Having a transperineal biopsy of the prostate
Information for patients from the Urology Department
This leaflet explains what it involved in a transperineal biopsy, and the possible risks. It is not meant to replace informed discussion between you and your doctor, but can act as a starting point for such a discussion. Please feel free to discuss the examination with your referring doctor or the person carrying out your examination.
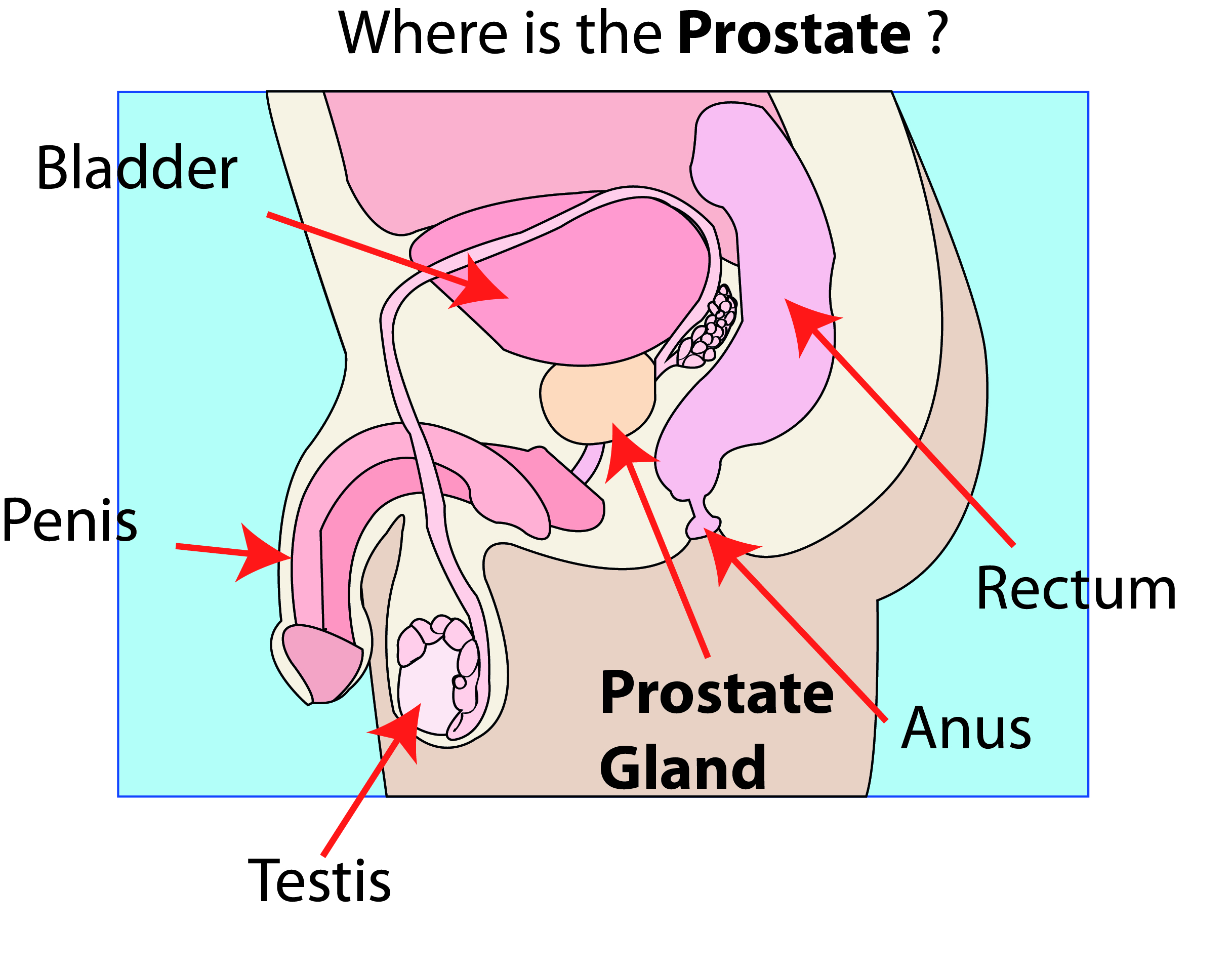
What is the prostate?
The prostate is a small gland, located in the pelvis, between the penis and bladder. It tends to get larger with age, and can partly block the flow of urine.
Why have I been referred for a transperineal ultrasound scan and prostate biopsy?
There are a number of reasons why you might have been advised to have a prostate biopsy.
Your doctor / nurse specialist may have found a lump or abnormality during a digital rectal examination (DRE). A DRE is where a doctor feels your prostate gland through your rectum (back passage) with their finger.
