Having a sentinel lymph node biopsy and wide local excision for malignant melanoma
Information for patients from the Skin Cancer Multidisciplinary Team (MDT)
If you have recently been diagnosed with melanoma, you may also need a wide local excision (WLE). You may also be eligible and benefit from a procedure called sentinel lymph node biopsy (SLNB).
This leaflet explains the following.
What each procedure involves.
The benefits and risks of having them.
What will happen before, during, and after each procedure.
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please speak to your skin cancer nurse specialist.
What is a sentinel lymph node biopsy?
A sentinel lymph node biopsy is a surgical technique. It is used to find out if melanoma cells have spread from the original site into your lymph glands. The cancer cells in these lymph glands can be so small that they cannot be felt or seen on a scan. The biopsy is the most accurate way of checking for any spread of the melanoma cells.
Once removed, these glands are examined under a microscope.
What is the lymphatic system?
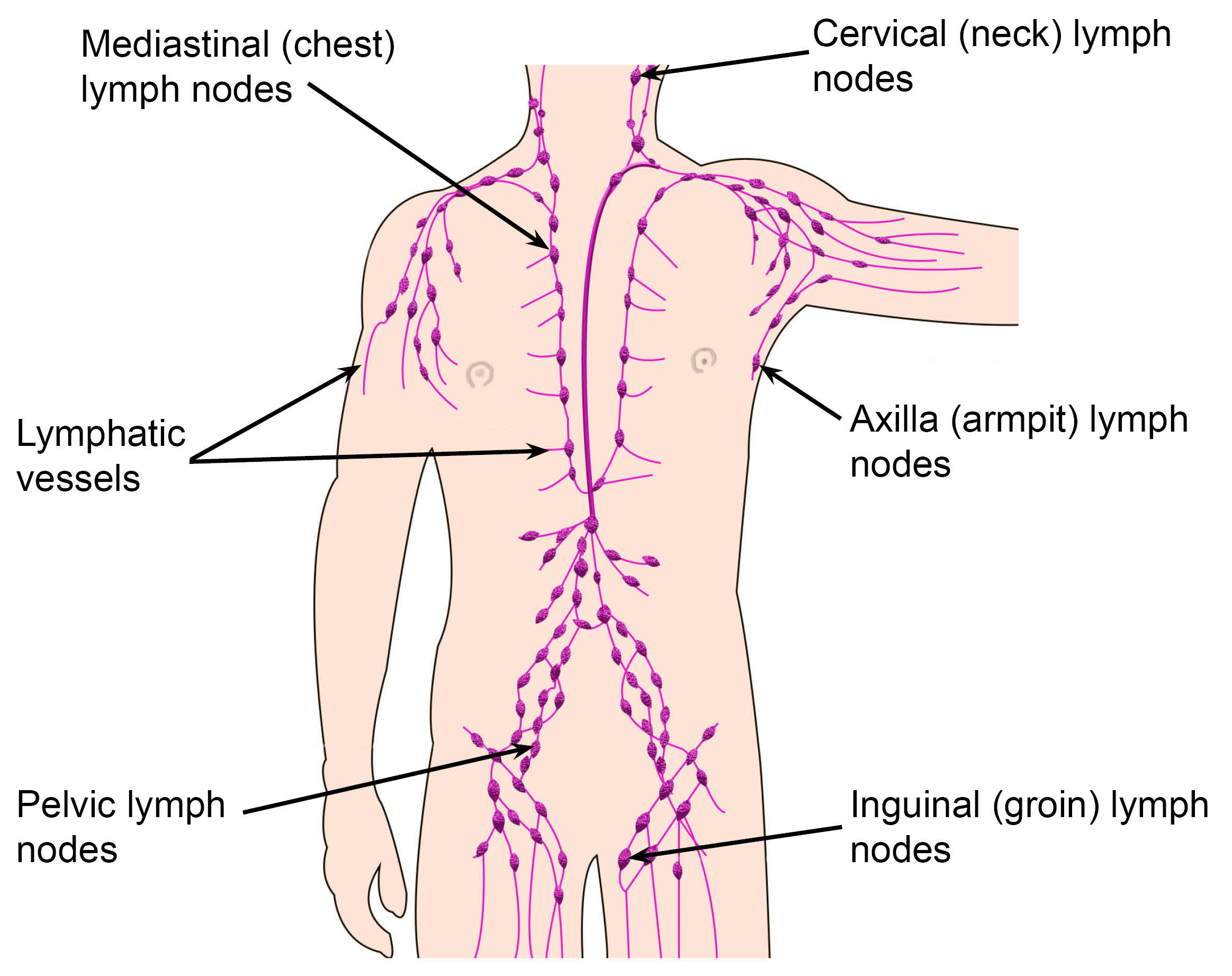
Lymph glands (or nodes) are fleshy structures. They usually lie in groups in the neck, axilla (armpit), groin, abdomen, and chest.
