess bone health and review falls to prevent more injuries. They also manage any medical conditions you have, including any issues you have after surgery.
Anaesthetists are doctors with specialist skills in administering anaesthetics and critical care.
A consultant is a senior doctor who is in charge of your care. You will have an orthopaedic consultant responsible for your overall care. If you are elderly or need support with other medical issues, an ortho-geriatric consultant will also look after you.
Ward doctors work alongside the consultant to manage your care.
A hip fracture practitioner is a nurse who specialises in hip fractures. They will follow your care throughout your hospital stay. They will also be your point of contact on discharge, if you have any issues with your hip fracture or wound.
Nursing staff include registered nurses and support workers. This team help to meet your care needs while in hospital. During each shift there will be a nurse-in-charge of your care. The ward manager is a senior nurse, responsible for the nursing team and the ward.
Physiotherapists will help you improve balance, strength, and mobility after your injury.
Occupational therapists assess your ability to manage everyday activities. They help predict what care or help you will need after you leave hospital.
The discharge co-ordinator organises your discharge or transfer from hospital. They work with inside and outside agencies, including care homes and care agencies. They will do this to help with your safe discharge from hospital.
What is a hip fracture?
The hip joint is an example of a ball and socket joint with the socket in the pelvis. The ball is the head of the thigh bone called the femur. It is attached to the shaft of the femur by a bone area called the neck of the femur.
A hip fracture is a break at the top of the femur bone. It is sometimes called a ‘fractured neck of femur’ or ‘fracture of the proximal femur’.
Most fractures are the result of a fall, and almost all need surgery. The type of surgery you have will depend on where your bone has broken. Sometimes surgeons fix the fracture with a metal implant to help it heal. In other fractures, it is better to replace the head of the femur with a metal one.
-
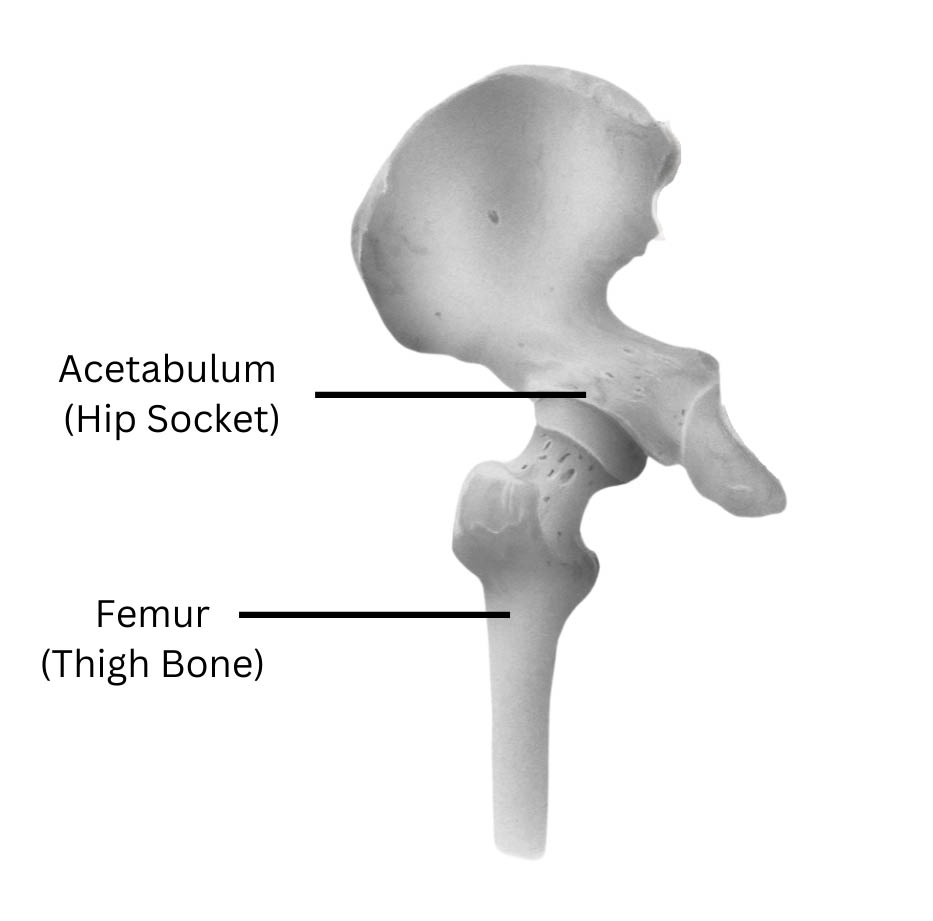 Parts of the hip
Parts of the hip -
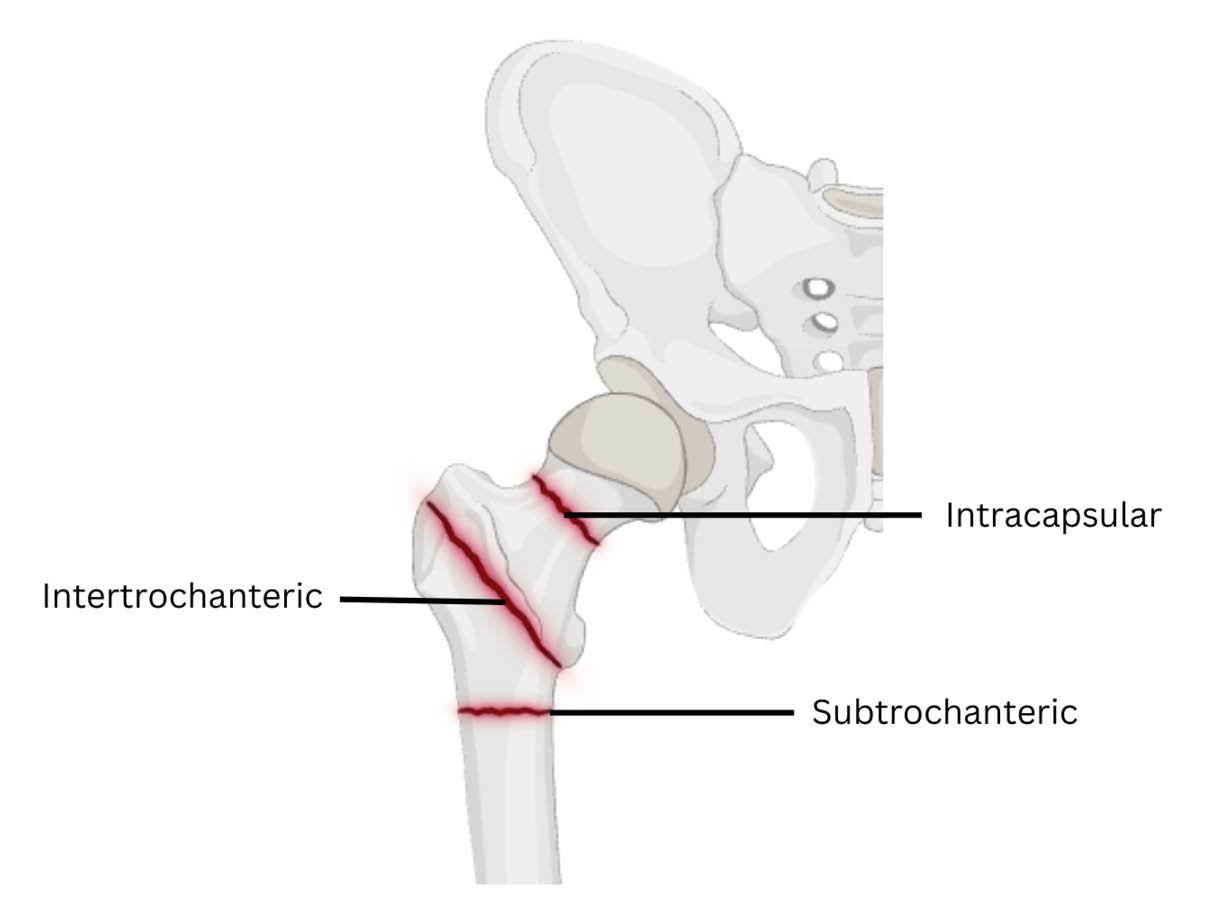 The areas of the femur where different types of fracture commonly occur
The areas of the femur where different types of fracture commonly occur
What causes a hip fracture?
You may have had a fall. Falls are common in older people, and one in three people over 65 will fall each year. Bone does not usually break with a simple fall. However, with age, our bones become weaker. Osteoporosis and other bone diseases can also make your bones weaker. This means that a fall even from standing height can cause a fracture.
Why do I need an operation?
If you have mental capacity the decision to proceed to surgery is yours and yours alone. You may change your mind at any time.
Surgery aims to reduce pain. It also allows you to move around earlier, and lowers the risk that you will not be able to move for a long period of time.
Does every patient have surgery or is there an alternative?
Surgeons operate on most patients with a hip fracture. There are a few exceptions where a hip fracture is managed without an operation, but this is rare. We will discuss alternatives with you, if it is relevant to your situation.
What are the risks of not having surgery?
One of the main risks is ongoing pain.
There can also be serious complications from immobility (not being able to move around). These complications can include chest infections or blood clots in the legs and lungs. Immobility can also lead to sores from pressure on the skin.
There is a significant risk of death (mortality) linked with not having surgery. Our research shows that there is a much higher risk of death for hip fracture patients treated without surgery compared to those who have surgery.
What are the risks to having surgery?
