Having a gallbladder operation
Information for patients from General Surgery
What is a gallbladder?
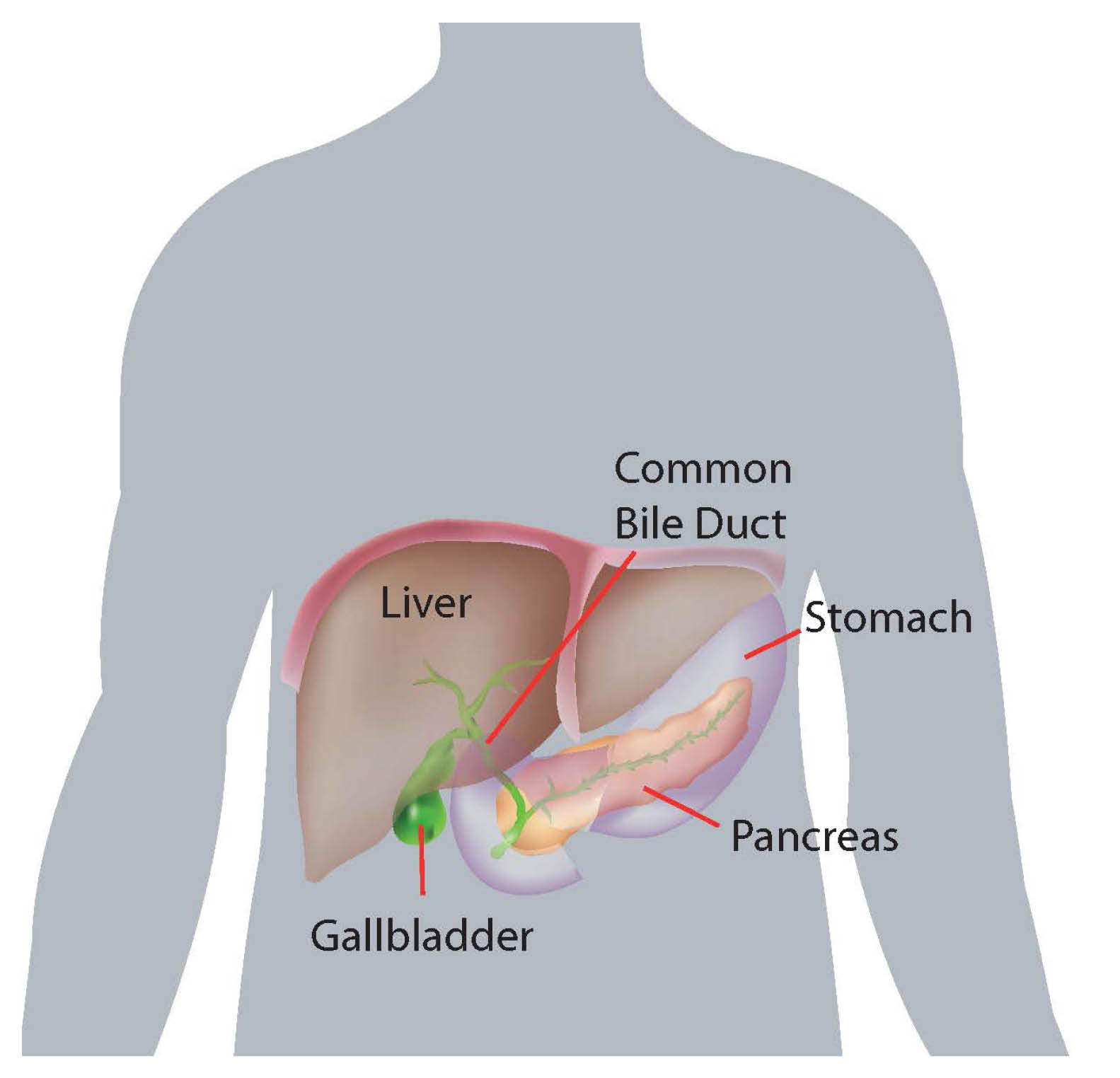
The gallbladder is a muscular storage bag roughly the size of a small pear, that is attached to the liver (this is on the upper right side of your tummy, just behind your lower ribs).
What does the gallbladder do?
It acts as a storage tank for bile.
Bile is continuously produced by the liver, from where it travels down a tube (called the common bile duct) into the duodenum (the part of the bowel that food enters once it leaves the stomach).