You may have had a blood test showing a high level of prostate-specific antigen (PSA). PSA is a protein released into your blood from your prostate gland. High levels of PSA in your blood may mean there is a problem with your prostate. Further tests are needed to determine what these are.
You may have had previous biopsy results that came back with no evidence of cancer but your PSA blood test is still suspicious.
You may have a known diagnosis of prostate cancer that has not need treatment and your doctor / nurse specialist might want further information to plan for possible treatments or observation.
The biopsy can find out:
if any of your prostate cells have become cancerous or,
if you have pre-existing cancer, whether the cancer has changed.
The biopsy can also diagnose other conditions such as:
benign prostatic hyperplasia (enlargement of the prostate)
prostatitis (inflammation of the prostate, usually caused by a bacterial infection), or
prostatic intraepithelial neoplasia (PIN), which is a change in the cell type but not cancer.
How is the biopsy done?
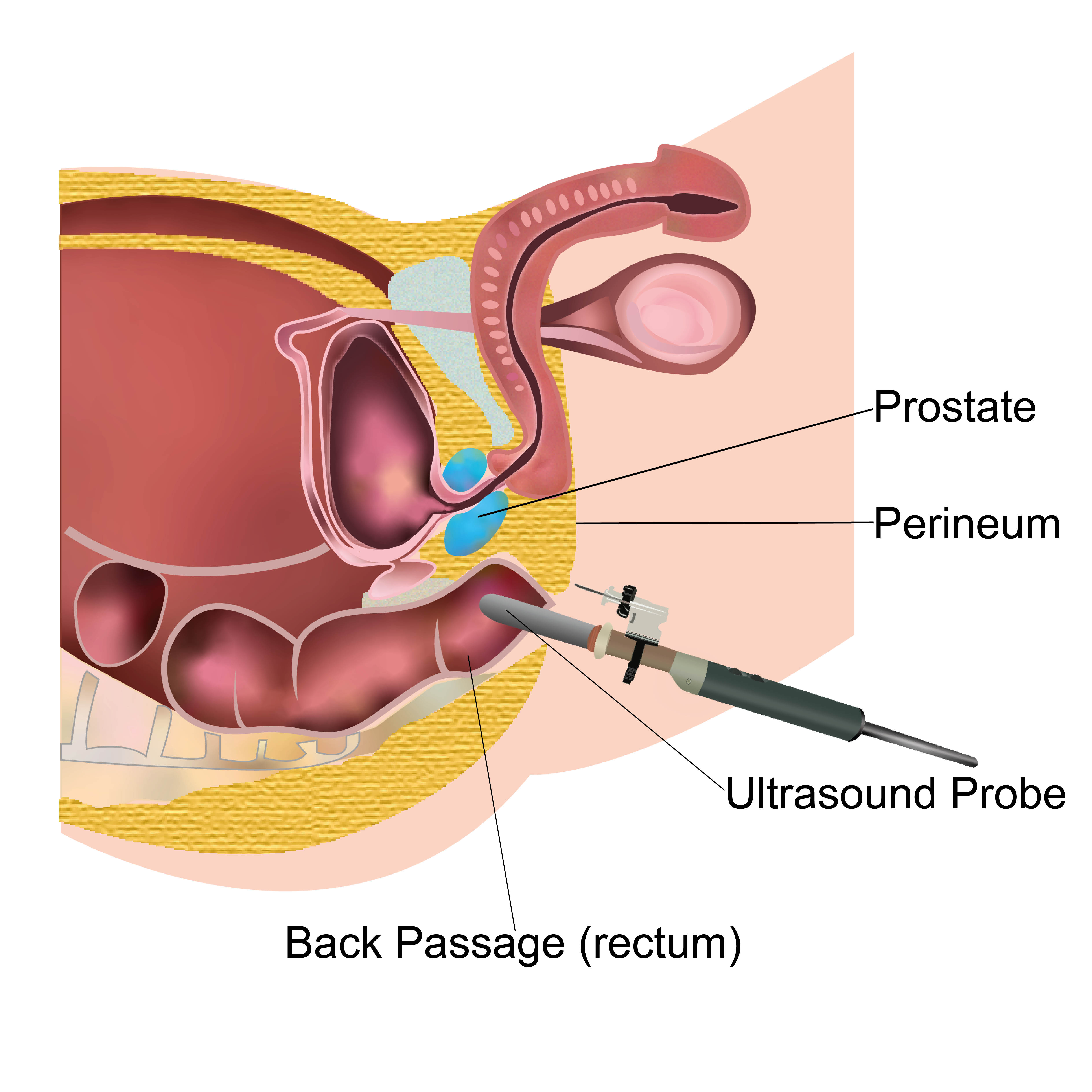
A transperineal template biopsy is used to gain further information about your prostate. Using an ultrasound probe in your back passage, we take samples of your prostate from a different angle through the perineum (the skin between your scrotum and back passage the perineum).