These nodes receive lymph (a clear or whitish fluid) from every part of the body. This is done through a network of fine tubes called lymph vessels.
Each area of skin will drain lymph fluid into certain nodes, usually the group of nodes which are closest. The first node the fluid drains into is called the sentinel node.
Sentinel nodes act like police officers within the lymphatic system, checking what is passing through the body.
Melanoma cells that become loose from the original site, often travel in lymph channels. They pass to the sentinel lymph node, where they become trapped.
As the melanoma cells grow and multiply in the lymph node, the node can become larger and be felt.
However, in the early stages there are very few melanoma cells present in the lymph node. They cannot be felt through the skin. This is why you need a biopsy of the sentinel lymph node. It needs to be examined under a microscope, to see if the melanoma has spread.
What does a sentinel lymph node biopsy involve?
During the procedure, one or more of the nodes the lymph fluid drains into first, are removed. These are closest to the area where the melanoma has been found. For example:
If the original melanoma is on the right calf of your leg, the sentinel lymph node is likely to be in your right groin.
If the melanoma was on your right arm, the sentinel lymph node is likely to be in your right armpit.
In areas like the trunk or head and neck, there may be more than one group of lymph nodes involved.
Who does the sentinel lymph node biopsy?
A specially trained surgeon will carry out your biopsy. The surgeon is part of the Skin Multidisciplinary Team (MDT). They are based at either the:
Queen Elizabeth the Queen Mother (QEQM) Hospital in Margate; or
William Harvey Hospital in Ashford.
The MDT is a team of health professionals specialising in different areas of patient care. The team includes:
dermatologists
surgeons
pathologists
radiologists
a doctor specialising in cancer treatment (oncologist), and
specialist nurses.
The team will discuss your case before your clinic appointment. All members of the team are available to talk to you about what is involved. They can answer any questions you may have, before you decide whether to go ahead with any treatment.
How long will I be in hospital?
This is a day procedure, so you will be able to leave hospital after your procedure. Please allow most of the day for the procedure to be carried out.
What are the advantages of a sentinel lymph node biopsy?
This biopsy is not a treatment, but it does give more information about the stage of your disease. It gives you and your Skin Cancer Team the most accurate information about:
the risks of your melanoma returning; and
what the future may hold for you.
What happens before the sentinel lymph node biopsy?
Before the date of your procedure, you need to come into hospital for a pre-assessment appointment. At this appointment you will speak to a pre-assessment nurse. They will make sure you are fit for surgery and answer any questions you may have. Please use this time to ask any questions.
We want to involve you in all decisions about your care and treatment. If you decide to go ahead with the biopsy, you will need to sign a consent form. This confirms that you agree to have the biopsy and you understand what this involves. For more information, see Why do I need to sign a consent form? below.
The day before your biopsy, go to the Nuclear Medicine Department at the KIMS Hospital Maidstone. At this hospital, you will have a scan called a lymphoscintigraphy. This scan finds the lymph node(s), which your surgeon will remove the next day.
You will be asked to lie down. Small injections containing a tracer are injected around the original melanoma site. It is called a tracer because it is slightly radioactive, and a special scanner called a gamma probe can pick up or ‘trace’ it. Although the word radioactive may sound alarming, it is completely safe.
