Hallux Valgus and Lesser toe conditions
Information for patients from Trauma and Orthopaedics (T&O)
You have been given this leaflet because you have a Hallux Valgus or a lesser toe deformity. This leaflet explains:
what Hallux Valgus is
what your treatment options are
what the risks are to having this surgery; and
what happens if you choose not to have treatment.
We hope this leaflet helps to answer some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
What is Hallux Valgus?
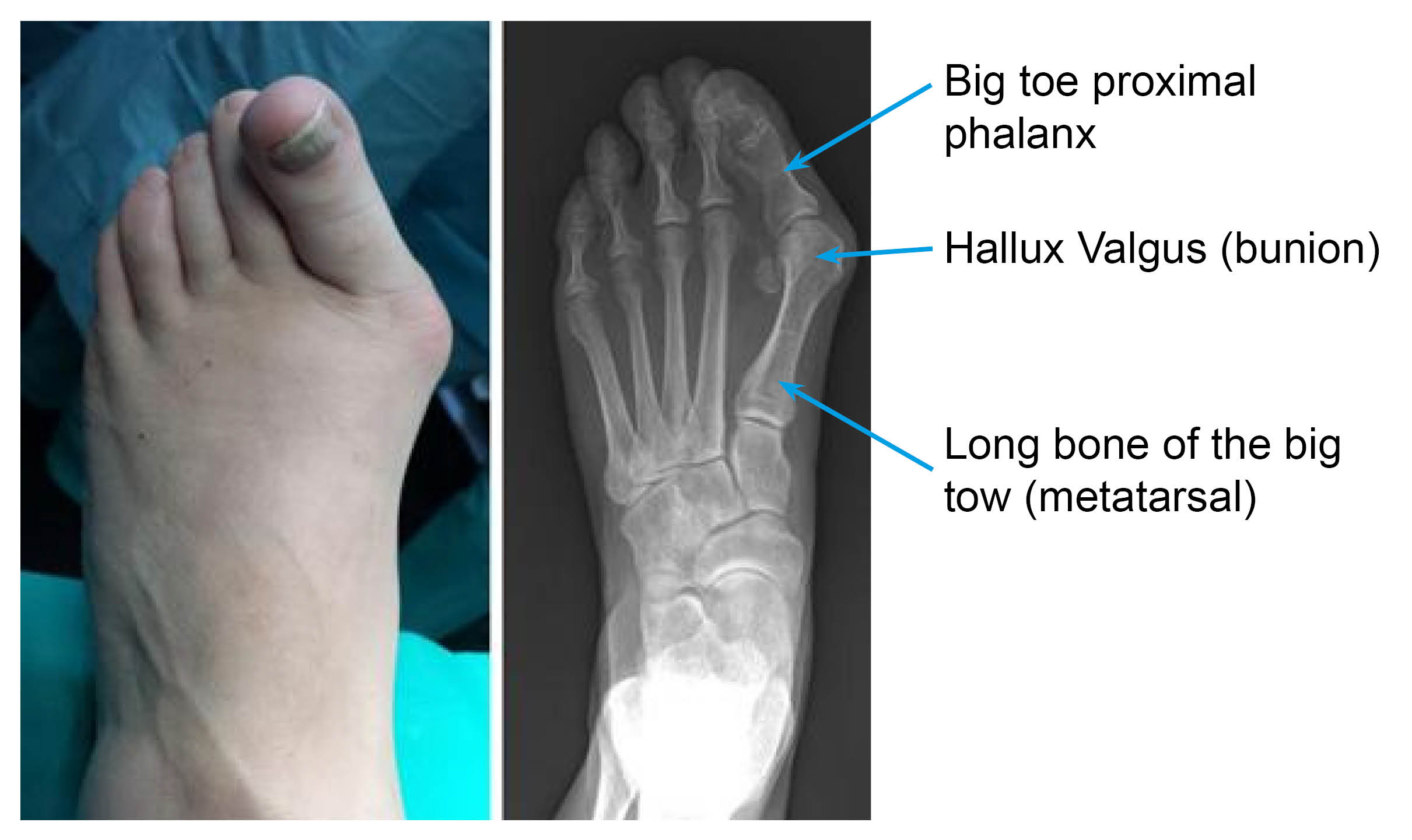
Commonly known as a bunion, this condition is often mistaken as a bony prominence on the big toe. However, Hallux Valgus is a complex deformity. It involves the long bone of the big toe (metatarsal) deviating away from the second toe metatarsal. This causes the soft tissues to work in a different way, and results in the end of the big toe turning towards the second toe.