Will the procedure hurt?
You may feel discomfort when the probe is inserted, which is a little wider than your finger. You will have the biopsy under a local anaesthetic. There will be pain and discomfort while the local anaesthetic is being given, like when visiting the dentist. After this you should feel no pain.
Are there alternatives?
If alternatives are available to you, these will be discussed with you on the day of your procedure. The alternatives available will depend on your PSA, MRI results, and following your consultation.
What happens if I choose not to have the procedure?
We recommend you have this procedure. It is the only procedure that will clearly find cancer. Offering the diagnosis needed before you receive further necessary treatment.
Will I need to stay in hospital overnight?
No, you do not need to stay in hospital overnight after having an ultrasound scan and prostate biopsy. However, we ask that you return to Kent and Canterbury Hospital Urgent Treatment Centre (if you are able to) or your local Emergency Department should any complications arise following your procedure.
Are there any risks or complications?
Small amounts of blood in your urine may occur for up to 10 days after your procedure, sometimes longer; this is normal. If bleeding becomes heavy or continues, please go to the Kent and Canterbury Urgent Treatment Centre or your local Emergency Department.
Rarely, heavy bleeding happens at the time of your biopsy. If it does, we will keep you in the department until it settles.
Infection can happen to one in 100 patients. It usually happens 24 to 48 hours after your biopsy. If it is a bad infection, you may need hospital treatment with intravenous (IV) antibiotics. This happens to less than one in every 100 patients that develop an infection.
Difficulty passing urine. The biopsy may cause an internal bruise, that causes you to have difficulty passing urine. This can happen in two in every 100 cases. It is more likely to happen in men who had difficulty passing urine before having their biopsy. If you have difficulty passing urine, you may need a temporary catheter. You will need to go to Kent and Canterbury Hospital Urgent Treatment Centre or your nearest Emergency Department. A catheter is a hollow, flexible tube that drains urine from your bladder.
Despite these risks, your specialist will have decided that you should have this examination. Remember that the risks from missing a serious disorder by not having the procedure are considered to be much greater.
Where will the procedure take place?
Your procedure will take place in a room in the Outpatients Department.
Please note that due to the nature of the examination, we are unable to accommodate unaccompanied children within the department.
How do I prepare for a transperineal ultrasound scan and prostate biopsy?
Normally no preparation is needed. However, if you take anticoagulants and dipyridamole we may ask you to stop taking these before your biopsy. Anticoagulants can include the following blood thinning medication:
aspirin, clopidogrel, ticagrelor, prasugrel, rivaroxaban, dabigatran, apixaban, or warfarin.
If we have told you to stop taking your medication before your biopsy, the table below will tell you when to do this.
Please contact Urology on 01227 864383 if you are not sure about when to stop taking your anticoagulants.
| Drug | Should I stop taking my medication? | When should I stop taking my medication before my procedure? |
|---|---|---|
| Warfarin (Coumadin) | Yes | 5 to 7 days |
| Heparin | Yes | 3 to 5 hours |
| Rivaroxaban (Xarelto) | Yes | 48 hours |
| Dabigatran (Pradaxa) | Yes | 48 hours |
| Apixaban (Eliquis) | Yes | 48 hours |
| Edoxaban (Savaysa) | Yes | 48 hours |
| Enoxaparin (Lovenox) | Yes | 6 hours |
| Fondaparinux (Arixtra) | Yes | 48 hours |
| Aspirin | Yes | 12 hours |
| Clopidogrel (Plavix) | Yes | 7 days |
| Prasugrel (Efient) | Yes | 7 days |
| Dipyridamole/aspirin (Aggrenox) | Yes | 3 days |
| Ticlopidine (Ticlid) | Yes | 7 days |
| Eptifibatide (Integrilin) | Yes | 2 to 4 hours |
| Ticagrelor (Brilinta) | Yes | 3 days |
Before you have your biopsy, you should let your doctor or specialist nurse know if you;
Are taking anticoagulant medication.
Are allergic to any antibiotics.
Have or have ever had bleeding problems.
Have an artificial heart valve.
You should continue to take all of your medications as normal, unless you have been told otherwise by the doctor who organised your biopsy.
What will happen when I arrive at hospital?
Please go to the reception desk in the Outpatients or Urology Department (see your appointment letter for details). You will be seen by the specialist who will explain your procedure, before asking you to sign a consent form. Please use this time to ask any questions and raise any concerns you may have.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
What happens during the biopsy?