Hip and femur fracture surgeries are common procedures, but can have major implications. All surgical procedures have associated risks and complications.
Loss some or all of your independence. This can depend on how fit you were before you broke your hip. Even for the fittest people, a hip fracture can mean that you do not regain full mobility. If you were less fit when you broke your hip, you may find that after a hip fracture it is hard for you to live alone.
Blood clots: A deep vein thrombosis (DVT) is a blood clot in a vein. This may present as a red, painful, and swollen leg. DVTs can lead to ulcers and swelling in the long-term. A DVT can travel through the blood stream and lodge in the lungs, causing a pulmonary embolism or PE. This is a very serious condition which affects your breathing. Being mobile is one of the best ways to prevent blood clots from forming. Doctors also give blood thinning medication through a daily injection or a tablet. This reduces the risk.
Delirium after surgery. Some patients become confused after surgery. This is usually short-term, but rarely it can continue. This complication happens more often in patients who already have dementia. Delirium is more likely if you:
are 65 or older
develop an infection after surgery
are diabetic or have kidney disease
needed a blood transfusion during or after surgery
have low blood oxygen, or
you had a reaction to the sedation.
We will assess and screen you for delirium when your arrive at the hospital and after your surgery. Prevention includes encouraging fluids, nutrition, deep breathing, mobility, and management of pain. Using your glasses and hearing aids to can also help.
Pain: Your hip will be sore after the operation. If you are in pain, tell the staff, who can give you painkillers. Pain will usually improve with time. Some people continue to have pain in their hip area after a fracture.
Chest infection, also called pneumonia. Bed rest increases the risk of developing a chest infection. Getting out of bed, even sitting, lets the lungs work better. It lets you breathe deeply and cough to clear your chest. A chest infection needs antibiotics and can delay recovery after surgery.
Urinary retention. After surgery, many patients struggle to pass urine and have a catheter fitted. The catheter is passed into the bladder to let urine drain. Passing urine with a broken hip or femur is hard. Rarely patients are discharged from hospital with a urinary catheter.
Pressure ulcers are more likely to occur if pain from your hip fracture prevents you from moving in bed. First the skin hurts, and then begins to blister, before turning into an open sore. These can become infected and are difficult to heal if they are large.
Common areas affected are your heels and your buttock. Prevention of pressure ulcers is important. Your nurses will encourage you to turn often in bed. They will help if you cannot move yourself. Eating a good diet is important in preventing pressure ulcers.
Changes in leg length. The leg which has been operated on, may be shorter or longer than the other. This may need a further operation to correct the difference. Shoe inserts can be helpful.
Hip stiffness after the operation. This is especially likely if your movement is limited after your operation. Physiotherapy helps this.
Nerve damage may cause temporary or permanent altered sensation. It may also cause weakness in the leg.
Bone damage. The thigh bone may break when the metal is inserted during surgery. Your surgeon may need to fix this either at the time or at a later operation.
Wound healing problems. Make sure you eat a good diet and drink plenty of water, both in hospital and when you get home. More information is available on the NHS 5 A Day: what counts? web site.
Stopping smoking helps wound healing. If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
Bleeding is usually minor and can be stopped during the operation. However, large amounts of bleeding may need a blood transfusion, or you may need to return to surgery to stop the bleeding and remove the collection of blood. Many patients suffer significant bruising down the leg following surgery.