Patients with this condition, often feel pain when they wear the wrong footwear (usually with a narrow toe box). The pain usually stops when the shoes are removed.
What happens if I ignore the condition?
If you ignore the condition, you may:
develop pain under the balls of your lesser (smaller) toes; or
pain from deformities caused by the big toe squashing the smaller toes.
What are common lesser toe deformities?
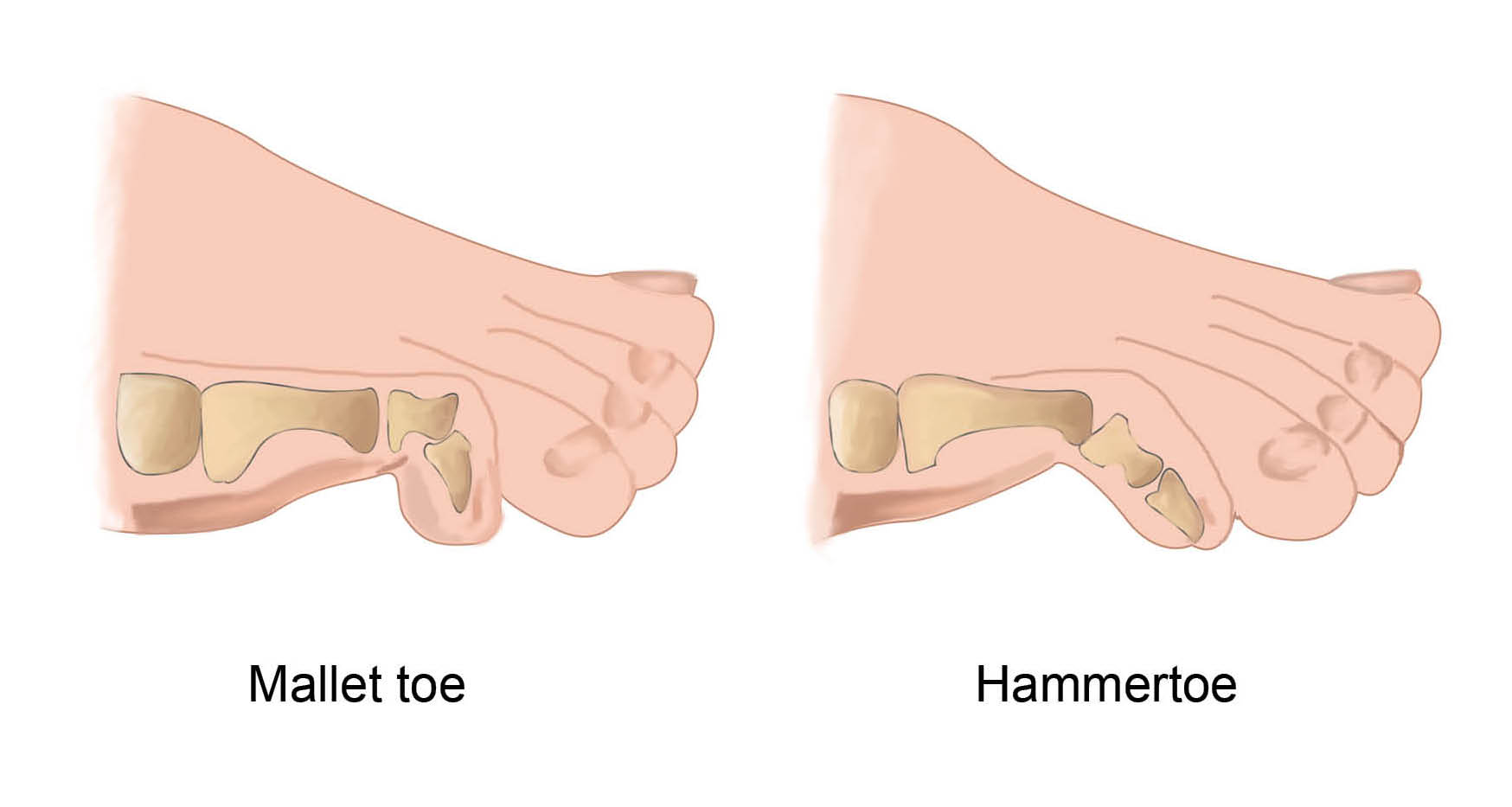
Common lesser toe deformities can be either:
a hammertoe (flexion of the joint closest to the ball of the foot); or
a mallet toe (flexion of the joint near the tip of the toe).