You will be asked to lie on a table and your legs will be placed in supportive stirrups.
Your doctor / nurse specialist will examine your prostate with a finger in your back passage. They will use a special gel to relax your anus muscle.
They will then tape your scrotum out of the way, and lift your legs so that your hips are bent as far as possible.
The doctor / nurse specialist will use an antiseptic solution to clean the skin between your scrotum and your anus. This is the area through which the biopsies are taken.
You will be given a local anaesthetic injection. This will numb the treatment area, so that you do not feel any pain during the procedure. The injection will sting for a few seconds (a bit like having an injection at the dentist). Once the anaesthetic has had time to work, you should not feel pain. You may still find the procedure uncomfortable.
If you were unable to tolerate the procedure under local anaesthetic, you will need to come back to hospital to undergo the procedure under a general anaesthetic. You will be told when to stop eating and drinking before the procedure. The general anaesthetic will be given through a small needle in the back of your hand. This will make you sleep for the whole procedure, so you will not feel any pain or discomfort.
The probe will be in your rectum throughout the procedure. This is so your doctor / nurse specialist can see your prostate.
A very fine needle is passed through the numb skin of your perineum (below your scrotum). The biopsies of your prostate are taken with a biopsy needle. The needle is inserted into your prostate gland and removes a tissue sample very quickly. You will hear the click of the ‘gun’ as it takes the biopsy. Between 12 and 24 biopsies are normally taken.
Will I need a prescription of antibiotics before receiving my prostate biopsy?
No, you do not need prescribed antibiotics before a transperineal biopsy. Your doctor or specialist nurse will give you advice on the day of your procedure, if needed.
How long will it take?
The complete consultation takes about 45 minutes. The biopsy takes between 15 to 30 minutes.
If you have a general anaesthetic, following your biopsy you will be taken to the recovery room. Your surgeon will see you before you are discharged from hospital.
If you have had a local anaesthetic, you can leave as soon you are passing urine normally.
You must rest for about four hours at home after this procedure.
What do I need to know before I go home?
If you have had a general anaesthetic, you will need someone to help you home. Your muscles may ache, and you may feel woozy because of the anaesthetic.
General anaesthetic takes 24 to 48 hours to wear off, so please rest for this period of time.
Before you leave hospital, you may be given antibiotics to take at home to prevent infection. Your nurse will explain why you have been given these and how long you need to take them for.
Before you leave hospital, we will tell you how your procedure went, and you should:
Make sure you understand what has been done.
Ask your surgeon if everything went as planned.
Let staff know if you have any discomfort.
Ask what you can (and cannot) do at home.
Make sure you know what happens next.
Ask when you can return to normal activities.
Can I drive after my procedure?
You cannot drive for 24 hours after your procedure, or until pain allows and you can carry out an emergency stop pain free. Please arrange for someone to take you home from hospital after your procedure.
When will I receive my biopsy results?
A pathologist will examine the biopsies we have taken. You will have a follow-up appointment within two weeks of your procedure. At this appointment you will discuss your results with your urologist or cancer nurse specialist.
How will I feel afterwards?
You may have mild discomfort in the biopsy area for one or two days after your biopsy.
You may notice some blood in your urine for up to 10 days. You should have plenty of non-alcoholic drinks while you have blood in your urine.
Your semen may be discoloured (pink or brown) for up to six weeks, and occasionally longer. This is nothing for you or your partner to worry about.
What if I have any questions or concerns once I return home?
Please go to your Kent and Canterbury Hospital Urgent Treatment Centre or your local Emergency Department if you experience any of the following.
Your pain gets worse.
You have a temperature higher than 100.4°F (38°C).
You do not pass urine for eight hours.
You start to pass large clots of blood.
You have heavy and non-stop bleeding.
If you need to visit your local Emergency Department, please ask them to contact the on call urology doctor at Kent and Canterbury for advice. The number is 0207 188 7188, bleep number 1228.
If you have any questions about this procedure or your results, please contact:
Prostate Cancer Nurse Specialists
Telephone: 01227 868666 (Monday to Friday, 9am to 5pm).
Urology Department
Telephone: 01227 864383 (out of hours)
Where can I get more information?
Prostate Cancer UK
Provides support and information for men with prostate cancer.
Telephone: 0845 300 8383Macmillan Cancer Support (all numbers freephone)
Telephone: 0808 808 2020 (information on living with cancer)
Telephone: 0808 800 1234 (information on types of cancer and treatments)
Telephone: 0808 801 0304 (benefits enquiry line)
References
Information adapted from Guy’s and St Thomas’ NHS Foundation Trust with kind permission.