Bile mixes with food and is needed for the normal digestion of fat. If you have not eaten recently the bile is diverted from the bile duct to the gallbladder, where it is concentrated and becomes thick. The next time you eat, the muscle of your gallbladder wall squeezes the concentrated bile out into the bile duct to travel down into your duodenum.
Why did I get gallstones?
We do not really know the exact cause of gallstones.
They are more common in older people and those with certain other medical conditions, such as Crohn’s Disease. They are also more common in women and seem to run in families.
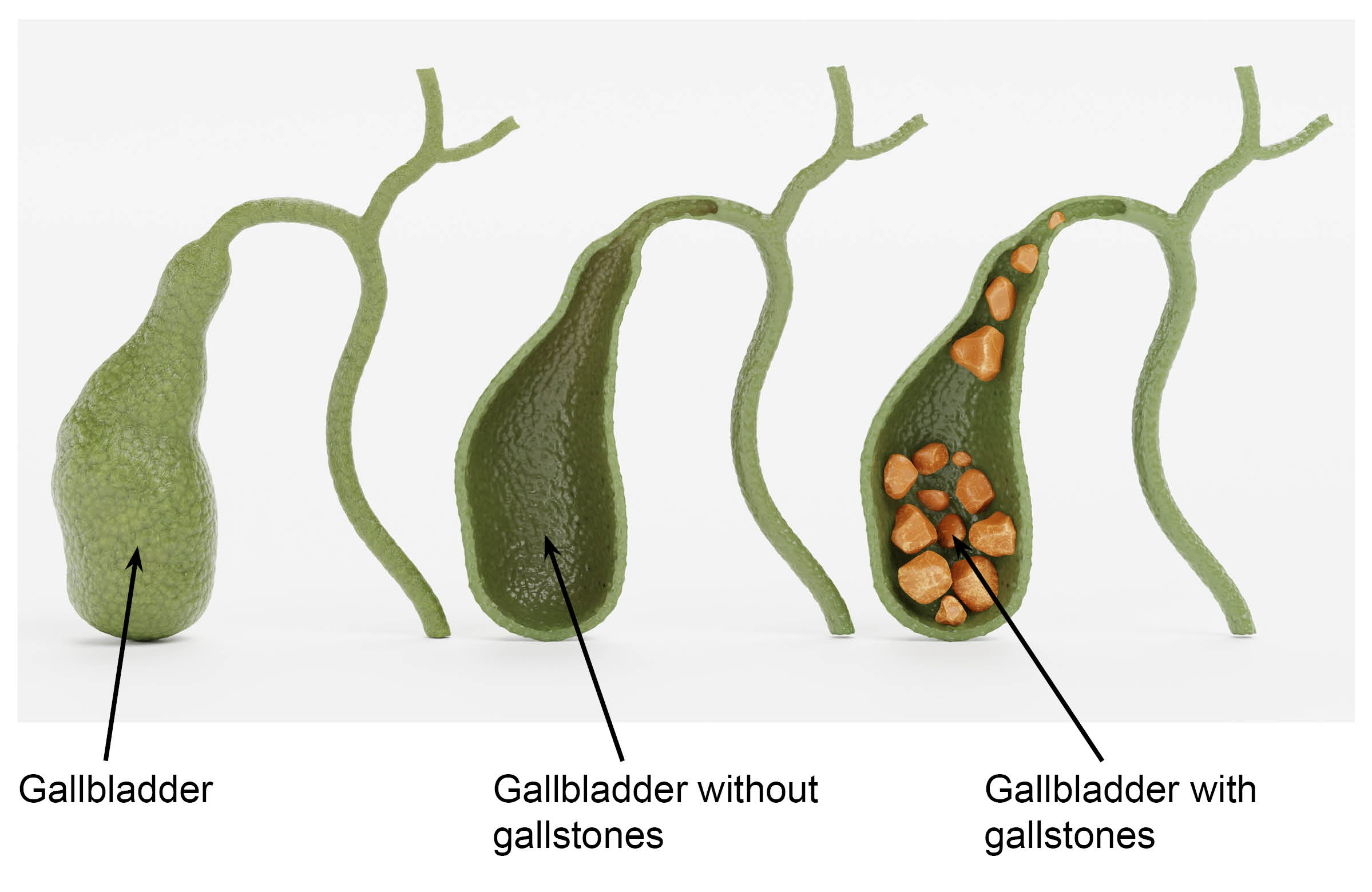
The gallbladder produces thick bile, which settles down as micro crystals and becomes sizable stones. There are many different sizes and shapes of gallstones, ranging from tiny “grains of sand” to a single stone the size of an egg.