The tracer drains into your lymphatic channels and lymph nodes. Whichever lymph node(s) the tracer drains into first is the sentinel lymph node(s). A type of x-ray picture is taken. The skin over the sentinel node is marked, to help the surgeon find the sentinel lymph node(s) easily. It helps them make the incision (cut) in the right place, when you have your biopsy.
This scan normally takes about 90 minutes. It can take longer, depending on where the melanoma is and where the lymph nodes involved are. You can go home after the scan.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment. We may ask you to give your consent verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you, and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
Can I eat or drink before my biopsy?
On the day of your biopsy, before your procedure:
do not eat anything for 6 hours; or
drink anything for 4 hours.
If you have food or drink in your stomach when you have the anaesthetic, there is a higher risk of you being sick while unconscious.
Should I take my normal medication on the day of my procedure?
Unless told otherwise, take any regular medicine as usual on the day of your operation. Take only with a sip of water.
What happens during the sentinel lymph node biopsy?
The day after your scan at the KIMS Hospital, you will have your biopsy at either QEQM or William Harvey Hospital. Please refer to your appointment letter for details of where you need to report to.
The biopsy is done under general anaesthetic (you will be asleep and feel no pain). There can be risks involved with having a general anaesthetic, but they are small. Your anaesthetist will talk to you before your biopsy, to make sure you are fit enough to have a general anaesthetic. Please speak to them if you have any concerns about the anaesthetic.
Once you are unconscious, you will have an injection of blue dye around the original area of the melanoma. The blue dye travels along your lymphatic channels to the sentinel lymph node(s).
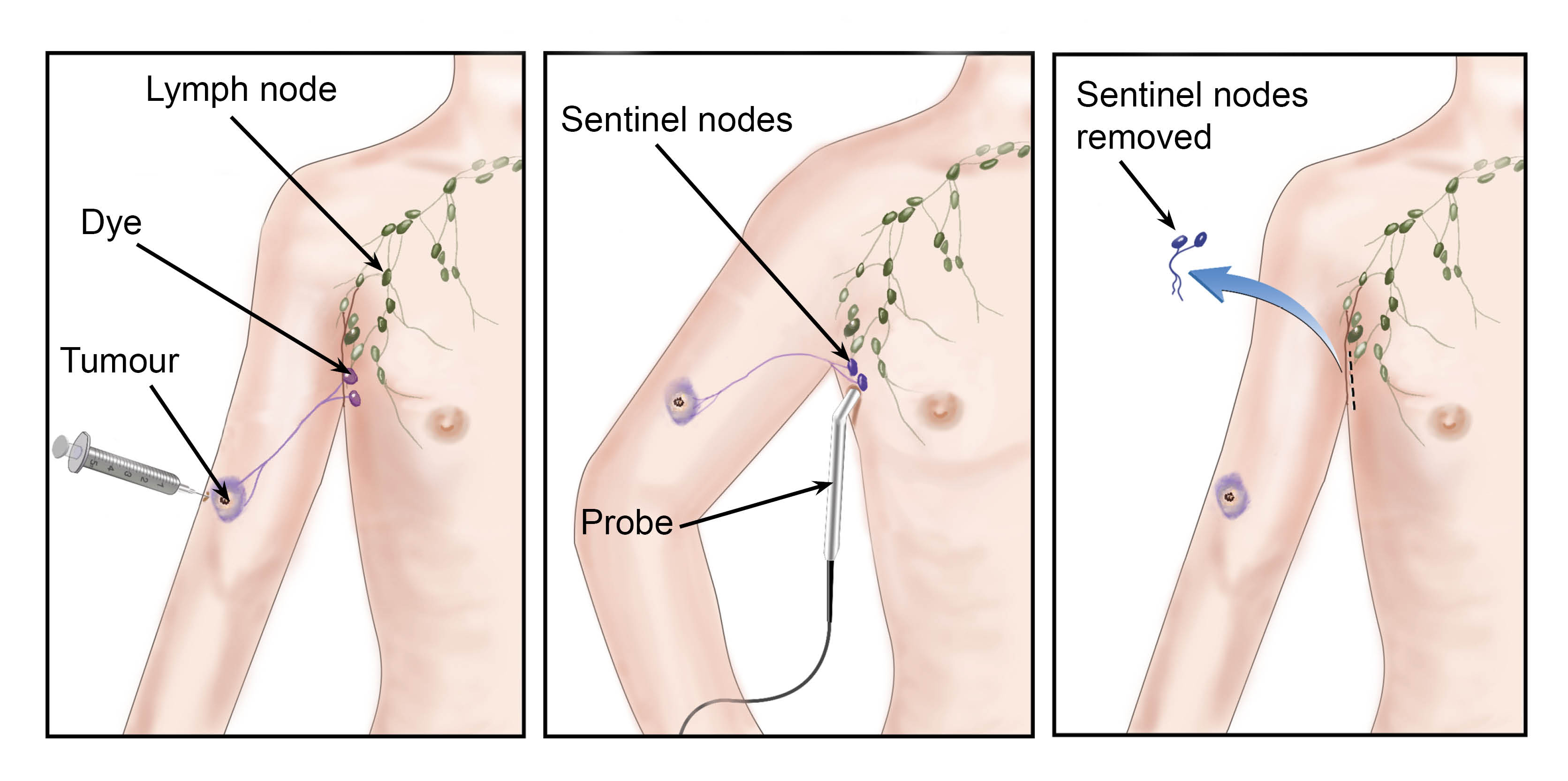
Lymph nodes look like bunches of grapes. The blue dye helps the surgeon to see the sentinel lymph nodes and makes sure they remove (cut out) the correct nodes.
Sometimes (very rarely) we are unable to find the sentinel lymph node during the procedure. Or it may not be possible to analyse the removed node.
Once your surgeon has removed the lymph node(s), they will remove more tissue from around where the melanoma was found. This is called a wide local excision.
What is a wide local excision?
At this stage, the original melanoma will have been removed. There might also be a small scar from your original skin biopsy.