Blood vessel damage. The vessels around the hip may rarely be damaged. This can cause a blood collection in the tissues, called haematoma. This may need further surgery.
Infection. Despite all precautions, infections occur in around 1 to 3 of every 100 patients. If you have an infection, the wound may become red, hot, and painful. There may also be a discharge of fluid or pus. You will be given antibiotics before your operation, to reduce the risk of this happening. The procedure will also be performed in sterile conditions with sterile equipment.
Doctors usually treat this with antibiotics, but you may need an operation to wash out the joint. In rare cases, the metalwork is removed and sometimes replaced at a later date.
Constipation (not pooing as often or finding it hard to poo). Many patients develop constipation after a hip fracture and surgery. This can be due to diet changes, not moving, not drinking enough water, or painkillers. We will offer you regular laxatives and encourage you to take them. Drinking more water will also help.
The nurses can bring you a bed pan or commode after your operation, so do not worry about not being able to get to the toilet.
Impaired kidney function after surgery. This is common in older patients, particularly those who already have weak kidneys. Blood tests are done to check kidney function, and urine output is also measured. Rarely, kidney function can be severely impaired following surgery.
Metal failure, prosthesis wear, and loosening. It is important to keep everything moving. However, the thousands of movements every day can lead to wear or loosening of the implant. If this happens, you may need further surgery. We will encourage you to do gentle exercises with less impact.
Joint dislocation applies only to hemi-arthroplasty (half hip replacement) or total hip replacement. This is the ball slipping out of the socket of the hip joint, sometimes a long time after the operation. The joint will need to be put back into place, which usually needs an anaesthetic.
Rarely if the hip keeps dislocating, a revision operation may be necessary. After replacement surgery, avoid extreme positions. These include twisting or bending over 90 degrees.
Fracture non-union is not a risk for patients who have had a hip replacement or hemiarthroplasty. Fracture non-union is where the bone fragments of the fracture do not heal together in the normal way. If this happens, you may need further surgery.
Avascular necrosis (AVN) is not a risk for patients who have had a hip replacement or hemiarthroplasty. AVN is a loss of blood supply to the ball of the hip, which makes the bone weak and can cause pain. If this happens, you may need another operation, such as total hip replacement. Smoking can reduce blood supply to bones.
Leg swelling is common in the operated leg, and it can take several months for the swelling to go down . It will improve as your mobility improves. If your leg becomes hot, red, or more painful, tell your doctor immediately.
Stroke is a rare complication. It tends to affect smokers and older patients with other medical problems. If you take blood thinners, you will told to stop taking these before surgery. An alternative form of blood thinner called Enoxaparin will be given via injection.
Death. A broken hip is a very serious condition. In England, 1 in 10 people die in hospital, and another 2 in 10 people do not survive a year. However, most people have a good result. Getting up and about as soon as possible is one of the best ways to keep your body working well.
Anaesthetic risks are usually related to medical conditions. These include heart disease, lung problems, and stroke risk. More information is available in the You and your anaesthetic leaflet.
Most of the complications that develop after surgery result from immobility. We will aim to reduce your risk by getting you up as soon as possible after your surgery.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. More information is available on the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
What is mental capacity?
Having mental capacity means being able to make and communicate your own decisions. Someone may lack mental capacity if they cannot:
Understand information about a particular decision.
Remember that information long enough to make the decision.
Use the information to make the decision.
Communicate their decision.
Many things can cause a lack of mental capacity. It can be:
Permanent, due to a stroke or brain injury. Or it could be due to severe dementia or a learning disability.
Temporary due to confusion, drowsiness (feeling tired), or unconsciousness caused by an illness or treatment.
What happens if I lose mental capacity?
The Mental Capacity Act aims to protect individuals who lack mental capacity. It says:
You have the right to make your own decisions if you have mental capacity.
It assumes you have mental capacity unless you have had an assessment showing you do not.
You need help to make your own decisions.
Any decisions made for you must be made in your best interests.
No-one should say you lack capacity or assume what is in your best interests based on:
your age
what you look like
a mental health diagnosis, or
another medical condition.
How can I plan ahead?
Loss of mental capacity can happen suddenly, so it is wise to plan for this.
Use a Lasting Power of Attorney (LPA), to appoint someone to make decisions on your behalf.
Make an advance decision to refuse treatment. This explains when you would not want medical treatment, if you lacked the capacity to decide that in the future. Advance decisions are legally binding.
Make an advance statement. This sets out your wishes about your care and treatment in case you are unable to communicate them in future. It is not a legal contract, but it helps family, friends, and doctors make choices for you.
More information on the Mental Capacity Act is available on the NHS web site.
What can I expect in the Emergency Department (ED)?
Patients are usually admitted to hospital via the ED.
A team of doctors and nurses will examine you, and ask how your injury happened.
You will have an x-ray taken of your hips. You may also have an x-ray of your chest.
A special tube, called a cannula, is placed into a vein in your arm. The cannula allows fluids and medication to be given to you intravenously. Pain medication is also given via the cannula; please tell staff if you need more pain relief.
You will be offered an injection of local anaesthetic into your groin. This injection will numb the nerves in the hip region, and is called a fascia iliaca block.
You will have routine blood tests, and a tracing of your heart called an ECG.
You may have a tube passed into the bladder called a urinary catheter.
If appropriate, you will be referred to the Orthogeriatric team.
We will discuss your treatment options either in ED or on the ward. If you decide to have surgery, your surgeon will ask for your written consent. They will also draw an arrow on your leg with a marker. This will make sure that they operate on the correct leg.
What will happen before my surgery?
Before surgery you may need further blood tests or other investigations.
You cannot eat for at least 6 hours before your surgery. You may be given fluid through an intravenous drip during this time. This helps prevent thirst and may help with your recovery after surgery.
Many patients worry about how much pain they will experience. You are given regular pain medication, but tell your nurse if it is not enough. Also, tell them if you need more pain relief between regular drug rounds.
Will I have a general anaesthetic?
An anaesthetist will talk to you before your operation, and decide which anaesthetic you will have for your operation. There are two main types of anaesthetic:
general anaesthetic that makes you sleep during the operation.
spinal anaesthetic which prevents you feeling anything from the waist down, but you are awake. The area being operated on is completely numb.