Do I have to have my gallbladder removed if I am found to have gallstones?
We do not always recommend surgery to prevent trouble from gallstones. Many people have gallstones and live their entire lives without having symptoms from them. Ten to 15% of the UK adult population have gallstones, and one in five (20%) of them have symptoms due to biliary colic (a recurrent pain in the right side of the abdomen), cholecystitis (inflammation of the gallbladder), jaundice (yellow colouration of the skin and eye), and pancreatitis (inflammation of the pancreas).
Reasons why your surgeon may have advised you to have surgery to remove your gallbladder
If you have symptoms or several stones, as it is safer to remove the gallbladder to avoid any serious complications (such as jaundice or pancreatitis). This can happen in five to 10 of every 100 patients who have gallstones.
If you have a condition such as diabetes or low immunity, or are on medications such as steroids or immune suppressing drugs, you may be advised to have your gallbladder removed for the same reason.
If your gallbladder is showing changes, such as thickening or contracting, as you are at risk of suffering complications.
Surgery is also recommended in some rare patients without gallstones in their gallbladder. In these cases, patients have similar symptoms like gallstone disease but are found not to have stones. Other special tests are performed to identify the diseased gallbladder, and surgery is recommended.
Please discuss your situation with your GP or a specialist.
Can I live normally after having my gallbladder removed?
Yes. Most people notice no difference, other than they no longer get the pain the gallstones were causing. Some patients also find their bowels work more frequently, but this is not often a problem.
The gallstones have usually caused the gallbladder to stop working before it is removed.
Can gallstones be got rid of without surgery?
No. At one time there was an attempt to dissolve gallstones by taking a course of tablets over a period of months, even up to two years. Unfortunately, these tablets caused uncomfortable side effects, which patients found even worse than the symptoms caused by the gallstones. The gallstones also came back within a few months of stopping the tablets.
The next attempt to deal with gallstones without surgery involved shattering the gallstones with ultrasound waves. Unfortunately, the fragments of gallstones either joined back together again or the gallstones became small enough to pass out of the gallbladder into the bile tubes, causing pain and sometimes resulting in jaundice (yellowing of the skin and eyes).
Why do I have to have my gallbladder removed, not just the stones?
A gallbladder which produces stones is a diseased gallbladder. If we only remove the stones, further stones will form very quickly in your gallbladder and your symptoms will return.
How is the gallbladder removed?
This is usually a keyhole surgery called laparoscopic cholecystectomy. This involves making three or four small (up to 1cm) cuts on the front of your tummy, and putting narrow hollow tubes through them. A camera on a telescope and other long thin instruments are put into your tummy through these hollow tubes. This allows your surgeon to see your gallbladder and cut it free of its attachments and remove it.
This operation is still considered by surgeons to be a major surgery despite the small cuts, which are the only visible signs you will have following your operation.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
Are gallbladders only ever removed by keyhole surgery?
No. If you have previously had major surgery to your abdomen, this may have resulted in scar tissue inside your tummy cavity (called adhesions), which can prevent the telescope being able to see your gallbladder clearly. Types of operations that can cause this problem are major bowel surgery, major surgery on the blood vessels in the abdomen, or abdominal surgery done as an emergency (for example following an accident). All these operations leave a long vertical scar on your abdomen.
Smaller operations such as removal of the appendix and operations in the lower abdomen (such as caesarean section or hysterectomy through a “bikini line” scar), rarely prevent successful keyhole surgery on the gallbladder.
The condition of your gallbladder may be the other reason keyhole surgery is impossible. Repeated inflammation and scarring of the gallbladder due to the gallstones can make the gallbladder wall very thick (normally the wall is paper thin), the delicate instruments of keyhole surgery cannot cope with this.
When you sign your consent form for your operation, your surgeon will explain the small risk of having your gallbladder removed with open surgery (a 10 to 20cm cut in the right side of the abdomen) rather than the keyhole surgery.
Apart from the size of the cuts on my tummy, is there any other difference between keyhole and open surgery?
The internal surgery is the same.
The main difference is the amount of discomfort felt. A larger cut will give more discomfort.
Patients having keyhole surgery will usually go home the same day or within 24 to 48 hours of their surgery. The stay is usually longer following an open operation.
Will I be shaved before my surgery?