It is important the tissue around the original melanoma is also removed. The removal of this skin is called a wide local excision. Wide local excisions are important as it aims to remove any stray cancer cells which may have been left behind. This lowers the risk of a melanoma returning to that area in the future.
Your surgeon will discuss with you how much skin they will need to remove. This will depend on the thickness of your original melanoma.
What will the area of skin look like after my procedure?
Your surgeon will tell you how they will remove the extra tissue. They will also explain how they will repair your wound afterwards.
Are there any risks with sentinel lymph node biopsy and wider local excision?
Infection: as with all operations, there can be a risk of infection. Your surgeon will do everything they can to reduce this risk. You may notice after surgery your wound becomes red, tender, and swollen. This is not unusual and should improve.
Please contact your GP if you notice signs of infection, such as:
inflammation;
your wound becomes very red and hot; or
you have a raised temperature.
You may need antibiotics to treat an infection.
Seroma: sometimes a pocket of fluid will collect in the area which has been operated on; this is called a seroma. It happens because your drainage system has been interrupted. Signs of a seroma can be swelling, a feeling of fluid moving in the area, and discomfort. This usually settles down by itself after a couple of weeks. In some severe cases you may need to come back to the hospital to have the seroma drained with a needle.
Stiffness in your affected arm or leg is common after your procedure. This will improve as your wound heals. Your team will tell you how and when to move your arm or leg.
Scars: treatment for melanoma can include incisions (cuts) and excisions (cutting out). It is quite common to have scarring left on your skin afterwards. Your surgeon / surgical nursing team will tell you about skin care before you go home.
Discomfort: you may feel some discomfort after your procedure. This will improve as your wounds heal. Your surgeon can discuss painkillers to help with any pain.
Numbness or tingling around your wound should return to normal as your body heals. If you become worried, please contact your Skin Cancer Team.
Blue / green urine: as your body flushes out the radioactive tracer and dye, you may notice your urine is blue / green. This will last for 24 to 48 hours, before returning to normal.
Allergy: there is a small risk that you will have an allergic reaction to the blue dye. Your surgeon will look for signs of allergy while you are unconscious. If you do have a reaction, you will be given medication to reverse the effects of the dye and be monitored.