If the toe can be straightened this is flexible. If it cannot be straightened it is a rigid deformity.
When the top of their toes rub in shoes, patients with these deformities often develop pain from friction. This friction often results in a callus (a thickened and hardened part of the skin) forming.
What causes these deformities?
It is not fully understood why these deformities appear. It can be due to:
your choice of foot wear
genetics / family history; or
other foot conditions, such as flat feet or inflammatory joint disease.
Claw lesser toes are often linked with:
neurological disorders, such as Charcot-Marie-Tooth or Polio; or
inflammatory arthropathy (a disease of the joints).
What are the treatments for Hallux Valgus and lesser toe deformities?
Changing foot wear to a soft wider shoe, will give your foot more space. A smaller heel can be of help as well.
Over-the-counter bunion pads / sleeves and spacers can help. Use these with caution though. They can make finding appropriate foot wear more challenging, as they widen your foot.
You should only consider surgery after you have tried the treatments listed above.
What surgical options are available?

Most Hallux Valgus deformities can be managed with surgery.
Surgery can involve breaking the long bone (metatarsal osteotomy) of the big toe and re-positioning it. This will correct the deformity. The bone shift of the metatarsal is then held by a small screw.
Sometimes a break in the bone (proximal phalanx) further along the big toe (akin osteotomy) is needed to complete the correction. This break is held with a small staple or screw. This procedure can be performed through a small incision (cut) on the side of the foot. The cut cannot be seen from the top and fades with time.
If arthritis is present or the deformity is very severe, a fusion procedure may be needed. If you have other lesser toe deformities, your surgeon can perform other procedures at the same time.
For lesser toe deformities:
If the deformity is flexible and related to an elongated metatarsal, the metatarsal can be broken and shortened (osteotomy). This is then held secure with a small screw.
If the metatarsal is not elongated, there are some soft tissue releases that can be done to correct the position of your toe. These include tendon lengthening or tenotomy.
When the deformity is rigid, the affected joint can be excised (cut out) and the joint fused straight. This is held with either:
a Kirschner wire (K-wire) that is removed in clinic after 5 weeks; or
with an implant, that stays within the bone.
You will discuss the above options with your surgeon before any treatment is decided. Your surgeon will discuss which treatment is more appropriate for your condition. You will have an opportunity to ask any questions or raise any concerns you may have.
Will I have a general anaesthetic?
The surgery is normally carried out under general anaesthesia (you will be asleep).
You will be given instructions at your pre-assessment appointment about:
when to stop eating / drinking
what to do with your medications; and
where to come on the day of your surgery.
What happens if I ignore my condition?
The reason(s) why you came to the appointment may not get better, and sometimes can get worse. It is difficult to predict.
How long will I have to stay in hospital?
This surgery is usually performed as a day case procedure (you will able to go home the same day). If you have fusion surgery, you may need to stay in hospital for one night.
You will need someone to drive you home after your surgery, and someone must stay with you overnight.
How can I prepare for my surgery?
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner; and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
What happens when I arrive at the hospital?