You may also be offered sedation. But sometimes this not possible, due to other medical conditions you have.
There are advantages of a spinal anaesthetic over a general anaesthetic. These include patient safety and significant continued pain relief after surgery. For medical reasons we may use a general anaesthetic. You will discuss this and the risks with the anaesthetist before your surgery.
When will I have surgery?
You will have surgery as soon as possible. In most cases, this is within 36 hours of admission to hospital. However, your surgery may be delayed for one or more of the following reasons.
If you are medically unwell and need further treatment before surgery.
If you are on anticoagulation (blood thinning medication, such as Warfarin). To prevent excessive blood loss, the affects of this medication must be reversed before surgery.
If there are other people waiting for emergency surgery with life threatening injuries.
If you need a specialist operation, such as a total hip replacement.
What operation will I have?
The type of operation you have will depend on which part of your bone is fractured. Your orthopaedic doctor will explain how your hip fracture will be treated. Most patients need an operation with one of four types of hip surgery.
Total hip replacement
A total hip replacement is considered:
when the fracture is in the neck of the femur, and
if osteoarthritis is likely to affect the joint soon due to wear-and-tear.
During this operation, both the ball and socket are removed and replaced by a metal ball and stem, and a plastic cup. This operation is more complex and has a high risk of dislocation and more blood loss. So, the extra risks are only worth taking if you are very active and fit.
Hemi-arthroplasty
When the fracture is in the femur's neck, the broken piece of bone is removed. A metal prosthesis replaces the broken piece of bone. In effect, this is half a hip replacement, where only the ball part of the joint is replaced.
Sliding hip screw or dynamic hip screw (DHS)
This is a larger metal screw which fixes the fracture, and holds it in place with a plate and some smaller screws. It holds the bones in position whilst they knit back together.
Intramedullary nail
Fractures that extend down the femur are fixed with a metal rod. The rod is passed down the middle of the bone, and extra screws hold it in place.
-
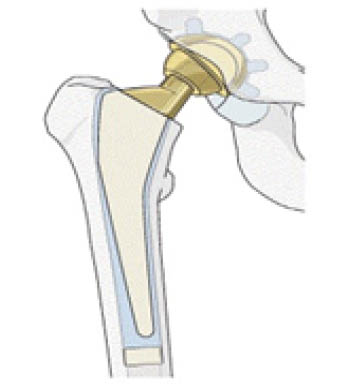 Total hip replacement
Total hip replacement -
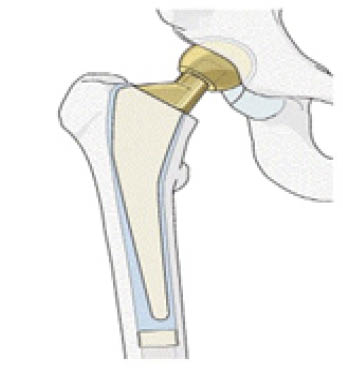 Hemi-arthroplasty
Hemi-arthroplasty -
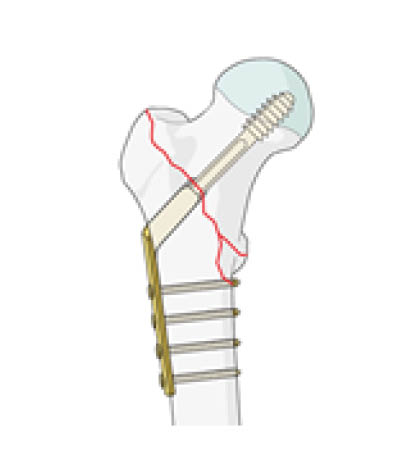 Sliding Hip Screw or Dynamic Hip Screw (DHS)
Sliding Hip Screw or Dynamic Hip Screw (DHS) -
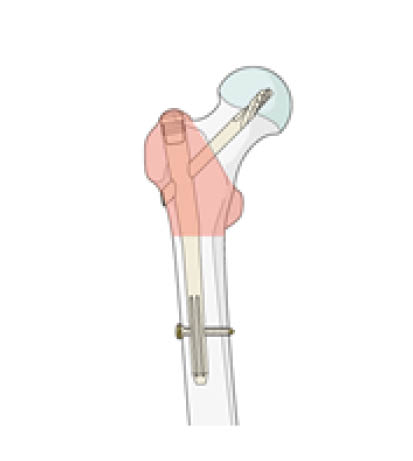 Intramedullary nail
Intramedullary nail
Copyright by AO Foundation, Switzerland. Source: AO Surgery Reference.
What happens after surgery?
After surgery, staff will move you from the operating theatre to a recovery room. Here you will receive one to one nursing care. This allows the nurse to closely watch your recovery from the anaesthetic and surgery. Once you have woken up from your anaesthetic, you will move back to the ward.
You will be offered regular pain medications, and can ask for more as needed.
You may need a blood transfusion, particularly if you are anaemic.
As soon as you feel able, you can eat and drink. If you feel sick, please tell the nurse who can give you medication to help with this. The intravenous drip is removed as soon as you are eating and drinking normally.
If you have a urinary catheter this will be removed once you are mobile and have opened your bowels (had a poo).
The day after surgery you will have blood tests. You may also need to have another x-ray of your leg.
The orthopaedic and orthogeriatric doctors will see you regularly and do a ‘falls risk assessment’. They will start the process for improving your bone health, to reduce your risk of having future breaks.
The nurses will help you with personal care (washing and brushing your teeth) and at mealtimes. However, they will encourage you to do as much for yourself as you can.
Your family, friends, and carers can help you prepare for the first few weeks after discharge. Ask friends or family to bring in supportive shoes or slippers from home. This will make it safer and easier for you to walk.
Nutrition (eating and drinking)
It is important to eat well during this recovery time, to help with healing. Poor appetite is common after surgery. If you or your family are concerned about this, please speak to a nurse. Family can bring you fruit and snacks, and can also help at mealtimes. If you have any allergies, dietary needs, or swallowing problems, please tell your nurse or doctor.
Pain relief
A hip fracture is painful, but this should improve after your operation. You are likely to need regular painkillers for the first few weeks. It is important that you take pain relief, to help you to move more easily. Pain relief will help you do the exercises given to you by your physiotherapist, which will speed up your recovery.
Please let the nurses know if you continue to be in pain: you do not have to wait until the next medicines’ round.
How long will I be in hospital?