If your tummy is quite hairy, we will shave part of it. This is so we can remove your wound dressings with little discomfort after your surgery. A small area on your thigh will also be shaved, so we can use electrical cautery to seal blood vessels during your operation. Any shaving is done when you are asleep in the operating theatre, with single use blade surgical clippers.
When can I go home after my operation?
Before going home, you should have fully recovered from the anaesthetic and had a drink and a light meal. You should also have passed water and walked about comfortably without support.
Will I be in pain after my operation?
Most people will need painkillers after their operation. If you have had keyhole surgery you usually only need to take painkillers for a few days after your surgery. However, you may need to take them for longer if you have had open surgery.
What will I be able to do when I go home?
It is normal to feel tired and a bit sore for several days following surgery. With keyhole surgery patients often feel pain in their shoulders and their appetite may be poor to begin with. It is better to eat light meals for the first few days, and avoid drinking alcohol while taking painkillers stronger than paracetamol.
Your tummy may appear a bit swollen for a week or so. You may also find your bowels are constipated. This is the result of missing normal meals around the time of your surgery or can be the effect of the painkillers. This normally settles by itself, but if it doesn’t a gentle laxative from the chemist will be helpful.
You should walk about your house or garden during waking hours, to keep the blood circulating in your legs and reduce the chance of blood clots forming (known as deep vein thrombosis or DVT).
Younger people will return to normal sooner than older people following surgery.
Recovery will be quicker if you had a planned operation rather than if you had your gallbladder removed as an emergency.
How do I look after my wounds after I go home?
Before you leave hospital the nurses will give you detailed instructions on how to look after your wound at home.
If you had keyhole surgery, most wounds will have dissolvable stitches (they do not need to be taken out) covered with small dressings.
You should keep your wounds dry for 48 hours after surgery, after this time you can have a shower.
Your wound may weep, but this should stop by day five. Your wound needs to be checked by your GP practice nurse if it continues to weep after five days. Normal weeping is either clear or bloodstained fluid. If the fluid becomes thick and yellowish / greenish this may mean you have a wound infection. You should see your GP practice nurse within 24 hours of noticing this.
If you had an open operation, then you will have a 10 to 20cm wound, which may have stitches or metal clips that need to be removed seven to 10 days after your operation. This will normally be done by your GP practice nurse or district nurse. You will be told by the ward nurses before you leave hospital whether this has already been arranged or whether you need to telephone your GP surgery to arrange this. These large wounds can weep longer and need to be covered for up to four to five days. You may still shower after 48 hours.
After five days you can have a bath (both open and keyhole surgery), as long as your wounds are not weeping.
It is normal for wounds to feel lumpy and tender for several weeks after surgery, with a slight redness along the line of the wound. If the redness spreads more than 1cm from your wound edges then this may be a sign of a wound infection developing, and you must see your GP practice nurse for advice.
When will I be able to go back to work?
This depends on the type of work you do and your surgery (whether keyhole or open). You can return to a desk job a week or two after keyhole surgery or around four weeks after open surgery. A heavy manual job will need a longer time off work, around four weeks for keyhole surgery and eight weeks for open surgery.
When can I drive again?
You can start to drive once you can comfortably perform an emergency stop and turn around to safely reverse your car. We usually recommend not driving for three or four days after keyhole surgery and around ten days for open surgery.
What are the complications of this surgery?
General risks for any operations
One in five patients will develop a wound infection, usually after they get home. The signs are significant discomfort / pain in relation to the wound, more discharge than usual, and / or feeling unwell with a temperature. If you have these symptoms, you will need to speak to your GP surgery as soon as possible so your wound can be reviewed. If out of hours go to your nearest Emergency Department, if you feel seriously unwell.
It is quite normal to have some bruising around your wounds. Your wounds may ooze a little bit of blood for the first 48 hours, needing a change of dressing.
Chest infections are rare for a fit and healthy person. You are at higher risk if you have a lung disease (severe asthma, emphysema, chronic bronchitis) and moderate risk if you are overweight or a smoker.
Internal bleeding can happen in less than one in 10 to one in 20 gallbladder operations. This may mean that you need to have a blood transfusion or a second operation in order to stop the bleeding. The nurses will check your pulse and blood pressure after your operation to see if this is a problem.
Allergic reactions are rare. If you have had a previous bad reaction to an anaesthetic or any medication, you must tell your surgeon or anaesthetist before your operation.