When you arrive at the hospital you will be seen by the nurses, a physiotherapist, and doctors who will explain your procedure. Please use this time to ask any questions.
You will be asked to change into a hospital gown and stockings.
How will I feel after surgery?
You will be given painkillers to help with any discomfort after your operation. Everyone reacts to the anaesthetic differently. Feeling sick is common and we do our best to avoid this.
What happens after surgery?

Your foot will be in bandaging.
You will have a surgical shoe, so you can put weight on your affected foot whilst protecting it. Unless you have been told not to by your surgeon.
A member of your healthcare team will give you crutches for support. Please use these as advised by your doctor.
You must elevate (raise) your ankle as much as possible in the first few weeks after your surgery. Move your ankle as much as possible.
What will happen at my follow-up appointments?
Your bandaging will be removed at your 2 week appointment, and your dressings changed.
If you had bunion surgery, at this stage you can start to bend your big toe to help prevent stiffness.
You will need to wear your surgical shoe for weight-bearing for another 5 to 6 weeks.
If a K-wire was used to hold a lesser toe fusion, this will be removed at your 5 week appointment. Your skin will need protecting for a further week, until the site of the K-wire is fully healed.
At 2 weeks, if you have had a soft tissue release for lesser toe deformity surgery and no K-wires were used to hold your toe in place, you can wear comfortable shoes again, but only if your wound has fully healed.
What are the risks?
As with any surgery there are risks. Your surgeon will discuss these with you in more detail before your procedure.
Common complications of this type of surgery include the following.
You can expect swelling for up to 6 months, particularly in the evenings.
You may have stiffness after fusion surgery. If you had a non-fusion procedure, a physiotherapist can show you stretching exercises that can help you avoid stiffness.
A recurrence of the deformity is rare, but can still happen. This may mean you have to have more surgery at a later date.
Overcorrection is also rare, but can be significant. If it does happen you may need further surgery.
Infection rates are low, and antibiotics are given before any surgery. If you do develop an infection, this can cause problems.
A skin infection can be managed with antibiotics.
If you develop a deep infection, we may need to remove all the metalwork and unhealthy bone. You will also need a long course of antibiotics.
Nerve injury can result in numbness or tingling over your toe. If a neuroma (nerve swelling) develops, this can cause pain in your affected toe. This pain is more common after Hallux Valgus surgery.
Non-union can sometimes happen with osteotomy and fusion surgery. Non-union is when the bones do not join together successfully. There is more risk of this happening in smokers. It may result in pain if the metalwork then loosens. If you smoke, stop before surgery and do not start again until the fusion has healed.
If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
Although rare, metalwork can become noticeable through your skin. This can cause pain from irritation. If this continues, we may need to remove the metalwork.
Deep Vein Thrombosis (DVT) / Pulmonary Embolism (PE) is rare with this surgery. Anticoagulation medication is given after surgery, to try to prevent clots forming whilst you are not able to move your leg. This is a preventative measure, but a clot can still form.
If you have any concerns or questions about any of these risks, please speak with your doctor before your surgery.
When can I start my normal activities again?
It should be possible for you to return to impact sports 3 to 6 months after your operation. You can start brisk walking and low impact sport activities earlier.
When can I drive again?
This is a difficult question to answer. Your healthcare professionals are not able to take responsibility for this.
You will need to check with your insurance company as to when they will be willing to insure you to drive again. It is important not to be in a cast or boot when driving, and you must be able to do an emergency stop safely before driving again.
When can I return to work?
When you can return to work depends on the amount of weightbearing needed in your job. If you sit down a lot at work and you can keep your foot elevated, you can return 2 weeks after your operation. Otherwise you should expect to return to work after 6 to 8 weeks.
What if I have any questions or concerns once I return home?
If you have any questions before your surgery, contact the team secretary through the hospital switchboard.
After surgery you can call the team secretary, the ward, or your GP if you have any further concerns or questions. If you have concerns and cannot get in touch with anyone, go to your nearest Emergency Department.
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email