Most patients stay in hospital between 8 to 13 days. However, you will get an individual assessment of your needs after your operation. How long you stay in hospital will depend on the results of this assessment. We will make sure that we address your needs before we discharge you from hospital.
What can I expect after discharge?
Understanding what you can and cannot do after surgery is often quite a shock when you get home. This is normal.
It is important to stay mobile and do the exercises you have been shown by your physiotherapist.
There is significant improvement the first 12 weeks after surgery. Most patients will continue to improve for many months, and do not need ongoing physiotherapy.
We will make sure you are safe at home before discharging you from hospital. However, if you still feel unsteady when you first go home, ask for help from a friend or family member. If your progress concerns you, please discuss this with your GP.
Patients with hip fracture are at high risk of developing blood clots. Most patients should keep taking blood thinning medication for 28 days after surgery. This is usually a daily injection, which you or a family member can be taught to give. If this is not possible, a district nurse will visit you after discharge to help with this.
You may be prescribed vitamin D supplements, as most people do not get enough vitamin D in their normal diet. It is important to keep taking this. It will improve your stability and strengthen your bones. If you struggle to take these tablets, talk to your GP. Ask about switching to powder or caplets.
Many patients are also prescribed another medicine to strengthen their bones and prevent further fractures. Often this involves taking the tablet Alendronate, once a week for about three years. Please discuss with your GP if you are having difficulty taking it, as alternatives are available.
Will I have follow-up appointments?
Most patients do not need further x-rays, or any follow-up with the orthopaedic team. If you have concerns about the operation, or if your pain increases, speak to your GP.
The hip fracture practitioner will call you 30 days after your operation. They will ask about your progress and discuss any concerns. They will also ask you about your surgical wound.
There is a national database of hip fracture patients. All NHS Trusts submit data to it. As part of the data collection, you will get a follow-up call 120 days after discharge. You will be asked about your progress, if you are back home, how well you are moving, and if you are taking bone health medication. These calls are with a non-clinical person. If you would prefer not to be contacted, please tell a member of your clinical team while you are in hospital. Ask for this to be added to your electronic patient record.
How do I care for my wound following surgery?
A surgical wound is the cut made to the skin by the surgeon during an operation. At the end of the operation the cut is closed with either stitches or clips. Steri-strips or adhesive dressings (glue) may also be used. These allow the skin edges to come together and heal.
You will need to change your dressing at home. To help your wound to heal and avoid a wound infection:
Before changing your dressing, wash your hands with soap and water.
Carefully take the dirty dressing off, without touching the used side.
Do not touch the healing wound with your fingers.
Do not to touch the inside of the new dressing, so that it remains clean.
Do not use antiseptic cream under the dressing.
If your wound is healing, you can leave it undressed. However, you may prefer to cover it for protection, especially as your clothes can rub it.
We will give you a supply of replacement dressings to use at home.
Will my stitches / clips need to be removed?
Usually, surgeons use dissolvable sutures, which will disappear on their own and do not need removal. However, if your surgeon used non-dissolvable sutures or clips, these will need to be removed. Your GP or practice nurse can do this, 10 to 14 days after your operation.
You may see the ends of the stitches poking out of your healing scar. If used, the clips will also be over the wound. Please do not pull on these. If the loose ends catch on clothes, cover the wound until the stitches / clips are removed. This will stop them from catching.
If you have any worries about your stitches or clips, please speak to the hip fracture practitioner. You can also contact:
Kings C1 Ward, William Harvey Hospital, or
Seabathing Ward at Queen Elizabeth the Queen Mother (QEQM) Hospital.
When can I have a bath or shower?
Showering is preferable to bathing. Soaking your wounds in a bath might soften the scar tissue and cause the wound to open up. Only have a bath if you are sure you can keep your wounds dry.
Some waterproof dressings can be left in place whilst you take a bath or shower. Other dressings may need to be removed beforehand. The nurses will tell you which type of dressings you have before you leave hospital.
Do not put any soap, shower gel, or lotion on your healing wound. Do not use talcum powder or other bathing products. These will cause discomfort and may lead to an infection.
Do not worry if you splash the wound. Pat the wound dry gently with a clean towel after bathing or showering.
Do not rub the wound area. This will cause pain and might slow down healing.
Contact details
If you have any concerns about your wound or the dressing, please contact our hip fracture practitioner. You can find their contact details below.
At 30 days after your operation, you will get a phone call from our hip fracture practitioner. They will ask about your wound and any worries you have after your operation.
Hip Fracture Practitioner, William Harvey Hospital, Ashford
Telephone: 07500 817652 or 07773 152461
Available: Monday to Sunday; 8am to 5.30pmHip Fracture Practitioner, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 07955 320770
Available: Monday to Friday; 8am to 6pm
Physiotherapy
What physiotherapy will I need?
You will be seen by a member of the Physiotherapy team the day after your surgery. With the nursing staff, the team will assess the safest way for you to transfer. They will also teach you some exercises to help with your recovery.
It is important you sit out in the chair every day. The team will help you with this and with your rehabilitation, as advised by the Physiotherapy team.
The physiotherapy team will review you often. They aim to improve your transfers and for you to walk with the right aids.
On your return home it is important you continue to stay mobile and do the exercises you have been shown.
Exercises following hip surgery
You will be taught exercises to help with your circulation. They will also help get your hip moving and improve your muscle strength.
It is important you complete these exercises outside of your physiotherapy sessions. You may need a relative / friend to help you with these.
If able, please aim to complete all exercises on both legs, with emphasis on the operated leg.
Bed exercises
Ankle pumps / rotations
This exercise will help reduce swelling in your leg, which can take several months to settle down. It also reduces your risk of developing blood clots.
-
 Sit or lie down. Move your feet up from the ankles.
Sit or lie down. Move your feet up from the ankles. -
 Move your feet down from the ankles.
Move your feet down from the ankles.
Static quadriceps
-
 Lie on your bed or on a flat surface. Put your legs out straight and point your toes to the ceiling.
Lie on your bed or on a flat surface. Put your legs out straight and point your toes to the ceiling. -
 Press the back of your knee to the bed as firmly as possible, tensing your thigh muscle. Hold for 5 seconds.
Press the back of your knee to the bed as firmly as possible, tensing your thigh muscle. Hold for 5 seconds. -
 Relax your knee.
Relax your knee.
Gluteal contraction exercise
Stay in the same position. You can also do this exercise while sitting.