Lymphoedema: rarely, the affected arm or leg becomes swollen. This is called lymphoedema and is diagnosed by the Skin Cancer Team. It may be temporary or in some cases, permanent. Lymphoedema nurse specialists can help you manage and improve symptoms of lymphoedema. If you have any concerns, please ask a member of your Skin Cancer Team to refer you to the lymphoedema nurse specialist.
What happens if I decide not to have a sentinel lymph node biopsy?
A sentinel lymph node biopsy is not a treatment for melanoma. It is used to get more information. If you would prefer not to have this done, you do not have to; this decision will not affect your treatment.
You will still be offered a wide local excision. This is standard treatment for melanoma and it is likely your Skin Cancer Team will advise you to have this. You will also be offered regular follow-up appointments, so you can be monitored.
What happens after my procedure?
Do not undertake strenuous activities for at least 2 to 4 weeks after your operation. For example:
heavy lifting, including moving boxes or gardening; and
strenuous exercise, such as running, cycling or walking long distances.
When you do resume these activities, do it slowly.
Do not operate machinery or do anything needing fine co-ordination or judgement, for example using a cooker, for at least 24 hours.
Do not make any important decisions or sign important documents for the first 48 hours after your operation.
You must not drive a car, or ride a motorbike or bicycle for at least 48 hours, unless advised otherwise by your doctor. Arrange for someone to collect you from the hospital after your procedure and to take you home (in a car or taxi, not by public transport). Do not travel home on your own.
Arrange for a responsible adult to be with you for the first 24 hours following your operation.
You may eat as you wish, but your appetite may be poor to begin with. You must drink plenty of fluids. Do not drink alcohol or take sleeping tablets for at least 24 hours.
Follow the advice on the leaflets that you have been given.
Some people may feel emotional or “weepy” during the first few days; this is normal.
How do I look after my wound at home?
The affected area(s) is likely to have stitches and be covered by a dressing. A member of the team will tell you how to care for your wound before you leave hospital.
What happens to the removed sentinel lymph nodes?
The sentinel lymph nodes are sent to our laboratory and examined under a microscope.
The results take between 10 to 14 days. You will discuss these with your doctor / specialist nurse at your next clinic appointment.
What happens if the sentinel node(s) contains melanoma cells?
If the sentinel node(s) contains melanoma cells, your doctor or cancer nurse specialist will discuss your treatment options with you at your next outpatient appointment. This may involve:
further surgery; and / or
a referral to oncology, to discuss preventative drug treatment.
Whichever treatment you have, the Skin Cancer Team will check your progress with regular appointments.
What happens if the sentinel lymph node biopsy is negative?
If the sentinel lymph node(s) does not contain any melanoma cells, you will not need any further surgery. You will still need regular appointments so we can closely monitor you.
Summary of advantages and disadvantages of having a sentinel lymph node biopsy
Possible advantages of SLNB
The operation helps to find out whether your cancer has spread to your lymph nodes. It is better than ultrasound scans at finding very small cancers in the lymph nodes.
The operation can help predict what might happen in the future. For example, in people with a primary melanoma that is between 1mm and 4mm thick:
around 1 in 10 die within 10 years if the SLNB is negative
around 3 in 10 die within 10 years if the SLNB is positive.
People who had the operation may be able to have preventative drug treatment with immunotherapy or targeted therapy. This can reduce the chances of the melanoma spreading to other areas of their body in the future.
Possible disadvantages of SLNB
The purpose of the operation is not to cure the cancer. There is no good evidence that people who have the operation live longer than people who do not have it.
The result needs to be interpreted with caution. Of every 100 people who have a negative SLNB, around three will develop a recurrence in the same group of lymph nodes.
The operation results in complications for between 4 and 10 out of every 100 people who have it.
A general anaesthetic is needed for the operation.
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please speak to your specialist nurse at your next appointment.
Contact details
If you have any questions or concerns, please contact the Skin Cancer Clinical Nurse Specialist team on 01227 868666.
Further information
[Websites last accessed 21 January 2026]
References
[Websites last accessed 21 January 2026]
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email