Blood clots in your legs are known as deep vein thrombosis (DVT). This carries the risk of the blood clot moving from your leg up to your lungs (pulmonary embolus), which can be a life-threatening condition. A fit healthy person has a very small risk of DVT. Your risk is higher if you are overweight, a smoker, in poor general health, have difficulty walking, or have had a DVT before. To reduce your chance of developing a DVT you will be encouraged to get out of bed as soon as you have recovered enough from the anaesthetic. You may also be given an injection of a medicine called Clexane, which reduces your chance of developing a large pulmonary embolus. While you are on bed rest, you should exercise your calf muscles by moving your feet up and down.
Risks specific to a gallbladder operation
Bile may leak inside your abdomen after your gallbladder has been removed. This happens in about one in 50 gallbladder operations and is usually diagnosed in the first few days after your operation. Symptoms include feeling sick all the time, not being able to eat or drink, yellow fluid in your surgical drain (a small plastic tube from the inside of the abdomen through the skin and attached to a bag at your side placed by the surgeon at the time of your operation), or developing jaundice (yellowing of the skin and whites of your eyes and dark coloured urine). A blood test and an ultrasound scan of your abdomen will usually diagnose this problem. If you develop this complication, you will need an ERCP (telescope passed down your throat while sedated) to find the source of the bile leak and to stop it. You may also need further surgery (keyhole or open) to wash out the bile from your abdomen, as bile is an irritant and can cause pain, discomfort, and even infection.
Gallstones in the bile duct. If you have very small gallstones, they may slip out of your gallbladder into the main bile passageway while your gallbladder is being removed. This cannot be seen during your operation. If small stones get stuck at the bottom end of the main bile passageway, you will become jaundiced or have similar pain to when you still had a gallbladder. This complication happens in around one in 50 gallbladder operations and can happen days, weeks, or even months after your operation.
Damage to the main bile duct is a serious but rare complication which happens in around one in 200 to one in 500 gallbladder operations. The damage may be seen during your operation and repaired then (this needs open surgery - a large cut) or it may show up in the first few days, weeks, or months after your surgery. It causes symptoms as described above for bile leak or gallstones in the bile passageway. Major surgery is usually needed to deal with all but the slightest damage. You may need to be transferred to another hospital for the surgery.
Damage to the bowel may happen as a result of the hollow tubes being placed in your abdomen or from your bowel being scarred from previous surgery or inflammation. Bowel damage is usually seen at the time of your operation and dealt with by your surgeon. An open operation may be needed if your bowel cannot be repaired by keyhole surgery. Rarely, the bowel damage may not be seen during your operation and a second operation will be needed. If this happens, it will mean that you will have to stay in hospital for longer.
Is it possible to be unfit for gallbladder surgery?
Yes. Some people’s health is too poor to have major surgery. This may be due to a serious heart or lung condition, or other serious health conditions where there is a high risk of dying from surgery. We may decide to have an anaesthetist examine a patient to help us assess their fitness for surgery.
If you still wish to have the operation, you could ask for a second opinion from another surgeon. We will arrange this for you or will ask your GP to arrange this for you.
Can people die having gallbladder surgery?
Yes, but this is rare. Around one person in every 1000 having gallbladder surgery will die, usually of a complication after surgery. Risks are higher if you are elderly or in poor health, than if you are young and fit.
Is there anything that I can do to improve my health before having surgery?
If you are a smoker try to give up smoking as soon as possible (at least six weeks before your surgery), as smoking increases the risk of developing a chest infection after having a general anaesthetic.
For more information and free friendly NHS support to stop smoking in the community, contact One You Kent on 0300 123 1220, or email.
If you are overweight try to lose weight. Your GP surgery may have a practice nurse that can help you with a weight loss diet.
If you are diabetic you need to keep your blood sugar levels in the correct range.
If you have high blood pressure it needs to be well controlled before you can have surgery.
While waiting for surgery, is there anything that I can do to reduce or prevent the attacks of pain?
Yes. You need to be on a low fat diet. This means avoiding foods such as butter, full fat milk, cream, cheese, chocolate, and red meat. You should also avoid oily and fried food. Keeping strictly to this sort of diet will also help you lose weight.
Your GP may have already given you a supply of strong painkillers, should you have another attack of serious pain.
If I have my gallbladder and gallstones taken out will all my symptoms go away?
If your symptoms were due to the gallstones, then your symptoms will stop once you have recovered from your operation.
About one in 20 patients continue to have pain after their gallbladder has been removed. Gallstones are common and you could have other conditions that can cause similar symptoms. If we feel your symptoms may not be due to your gallstones, we will tell you before your operation that we may need you to have other tests.