Clench your bottom muscles together as firmly as possible.
Hold for 5 seconds and relax.
Supported knee bends
-
 Lie on your bed.
Lie on your bed. -
 Bend the knee of your operated leg, keeping your knee pointed upwards. Do not let your knee point inwards.
Bend the knee of your operated leg, keeping your knee pointed upwards. Do not let your knee point inwards. -
 Slowly lower your leg and return to the starting position.
Slowly lower your leg and return to the starting position.
Hip abduction
-
 Lie on your bed, with your legs straight in front of you.
Lie on your bed, with your legs straight in front of you. -
 Move your operated leg out to the side, keeping your knee straight and toes pointed to the ceiling.
Move your operated leg out to the side, keeping your knee straight and toes pointed to the ceiling. -
 Slowly return to the starting point.
Slowly return to the starting point.
Straight leg raise
-
 Lie on your bed, with your legs straight in front of you. Place a rolled-up towel under your knee.
Lie on your bed, with your legs straight in front of you. Place a rolled-up towel under your knee. -
 Tighten your thigh muscle and lift your leg off the bed.
Tighten your thigh muscle and lift your leg off the bed. -
 Hold for 5 seconds and lower slowly. Repeat 10 times, 3 to 4 times a day.
Hold for 5 seconds and lower slowly. Repeat 10 times, 3 to 4 times a day.
Once you are comfortable doing this exercise and have regained some of your muscle strength, you can remove the towel.
Seated exercises
Ankle pumps
Sit in a chair, with your feet flat on the floor.
Bend and straighten your ankles.
Repeat 10 times, 3 to 4 times a day.
Knee extension
-
 Sit in a chair, with your feet flat on the floor.
Sit in a chair, with your feet flat on the floor. -
 Straighten your leg, and hold it out in front of you for 5 seconds.
Straighten your leg, and hold it out in front of you for 5 seconds. -
 Return to the starting position. Repeat 10 times, 3 to 4 times a day.
Return to the starting position. Repeat 10 times, 3 to 4 times a day.
Hip abduction
Sit in a chair, with your feet flat on the floor.
Keep your feet on the floor and move your knees out to the side. To add some resistance, use your hand on the outside of your knee.
Repeat 10 times, 3 to 4 times a day.
Standing exercises
Do all standing exercises while holding onto something for support, such a sturdy chair or walking frame.
Hip abduction
-
 Stand and hold onto a solid support.
Stand and hold onto a solid support. -
 Put your weight on your opposite leg and lift your operated leg sideways. Keep your knees straight and toes forward.
Put your weight on your opposite leg and lift your operated leg sideways. Keep your knees straight and toes forward. -
 Slowly lower your leg.
Slowly lower your leg.
Hip flexion
-
 Stand and hold onto a solid support.
Stand and hold onto a solid support. -
 Lift your operated leg, bending your hip and knee upwards toward your chest.
Lift your operated leg, bending your hip and knee upwards toward your chest. -
 Slowly lower your leg.
Slowly lower your leg.
Hip extension
-
 Stand and hold onto a solid support.
Stand and hold onto a solid support. -
 Lift your operated leg backwards. Clench your bottom muscles, while keeping your knee straight.
Lift your operated leg backwards. Clench your bottom muscles, while keeping your knee straight. -
 Slowly lower your leg.
Slowly lower your leg.
Exercise Programme
You may find it helpful to photocopy the below timetable for keeping track of your exercises.
| Exercise programme | |||||||
|---|---|---|---|---|---|---|---|
| Ankle pumps and rotations | |||||||
| Supported knee bends | |||||||
| Static glutes / buttock contractions | |||||||
| Static quadriceps | |||||||
| Inner range quadriceps | |||||||
| Hip abduction | |||||||
| Straight leg raise | |||||||
| Seated ankle pumps | |||||||
| Seated knee extension | |||||||
| Seated hip abduction | |||||||
| Standing knee raises | |||||||
| Standing hip abduction | |||||||
| Standing hip extension |
Occupational therapy (OT)
What occupational therapy will I need?
Occupational therapists assess your ability to manage everyday activities. Your occupational therapist will meet with you on the ward after your surgery. They will talk to you about your home and how you were managing before coming to the hospital.
As you get more mobile, the Occupational Therapy team will keep assessing you. They will suggest how to manage your daily activities at home. They may suggest small changes to your home. They can lend you basic equipment and refer you to other services for home support if needed.
When you are discharged home, the occupational therapists will make sure you can manage safely. They will also help you be as independent as possible before you go home.
Advice for managing your daily tasks
Transferring on and off a bed
The circle shows which side was operated on, in this case the left-hand side.
Position yourself at the side of the bed, two thirds of the way up.
Make sure you can feel the bed on the back of your legs before you try to sit down.
Try to get onto the bed, leading with your non-operated leg if possible.
Support your upper body with your arms. Slide your bottom as far back onto the bed as you can. Bring your non-operated leg onto the bed.
Bring your operated leg up onto the bed gradually. Use your upper body to move yourself further up the bed.
Try to get out of bed on the same side. Lead with your operated leg, and reverse the steps above.

Transferring on and off a chair
Position yourself in front of the chair, so you can feel the chair on the back of your legs.
Reach back for the arms of the chair.
Straighten your operated leg out in front of you. Lower yourself gently into the chair.
When getting out of the chair, shuffle your bottom forwards and push up using both hands.
Make sure you are balanced, before taking your hands off the chair and onto your walking aid.
Driving and getting in or out of a car
When you can drive again depends on which leg has been operated on and whether you drive a manual or automatic car.
You must make sure you are not a risk to yourself and other road users.
If you can stamp your affected foot hard on the floor, try an emergency stop in a parked car with the engine off.
Discuss driving with your consultant. You must tell your insurance company about your recent surgery.
Transferring in or out of a car as a passenger
The passenger seat should be slightly reclined and as far back as possible, to allow for maximum leg room. If necessary, put a cushion on the seat to raise it.
Sit on the seat before lifting your legs into the foot well. You may find it useful to grip the door frame. Do this whilst someone holds the door steady. Lower yourself gently onto the seat.
Getting in and out of the bath or shower
Following hip surgery, you may find it difficult to get in and out of the bath. Your ability to use a shower safely depends on the style of your shower and the available equipment. It also depends on what walking aids you are using. Please discuss this with your occupational therapist.
For your safety and independence, it is usually advised that you strip wash when you leave the hospital. We also advise you to sit down to get dressed. The following section provides some helpful tips for dressing after your hip surgery.
How to use long-handled aids following hip surgery
You can buy the following aids, which may be helpful after your surgery
Sit on a suitable height chair or perching stool to wash and dress.
It is easier to dress your operated leg first.
To use long-handled aids to dress your lower half
Hold the waist band of your clothing with your helping hand and lower to the floor. You can use the hooked end of a long-handled shoe horn to open the leg hole of the clothing.
Using the helping hand, guide the clothing over your leg and up to your knees, where you can safely reach it.
Carefully stand with the help of a walking aid, to finish dressing your lower half.
Undress your non-operated leg first.
-
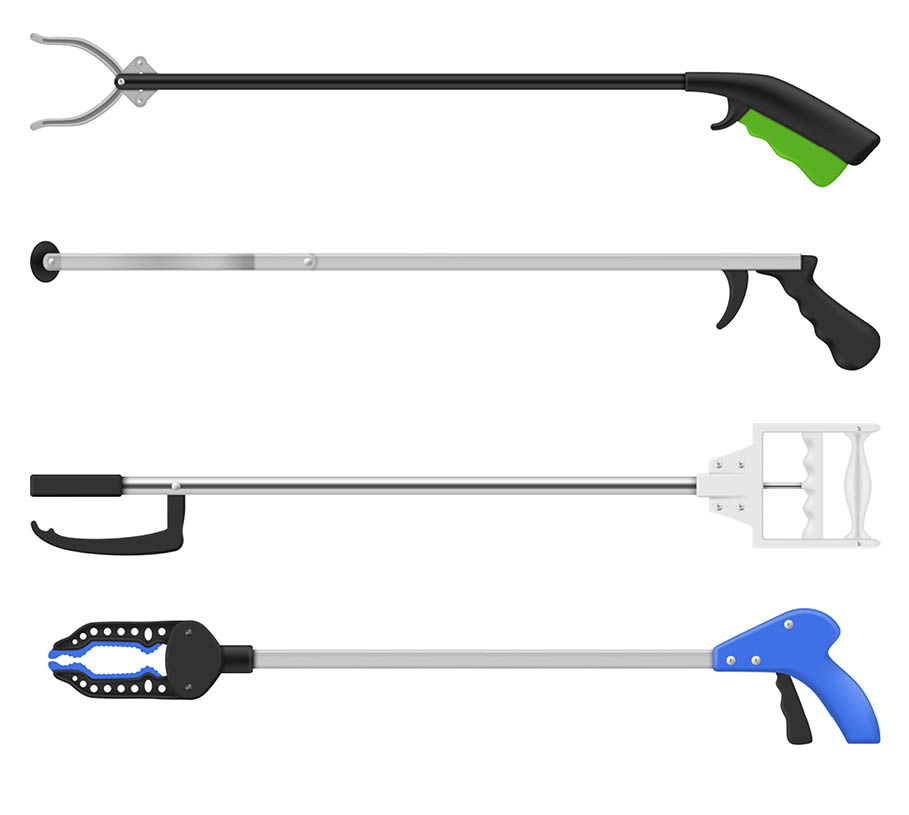 A helping hand
A helping hand -
 A long-handled shoe horn
A long-handled shoe horn -
 A long-handled sponge
A long-handled sponge -
 A sock aid. Please note this cannot be used with anti-embolic stockings.
A sock aid. Please note this cannot be used with anti-embolic stockings.
Managing kitchen tasks
Your occupational therapist will discuss how you will safely do tasks in your kitchen at home. To start with use easy meals. Build up gradually to your usual cooking routine.
You are likely to be discharged home using a walking aid, which will affect your ability to carry items. Your occupational therapist will discuss the set-up of your kitchen at home. They will find any equipment that can make you safer and more independent with food and drink preparation.
Managing household tasks
During your recovery, you may need help with household tasks. These include housework, laundry, and gardening. If you do not have family or friends who can help, speak to your occupational therapist. They may be able to direct you to charities and services who can help after you leave hospital.
Reducing trip hazards
Most hip fractures happen as the result of a simple fall. Falling is not an inevitable result of ageing, but the risk of falling increases as we get older.
During your admission, your orthogeriatric doctor will have assessed your risk of falling. This is to find any medical problems which make you more likely to fall. Your occupational therapist may recommend changes at home to lower your risk of falling. This advice may include the following.
Make sure you use the correct walking aid to provide stability when moving around.
Remove or secure any rugs or loose-fitting carpet.
Make sure you use non-slip mats in the bathroom.
Remove or secure loose wires.
Make sure your lighting is adequate, particularly if you get up at night for the toilet.
Reduce clutter.
Wear appropriate footwear.
Organise your home to reduce your need to bend, stretch, and climb.
Ask for advice on installing emergency buttons (lifeline), to quickly alert others if you fall.
Make sure you have regular eye tests.
What is osteoporosis?
Osteoporosis is a disease, often without symptoms. Bone tissue and bone density gradually decrease. This makes bones fragile, so they break more easily.
If you need dental work (especially surgery), tell the dentist ahead of time if you are receiving treatment for osteoporosis. You may need to stop taking the medicine for a short-time.
Who is at risk of osteoporosis?
We all at risk of developing osteoporosis with age, but it is more common in women and Caucasians. The following increase your risk of developing osteoporosis.
Early menopause
A previous fracture after a minor fall or accident
Family history of osteoporosis
Being severely underweight
Immobility or sedentary (not moving around) lifestyle
Steroid therapy, such as Prednisolone
Smoking
High alcohol intake
Lack of vitamin D, likely due to little sunlight exposure or poor diet
Medical conditions, including an overactive thyroid. Or conditions that affect mobility, including stroke.
How is osteoporosis diagnosed?
Doctors often find osteoporosis after you break a bone from a standing-height fall. They may not need to do more scans. However, you may be referred for a DEXA (Dual Energy X-ray Absorptiometry) scan to confirm osteoporosis.
What are the symptoms and effects of osteoporosis?
Osteoporosis has no true symptoms. It reveals itself after fractures, often in the wrist, hip, and spine from falls.
What can I do to reduce the onset of osteoporosis?
Regular weight-bearing exercise can help to prevent or slow down bone loss.
Adequate calcium and vitamin D intake are important for healthy bones.
If you smoke, try to stop. If you drink heavily, cut down on how much alcohol you drink. For help and advice, please contact One You Kent on 0300 123 1220, or email.
What are the treatments for osteoporosis?
Doctors treat osteoporosis based on many factors. These include your age, gender, and medical history. The aim is to strengthen existing bone, prevent further bone loss, and reduce the risk of broken bones.
Once you start osteoporosis medication, you will likely need it for at least five years. Sometimes, you will need it for life. If you experience any side-effects, please discuss with your doctor before stopping medication. An alternative drug may be more suitable for you.
The bisphosphonates are a group of drugs that include a weekly Alendronate tablet or a once yearly Zolendronic Acid injection via a drip. These are the most commonly used drugs to treat osteoporosis. They work on the bone-making cells. The most common side-effect with Alendronate is indigestion.
Denosumab (Prolia) is a protein that targets specific cells in the body. It works to block the cells that break down bone, allowing the bone-making cells to build-up bone mass. It is given as a six-monthly injection, which can be given at your GP practice or by the Osteoporosis service.
Vitamin D tablets are commonly prescribed in addition to one of the above medicines.
Some osteoporosis treatments very rarely cause a complication. This involves bone loss in the jaw bone, and is called osteonecrosis.
Smoking and osteoporosis
Smoking increases the likelihood of you having osteoporosis. Smoking has a very big impact on bone and tissue healing. Smoking slows healing down by reducing the blood flow to damaged tissues. It raises the risks of complications after surgery very significantly.
If you smoke, you should stop. If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
CPR and Do Not Attempt CPR orders (DNACPR)
What is CPR?
CPR (cardiopulmonary resuscitation) is used to try to restart someone’s heart and breathing, when one or both has stopped. While we hope this does not happen, a hip fracture is a major injury and may make you unwell, especially if you have other medical problems.
CPR includes:
Repeatedly pushing down with force on the centre of the chest.
Blowing air or oxygen into the lungs, using either a mask or a tube inserted into the throat.
At times using electric shocks to try to restart normal heartbeats.
Will I be asked whether I want CPR?
Frequently asked questions
What can be done if I have memory problems?
If you had memory problems before you broke your hip, they may get worse for a while after your operation. Please tell staff as soon as you can.
Surgery and medication can also cause some people to get a condition called delirium. Delirium is a state of mental confusion. Delirium often starts suddenly. It can be scary, but usually improves when the underlying condition gets better. For more information, please ask a staff member for a copy of the Delirium leaflet.
If you had memory problems before your hip surgery, speak to your GP after you recover from your surgery to investigate the cause.
When will I have surgery?
It is unpleasant to be stuck in bed with a hip fracture. The sooner you have surgery, the sooner you will be able to walk again. If you are well enough for surgery, the operation to repair your hip should happen on the day after you are admitted to the hospital.
When will I be able to eat and drink normally again?
You will not be able to have any food or drink, known as ‘nil by mouth’, for a few hours before your surgery. Once you have had your operation, it is very important that you eat well and drink lots of fluids. Food and drink are key to a good recovery from your hip fracture and surgery.
What if I find it difficult to eat or drink?
If you cannot move in bed and sit up at meals, staff will help. Do let staff know if you find eating and drinking difficult at any time. Your family and friends may also be able to help you at mealtimes, so speak to staff to see if this is possible.
How soon after surgery will I get out of bed and start physiotherapy?
The aim of your operation is to let you get up and put weight on your hip right away. This is usually the day after your surgery. You may have some pain and discomfort to start with, and may also feel weaker than usual. This is normal and should improve as you continue to recover. Pain relief will also make getting up and moving around easier.
What can I do if I am having problems with my bladder?
Bladder control problems can happen when you are in the hospital. If you have any problems with your bladder, let ward staff know. If you had bladder problems before breaking your hip, even if your symptoms have not got any worse in hospital, tell staff. They will see if they can help.
How will I be kept updated on my progress?
The team looking after you will keep you updated. They will also tell you about the plans for your discharge. With your permission, they will also discuss this with your family or friends. This is especially important for anyone who plans to help you at home.
What will be done to help reduce my risk of falling in the future?
Most hip fractures happen after a fall, so it is important that you avoid having another one. Staff will assess your risk of falling when planning your rehabilitation and discharge. This will normally include:
a review of your medication; and
physiotherapy to improve your strength and balance.
An occupational therapist will assess your home. They will make sure that you can do day-to-day activities safely.
Can anything be done to strengthen my bones?
Most people who suffer a hip fracture have osteoporosis. This means their bones have become weaker. Treatment is available for osteoporosis, in the form of tablets, drips, or injections. They help to strengthen your bones. Unfortunately, without this treatment, one in five people will have another hip fracture. There are many types of drug treatments. More information is available on the Royal Osteoporosis Society website.
When will I be discharged from hospital?
The average stay in this hospital after a hip fracture is 8 to 13 days. You will have an individual assessment to identify your needs, and your length of stay in hospital can be based on this. We will make sure we address your needs before discharging you from the hospital.
Will I need a follow-up appointment after I leave hospital?
Surgery to repair hip fractures is so successful that, for most patients, this is no longer necessary.
As part of the data collection, you will get a follow-up call 120 days after you leave hospital. The caller will ask you about your progress. These calls are made by a non-clinical person. If you would prefer not to be contacted, please tell a member of your clinical team in the hospital. Ask for this to be put on your electronic patient record.
Useful contacts
William Harvey Hospital, Ashford
Kings C1 Ward
Telephone: 01233 616076Kings D1 Ward
Telephone: 01233 616078Kings D2 Ward
Telephone: 01233 616884Hip Fracture Practitioner
Telephone: 07500 817652 or 07773 152461
Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Seabathing Ward
Telephone: 01843 234575Bishopstone Ward
Telephone: 01843 234576Cheerful Sparrows Female Ward
Telephone: 01843 234571Hip Fracture Practitioner
Telephone: 07955 320770
Further information and advice
The Royal Osteoporosis Society
Telephone: 0808 800 0035Kent Enablement at Home: Kent County Council
Telephone: 01843 873517Age UK
Telephone: 0800 055 6112Your hip fracture: all about your hip fracture and what to expect on the road to recovery (Royal College of Physicians)
One You Kent
Email
Telephone: 0300 123 1220
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email



